a case of congenital lobar emphysema: challenges in diagnosis and
advertisement
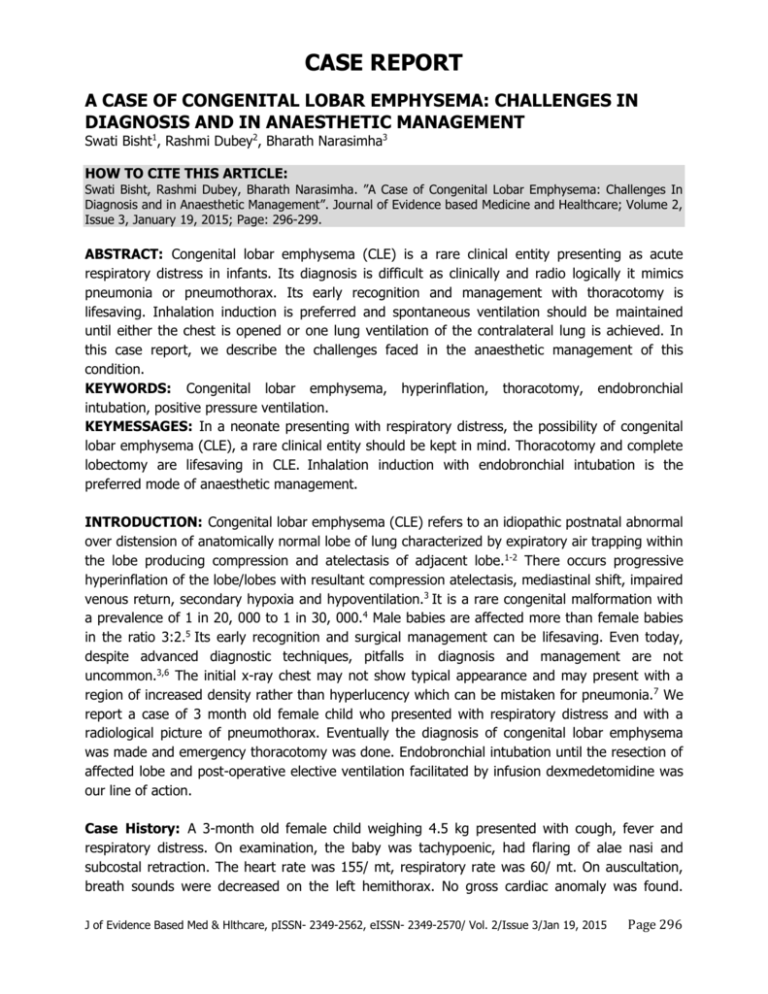
CASE REPORT A CASE OF CONGENITAL LOBAR EMPHYSEMA: CHALLENGES IN DIAGNOSIS AND IN ANAESTHETIC MANAGEMENT Swati Bisht1, Rashmi Dubey2, Bharath Narasimha3 HOW TO CITE THIS ARTICLE: Swati Bisht, Rashmi Dubey, Bharath Narasimha. ”A Case of Congenital Lobar Emphysema: Challenges In Diagnosis and in Anaesthetic Management”. Journal of Evidence based Medicine and Healthcare; Volume 2, Issue 3, January 19, 2015; Page: 296-299. ABSTRACT: Congenital lobar emphysema (CLE) is a rare clinical entity presenting as acute respiratory distress in infants. Its diagnosis is difficult as clinically and radio logically it mimics pneumonia or pneumothorax. Its early recognition and management with thoracotomy is lifesaving. Inhalation induction is preferred and spontaneous ventilation should be maintained until either the chest is opened or one lung ventilation of the contralateral lung is achieved. In this case report, we describe the challenges faced in the anaesthetic management of this condition. KEYWORDS: Congenital lobar emphysema, hyperinflation, thoracotomy, endobronchial intubation, positive pressure ventilation. KEYMESSAGES: In a neonate presenting with respiratory distress, the possibility of congenital lobar emphysema (CLE), a rare clinical entity should be kept in mind. Thoracotomy and complete lobectomy are lifesaving in CLE. Inhalation induction with endobronchial intubation is the preferred mode of anaesthetic management. INTRODUCTION: Congenital lobar emphysema (CLE) refers to an idiopathic postnatal abnormal over distension of anatomically normal lobe of lung characterized by expiratory air trapping within the lobe producing compression and atelectasis of adjacent lobe.1-2 There occurs progressive hyperinflation of the lobe/lobes with resultant compression atelectasis, mediastinal shift, impaired venous return, secondary hypoxia and hypoventilation.3 It is a rare congenital malformation with a prevalence of 1 in 20, 000 to 1 in 30, 000.4 Male babies are affected more than female babies in the ratio 3:2.5 Its early recognition and surgical management can be lifesaving. Even today, despite advanced diagnostic techniques, pitfalls in diagnosis and management are not uncommon.3,6 The initial x-ray chest may not show typical appearance and may present with a region of increased density rather than hyperlucency which can be mistaken for pneumonia.7 We report a case of 3 month old female child who presented with respiratory distress and with a radiological picture of pneumothorax. Eventually the diagnosis of congenital lobar emphysema was made and emergency thoracotomy was done. Endobronchial intubation until the resection of affected lobe and post-operative elective ventilation facilitated by infusion dexmedetomidine was our line of action. Case History: A 3-month old female child weighing 4.5 kg presented with cough, fever and respiratory distress. On examination, the baby was tachypoenic, had flaring of alae nasi and subcostal retraction. The heart rate was 155/ mt, respiratory rate was 60/ mt. On auscultation, breath sounds were decreased on the left hemithorax. No gross cardiac anomaly was found. J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 3/Jan 19, 2015 Page 296 CASE REPORT Oxygen saturation was 85 % with oxygen hood, but there was no visible cyanosis. An x-ray chest revealed hyper inflated left lung with mediastinal shift to the right side. (Figure 1- Initial x-ray) Fluid resuscitation was commenced with 5% Dextrose in normal saline at the rate of 10 ml/ kg/ hour. A provisional diagnosis of left pneumothorax was made and the child put on IV antibiotics, intermittent asthalin nebulization, oxygen via hood and intercostal chest drainage was inserted. Minimal air was drained, but the distress continued. Senior consultant reviewed the x ray and the diagnosis of CLE was