Low Risk Guide - The Alfred Research & Ethics Unit
advertisement

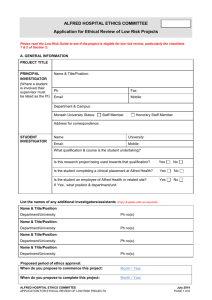
ALFRED HOSPITAL ETHICS COMMITTEE The Low Risk Guide This guide is divided into 4 sections: 1. An overview of the Low Risk ethics review process 2. How to determine whether your activity is suitable for Low Risk review 3. How to complete the Low Risk Application Form 4. How to complete the Biospecimen Addendum Section 1 provides information on what the definition of low risk review is and what the process is for submitting an application. Section 2 provides information on the types of activities that can and cannot be considered for low risk review. It is essential to read this section prior to completing the application form. Section 3 provides further information to assist in completing the application form. Section 4 provides further information to assist in completing the Biospecimen Addendum. SECTION 1: LOW RISK ETHICS REVIEW PROCESS A low risk activity is defined by the National Statement on Ethical Conduct in Human Research (2007) as one where the only foreseeable risk is one of discomfort. Where the risk, even if unlikely, is more serious than discomfort, the research is not low risk. It is important to note that risks include potential risks and not just actual risks, risk is defined by the National Statement and Ethics Committee rather than the clinical context, and that risks are not confined to just physical risks. Low risk review is a process whereby activities that are low risk are reviewed to ensure that issues of an ethical nature are addressed before commencement of the activity. Before considering sending an application in for low risk review it is important that any planned activity that fits into the following three categories, should be directed to the relevant areas first. Nursing related activities (at The Alfred only), including those conducted by nurses, using nursing resources, or involving nurses as research participants, must be assessed by the Nursing Research and Access Committee (NRAC) prior to any submission to the Ethics Committee: http://www.alfredresearch.org/ethics/nursing.htm Activities that involve Caulfield Hospital resources, staff and/or patients, must be authorised by the relevant authority at Caulfield Hospital prior to any submission to the Ethics Committee. Please refer to Section 2 of the Caulfield Hospital Research Governance Authorisation to Conduct Research Guideline for further information (and the corresponding application form ‘Notice of Intention to Conduct Research at Caulfield Hospital’). Both documents can be found on the Alfred Intranet. Go to the ‘Policies & Guidelines’ link and search in Prompt for “Caulfield Research”. Activities generated by external organisations (eg DoH) requiring: help in facilitation, use of multiple departments and/or Alfred Health authorisation, should contact the Clinical Governance Unit of the Alfred Hospital: http://intranet.alfredhealth.org.au/Department.aspx?topicID=1524 The process: 1. Review Checklists 1 & 2 in Section 2 of this Guide to determine if your activity is suitable for low risk review. 2. If your activity is suitable for low risk review, complete the application form and Biospecimen Addendum if applicable. These are located at http://www.alfredresearch.org/ethics/applicat.htm ALFRED HOSPITAL ETHICS COMMITTEE THE LOW RISK GUIDE JUNE 2014 PAGE 1 of 8 It is the responsibility of the investigator designated as the ‘Principal’ investigator to: ensure that the information provided on the form is accurate and sufficiently detailed to enable review. approach the relevant departments for approval to access sources of information and/or biospecimens approach supporting departments for approval to provide the necessary resources (including staff, time, biospecimens/samples, equipment and facilities) inform all those involved in the activity of their responsibilities meet all Alfred Health requirements such as checking the ‘opt-out of research’ list held by HIS prior to contacting patients for participation in research. 3. Email the completed form/s and any relevant documents to research@alfred.org.au In the subject field, type “Project for low risk ethical review”, followed by your last name. Insert signatures electronically, or scan the signed page/s. Please do not send any hard copies. There is no submission date as applications are reviewed on a continual basis. 4. When an application is received, it is checked in order to identify any preliminary issues that need addressing in order to facilitate adequate review. E.g. Failure to attach data collection document. 5. All low risk projects will be allocated a project number. Future correspondence in relation to the project should make reference to this project number. 6. Once the completed application has been submitted, it is reviewed by delegated member/s of the Ethics Committee and/or the Office of Ethics & Research Governance. 