considered. (Figure 2- x-ray after ICD insertion) A CT thorax was done immediately. It showed a hyper inflated left upper lobe, and collapse of left lower lobe and right lung, confirming CLE. Routine hematological studies, biochemical parameters were normal. The child was posted for emergency thoracotomy; left upper lobectomy. The child was posted under ASA III E. In OT, ECG, oxygen saturation, temperature monitor, NIBP monitors were connected. Standard precautions to avoid hypothermia were undertaken. A surgeon was scrubbed for an emergency thoracostomy if required. The child was premedicated with Inj atropine 0.03 mg IV, Inj. fentanyl 10 mcg IV. Induction was done by a face mask with 100% oxygen and sevoflurane 4-6 % with Jackson Rees circuit. After adequate depth, 4 mm endotracheal tube was inserted endobronchially into the right lung and confirmed by auscultation. Gentle assisted ventilation was done with hand. Baby was placed in the right lateral position and anaesthesia was maintained with sevoflurane 2-3 % in 100% oxygen. Peak airway pressure was maintained at 20- 25 cm H2O. Following thoracotomy, Inj. Atracurium 2.5 mg IV was administered. Left upper lobectomy was performed with stable haemodynamic vitals. Then bilateral lung ventilation using N2O was commenced after pulling out the endotracheal tube into the trachea. This was confirmed by seeing the expansion of the left lower lobe. Blood and fluid loss was monitored and replaced with 120 ml warmed ringer lactate and 20 ml fresh whole blood. At the end of surgery intercostal block was given by the surgeon under direct vision using 3 ml of 0.25 % of bupivacaine. The child was electively ventilated on volume control mode in the PICU for 12 hours. Intravenous dexmedetomidine infusion was started at 2.5 mcg/ hour and gradually tapered over. The baby was successfully weaned off and extubated uneventfully. Postoperative x-ray chest showed expansion of both the lungs with no mediastinal shift. Fig. 1 Fig. 2 J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 3/Jan 19, 2015 Page 297 CASE REPORT DISCUSSION: CLE usually presents in full term infants between the newborn period and six month of age. In 50 % cases, the exact etiology is unknown; but in 25% bronchial cartilage dysplasia is postulated.6,7,8 Infants with congenital lobar emphysema present a diagnostic challenge. The clinical picture in majority is chest retraction, tachypnea, tachycardia. If hypoxemia ensues, the infant may become agitated, anxious and cyanosed. Physical examination shows asymmetric chest expansion, focal hyperresonance and diminished breath sounds over the affected lobe. Chest x-ray typically shows hyperinflation of the involved lobe, atelectasis of adjacent lung, mediastinal shift and flattening of ipsilateral diaphragm.2 This picture is often confused with pneumothorax leading to intercostals chest drain tube insertion. ICD insertion does not help; rather it aggravates the respiratory distress.8 The correct diagnosis depends on a high level of suspicion. Chest radiography is helpful; but not definitive.9,11 The typical appearance is that of pressure expansion of a lobe of lung causing compression of adjacent lobe. A careful examination of the x-ray film by trans illumination and observing the broncho vascular markings in the hyper inflated lobe can help to differentiate congenital lobar emphysema for pneumothorax.9 CT scan, bronchoscopy and angiography are also helpful in diagnosis.11, 12 Thoracotomy and complete lobectomy are lifesaving in CLE.12 Inhalation induction is preferred and spontaneous ventilation should be maintained until either the chest is opened or one lung ventilation of the contralateral lung is achieved.3 Positive pressure ventilation due to a ball valve effect may cause over distension of emphysematous lobe, worsening of mediastinal shift, reduction of cardiac output and hemodynamic collapse. In case of poor respiratory response, if hypoventilation