7. The Office of Ethics & Research Governance sends an e-mail to the applicant, which either: i) approves the application; or ii) approves the application subject to conditions that need to be met before approval can be granted; or iii) defers the application for further consideration; or iv) declines the application and explains why a full application to the Ethics Committee is required. A requirement of approval is completing a Low Risk Final Report when the project is finished. This is a short form. For projects with a greater-than 12-month duration, an annual summary of progress is required on the anniversary date of approval. The reports can be found on the website on the following page: http://www.alfredresearch.org/ethics/progress.htm scroll to the end to find the Low Risk Final Report. Use the Progress Report for the annual progress update regarding projects which last longer than 12 months. ALFRED HOSPITAL ETHICS COMMITTEE THE LOW RISK GUIDE JUNE 2014 PAGE 2 of 8 SECTION 2: DETERMINING SUITABILITY FOR LOW RISK REVIEW To assist in determining whether the activity is Low Risk read through the various types of activities listed below. CHECKLIST 1 If the project fits into one or more of these categories, it cannot be reviewed through the Low Risk Process and requires a full application http://www.alfredresearch.org/ethics/applicat.htm It is important to note that: -low risk is not defined by what is lower clinical risk in a given medical specialty but by the National Statement and the Ethics Committee. -risk is not just physical but may incorporate social, psychological, financial or cultural risks, or risks such as breach to privacy. 1. ACTIVITIES REQUIRING A FULL ETHICS APPLICATION (not suitable for Low Risk review) Interventions. The research involves providing an intervention. Examples include testing, drugs, surgical procedures, therapeutic procedures, therapeutic devices, preventative procedures, collection of fresh biospecimens from donors where risks associated with collection are more serious than discomfort, diagnostic devices or diagnostic procedures. Vulnerable participants. The project requires obtaining consent from vulnerable people, where competence to provide consent is diminished. Examples include children, ventilated patients, those dependent on care, those with a mental health condition, and cognitively or intellectually impaired persons. Biospecimen (including genetic) research. The project involves research using an individual’s biospecimens where information may be discovered or generated that is of potential importance to the health of the individual, their blood relatives or their community; and/or generates sensitivities for the individual, their family or their community. Human Stem Cells. The research involves studying stem cells or using stem cells or their products to develop new therapies. Pregnancy and the foetus. The research involves the foetus or foetal tissue or has the potential to impact on the wellbeing of the foetus through involvement with a woman/ women who is/are pregnant. External registries. The project involves establishing an external registry where external is defined as one or more of the following: non-Alfred Health custodian, data contribution by other institutions to an Alfred Health registry, data access and use granted to researchers from outside Alfred Health. External researchers. The research is being conducted by a person not associated with the institution and there is no one on the research team from Alfred Health. External researchers. The research is being conducted by a person not associated with the institution and there is minimal supervision by Alfred Health staff and there is a request for waiving the requirement of obtaining consent to access/collect/use or disclose identifying information and/or biospecimens. Student researchers. The project involves a student, not on placement at Alfred Health, accessing identifiable information and/or biospecimens. External sites. The research involves sites that are not part of Alfred Health, do not have their own Ethics Committee and for which Alfred Health would be required to provide research governance. Examples include private practitioners and their patients. External sites. The research involves external sites with Alfred Health as the coordinating centre, where the external sites require full HREC committee approval. Examples are where cross approval at other institutions will be sought. Illegal Activities. The research intends to study or is likely to discover illegal activity. Examples include questioning about illicit drug use. ALFRED HOSPITAL ETHICS COMMITTEE THE LOW RISK GUIDE JUNE 2014 PAGE 3 of 8 CHECKLIST 2 If the project involves one or more of the activities below, justification will be required in the Low Risk Application (Section B, Question 2) as to why this should be considered low risk. 2. ACTIVITIES REQUIRING JUSTIFICATION (may or may not be suitable for low risk review ) Externally funded research where there is a commercial interest A multi-centre study originating from Alfred Health with Alfred Health as the coordinating centre Data access, collection, use and/or disclosure of identifiable information without participant consent Use of already collected biospecimens without the prior donor consent for research use Transfer of biospecimens to external researchers without donor consent Access/collection/use of sensitive information Access/collection/use of information that has regulatory and/or legal reporting requirements Personally intrusive/confronting or quite inconvenient/embarrassing questioning Providing, or potential to provide, individual health/medical/psychiatric diagnosis Screening for healthy participant inclusion/exclusion Change or withdrawal of services Conflicts of interest or dual researcher-professional roles Research conducted overseas Deception (participants will receive limited or no information about the research at time of recruitment) Participant recruitment/selection via a third party Qualitative research without experience Research involving family members of the patient where participants will recruit family members or where family members may need to help the participant to take part and/or provide extra info, etc. Research involving staff where (a) staff may be identifiable in findings, (b) there is a potential to damage or infringe on the rights of staff, (c) there is the potential to cause distress Participation incentives, prizes or significant payments Research placing researchers/assistants at risk ALFRED HOSPITAL ETHICS COMMITTEE THE LOW RISK GUIDE JUNE 2014 PAGE 4 of 8 SECTION 3: COMPLETING THE LOW RISK FORM All sections of the application must be completed with sufficient detail to allow a clear picture of what the project involves. The principal investigator is responsible for ensuring the accuracy of the information. The form has a considerable number of check or tick boxes. Hover your curser over the appropriate box and double click. A dialogue box will appear: under Default Value click on Checked, then OK. Section A: GENERAL INFORMATION Student researcher When the researcher is a student, their supervisor is the usual person who should be the Principal Investigator (PI). In this case there must be a person from Alfred Health on the research team. Proposed period of ethics approval The proposed period of ethics approval covers the duration of the activity, including the data gathering, write up and submission for publication. For those completing a retrospective review, this is not to be confused with the time period of data collection. Section B: PROJECT DETAILS 4. Selection and Recruitment i) This seeks to find out whether the number is based on convenience, anticipated numbers, the maximum available or a sample size determined by statistical means. ii) If the number of participants/samples in each group being studied is less than the maximum number available, explain how participants and/or their samples will be selected (eg. randomly, consecutively, etc.). iii) This seeks to find out whether the participants and/or their samples are identified from a database search, attendance at clinics or from previous research. iv) This part is only applicable for projects that intend to make contact with participants. In this instance the question seeks to determine if participants will be sent a letter, telephoned, approached at a clinic appointment etc. 5. Risks Risks should include all actual and potential risks. Risks should not be limited to physical risks to participants, but should include where applicable, risks to a participant’s emotional, social, financial, cultural, vocational and professional wellbeing. Risks can also be direct or indirect and encompass broader topics such as risks of civil liability, infringement on people’s rights, employability and professional reputation. Risks are not just to the participant but may also be to others such as carers, family members, health providers and institutions. 7. Likely Impact This relates to the degree of significance of the findings; whether the impact is at a personal/departmental/ hospital/professional/peer level and what that impact may be (eg. further review of processes, changes to guidelines, educational requirements, changes to unit/departmental procedures, treatment changes, development of a larger research project). 12. Human Biospecimens Additional questions need to be answered for research that involves the collection of biospecimens from donors, or the use of already-collected/stored biospecimens. Please also complete the Biospecimen Addendum if applicable. Section C: PRIVACY Note that Privacy questions relating specifically to biospecimens (rather than data) are dealt with in the Biospecimen Addendum. 1. a), b) and c) Access and collection of health information These questions relate to accessing information. Some projects may need to access a database to identify potential participants and then access health information from records kept in the database. Some projects may require accessing patient information kept by the patient’s bedside or in their medical history. All sources of information must be listed in b). 