occurs during induction, gentle assisted manual ventilation may be required. Airway pressure should be maintained at 20-25 cm H2O.3,13 Once chest is opened and affected lobe is delivered, the patient can be paralyzed and controlled ventilation can be initiated.14 Use of N2O before lobectomy should be avoided to prevent hyperinflation of emphysematous lobe.15 If over inflation of the emphysematous lobe occurs during gentle manual ventilation, then emergency thoracostomy and allowing the affected lobe to herniate through the thoracostomy incision will help. One lung ventilation in infants is challenging for anaesthesiologist. Positioning of an endobronchial tube is difficult; also proper size is not available. Reports of endobronchial intubation using single lumen endotracheal tube are described.11 The correct endobronchial placement should be confirmed by fibreoptic bronchoscopy. REFERENCES: 1. Husain A, Kumar V. The Lung. In: Kumar V, Abbas A, Fausto N, editors. Robbins and Cotran Pathologic Basis of Disease, 7 th edition. Philadelphia, Pa; Saunders Elsevier, 2005, Chapter 15. 2. Tempe DK, Virmani S, Javetkar S et al. Congenital lobar emphysema: pitfalls and management. Ann Cardiac Anesth 2010; Vol 13:1. 3. Cote CJ. The anesthetic management of congenital lobar emphysema. Anesthesiology 1978; 49:296-8. 4. Thakral CL, Maji DC, Sajwani MJ. Congenital lobar emphysema: Experience with 21 cases. J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 3/Jan 19, 2015 Page 298 CASE REPORT Pediatr Surg Int.2001; 17: 88-91. [PubMed]. 5. Al- Salem AH, Gyamfi YA, Grant CS. Congenital lobar emphysema. Can J Anaesth 1990; 37: 377-9. 6. Bappal B, Ghani SA, Chaudhary R, Sajvani MJ. Congenital lobar emphysema: A review of 10 cases. Indian J Pediatr 1996; 63:801-8. 7. Franken EA, Buehl I. Infantile lobar emphysema: report of two cases with unusual roentgenographic manifestations. Am J Roentgenol 1966; 98: 354-7. 8. Man DW, Hamdy MH, Henry GM, Bisset WH, Forfar JO. Congenital lobar emphysema: problems in diagnosis and management. Arch Dis Child 1983;58:709-12 9. Guidici R, Leao LE, Moura LA, Wey SB, Ferreira RG, Crott PL. Polyalveolosis: pathogenesis of congenital lobar emphysema? Rev Assoc Bras 1998; 44: 99-105. 10. Gupta R, Singhal SK, Rattan KN, Chhabra B. Management of congenital lobar emphysema with endobronchial intubation and controlled ventilation. Anesth Analg 1998; 86: 71-3. 11. Doull IJ, Connett GJ, Wamer JO. Bronchoscopic appearances of congenital lobar emphysema. Pediatr Pulmonol. 1996; 21:195-7. [PubMed]. 12. Mikhailova V. Congenital lobar emphysema in childhood. Khirurgiia (Sofia) 1996; 49:8-12 [PubMed]. 13. Payne K, Vanzyl W, Richardson M. Anaesthesia for congenital lobar emphysema resection. A case report. S Afr Med J 1984; 66: 421-2. 14. Hatch DJ, Summer E. Anesthesia – Specific conditions. In: Feldman SA, Scurr CF, editors. Current Topics in Anesthesia No 5, Neonatal Anesthesia. 1st ed. London: Edward Arnold Publishers Pvt Ltd; 1981. p.112. 15. Raynor AC, Cap MP, Scaly WC. Lobar emphysema of infancy: diagnosis, treatment and etiology aspects. Ann Thorac Surg. 1996; 4:374- 375. [PubMed]. AUTHORS: 1. Swati Bisht 2. Rashmi Dubey 3. Bharath Narasimha PARTICULARS OF CONTRIBUTORS: 1. Associate Professor, Department of Anaesthesiology, Vydehi Institute of Medical Sciences and Research Centre, Bangalore. 2. Associate Professor, Department of Anaesthesiology, Vydehi Institute of Medical Sciences and Research Centre, Bangalore. 3. Senior Resident, Department of Anaesthesiology, Vydehi Institute of Medical Sciences and Research Centre, Bangalore. NAME ADDRESS EMAIL ID OF THE CORRESPONDING AUTHOR: Dr. Swati Bisht, SG 304, Shriram Spandhana Appts, Challaghatta, Banglaore-560037. E-mail: swati_bisht@hotmail.com Date Date Date Date of of of of Submission: 08/01/2015. Peer Review: 09/01/2015. Acceptance: 10/01/2015. Publishing: 19/01/2015. J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 3/Jan 19, 2015 Page 299