2. a), b) and c) Identifiable information ALFRED HOSPITAL ETHICS COMMITTEE THE LOW RISK GUIDE JUNE 2014 PAGE 5 of 8 What is meant by identifiability of health information? A key issue concerning health information is whether an individual participant in the project could become known from the information gathered, analysed or reported. Data used for projects can be: identifiable re-identifiable or coded non-identified or anonymous. Identifiable data: Data that allows a specific individual to be identified. Identifiers may include the individual’s name, date of birth, UR or HRN number. An example is a hospital medical record. In particularly small sets of data, even information such as a postcode may be an identifier. Coded or re-identifiable Information: Coding is replacing identifiable data with an arbitrary code number. For example: Names & UR numbers can be replaced with a study code and the Principal Investigator or Head of Department could keep a separate document which has the identifying information along with the study codes which were assigned, so that if re-identification is required – to check something at a later date – then it can be done. Dates of birth can be replaced with age at a particular cut-off point such as time of diagnosis or admission. It is important to note that data can still be potentially ‘identifiable’ if it is possible to infer an individual’s identity from it (eg asking a hospital employee for work discipline or seniority grade, if they are the only ones working in that area). Non-identified data (anonymised, anonymous, unlinked, not re-identifiable): Data that have been collected without personal identifiers and from which no individual can be identified. It should be pointed out that the term ‘de-identified’ is used frequently to refer to sets of data from which only names or partial identifiers have been removed; (such data may remain ‘potentially identifiable’ and is therefore not non-identified data). Example of how many projects deal with privacy: It is possible that projects may involve more than one of the above. For example a clinician may access identifiable medical records, collect re-identifiable data by using a study code for each patient and keeping a separate log of the study code against the UR number and then provide only the coded data set to a student on clinical placement, so the student only has re-identifiable data to work with. Note: Linking of data sources requires identification. Human biospecimens are considered identifiable or potentially identifiable. Web-based surveys may collect ‘identifiable’ data if recording the IP address. 3. a). The response must include all forms of data; electronic, multi-media and paper based information. ‘Where’ should cover aspects such as locked rooms, locked filing cabinets and password protected drives and also include the physical location eg particular unit’s office. 3. e). Alfred Health requires most low risk project data to be stored for 7 years. There may be instances where data is kept for a different time period and if this is the case, then an explanation for the difference should be provided. Section D: CONSENT For any research project, including low risk projects, it is expected that informed consent will be obtained from participants where it is practicable to do so. If, in a previous related research project, participants consented to their information being used in a future project, details of that project and a copy of the consent form must accompany this new application. A waiver of the requirement to obtain consent may be requested and granted if certain conditions exist. The granting of a ‘consent waiver’ is based on provisions in the Health Records Act 2001 (Vic), Privacy Act (1988), and the National Statement on Ethical Conduct in Human Research (2007). The following items must be addressed when requesting a waiver. involvement in the research carries no more than low risk to participants; the benefits from the research justify any risks of harm associated with not seeking consent; it is impracticable to obtain consent (for example, due to the quantity, age or accessibility of records); ALFRED HOSPITAL ETHICS COMMITTEE THE LOW RISK GUIDE JUNE 2014 PAGE 6 of 8 there is no known or likely reason for thinking that participants would not have consented if they had been asked; there is sufficient protection of the participants’ privacy; there is an adequate plan to protect the confidentiality of data; in a case where the results have significance for the participants’ welfare there is, where practicable, a plan for making information arising from the research available to them (for example, via a disease-specific website or regional news media); the possibility of commercial exploitation of derivatives of the data or biospecimens will not deprive the participants of any financial benefits to which they would be entitled; the waiver is not prohibited by State, federal, or international law. For projects using non-identifiable data, please see Section C: PRIVACY, 2. a), b) and c) Identifiable information (above) for the definition. Where data has been supplied completely devoid of identifiers, from a registry or database, participants’ consent will not be required. However the Ethics Committee will need to be satisfied with the explanation in the application. When considering projects that involve the use or disclosure of information for a ‘secondary purpose’ there are key requirements that must be addressed in keeping with the Health Records Act 2001 (Vic), Health Privacy Principle 2.2 and (in some cases) the Privacy Act (1988). If a project meets one or more of the ‘secondary purposes’ described in HPP2.2(f) then consent for use of the information may not be required. An explanation of how the project meets these requirements must be provided. Consent for Biospecimen Collection Consent for the collection of biospecimens for research directly from participants (e.g. taking a small blood sample) can be addressed in this section of the main Low Risk Form. If the research involves the collection of biospecimens directly from the research participants, participant consent must be obtained. This would typically be done using a Participant Information & Consent Form (PICF). The Biospecimen Addendum, Q.6, includes a Checklist of information that must be covered in the PICF. For projects that involve only already-collected/stored biospecimens, questions relating to consent need to be answered in the Biospecimen Addendum. SECTION E: SIGNATURES A proper review can only be done if researchers provide complete and accurate information. Researchers, when signing their declaration, attest, amongst other things, that this is the case. The Head of Department, in signing the Statement, attests that the research project and its conduct conform to the relevant ethical and research standards. In addition, the Head of Department can make a comment on the points on which he/she has signed off. The signatures can be attached electronically or can be scanned once the paper copy has been signed. SECTION F: APPLICATION CHECKLIST Tick off all the relevant accompanying documents and remember to attach them all as separate documents (not joined into one PDF), along with your completed application, to your covering email to the Ethics Office: research@alfred.org.au The Ethics Office is paperless, so all applications and accompanying documents must be sent electronically. If you do not have access to a scanner for signatures pages, the Ethics Office can help. ALFRED HOSPITAL ETHICS COMMITTEE THE LOW RISK GUIDE JUNE 2014 PAGE 7 of 8 SECTION 4: COMPLETING THE BIOSPECIMEN ADDENDUM TO THE LOW RISK FORM 1(c). In accordance with the National Statement [3.4.14], where it cannot be established that biospecimens were obtained in a manner consistent with the requirements of the National Statement and relevant Australian legislation they should not be used for research in Australia. 7. ‘Pre-existing’/prior consent for research use should be demonstrated by provision of the relevant documentation, such as a copy of the consent form. Where the biospecimens are identifiable and consent is not being sought, a consent waiver must be requested addressing the relevant criteria in the National Statement [2.3.6 & 3.4.12] If, at the time of collection, donors were given an opportunity to express their wishes about the future use of their biospecimens the research must include a process to check what these wishes were. For example, when patients undergo surgery at Alfred Health, the Surgical Consent Form that they must sign includes a clause permitting tissue removed during the procedure to be kept for ethically approved research. Patients are instructed to strike this through if they do not agree. There is an obligation for researchers to check the medical record to ensure that the patient did not exercise this option to decline. The last option in this Consent section pertains to biospecimens that can be obtained and used for the research in an essentially anonymous way (in a sense, they are like a pre-existing collection of nonidentifiable data). 9. A Materials Transfer Agreement (MTA) is a contract governing the exchange of materials between two organisations, usually for research purposes. A MTA should be used for transfer of biospecimens. There are two types of MTAs: incoming and outgoing. An outgoing MTA is used when Alfred Health is providing materials to an external organisation. There is a template for an outgoing MTA at http://www.alfredresearch.org/ethics/legal.htm An incoming MTA is provided by the relevant institution to an Alfred Health researcher requesting materials from an external source. 10. Managers of Alfred Health departments providing resources or services must complete and sign this section of the form. ALFRED HOSPITAL ETHICS COMMITTEE THE LOW RISK GUIDE JUNE 2014 PAGE 8 of 8