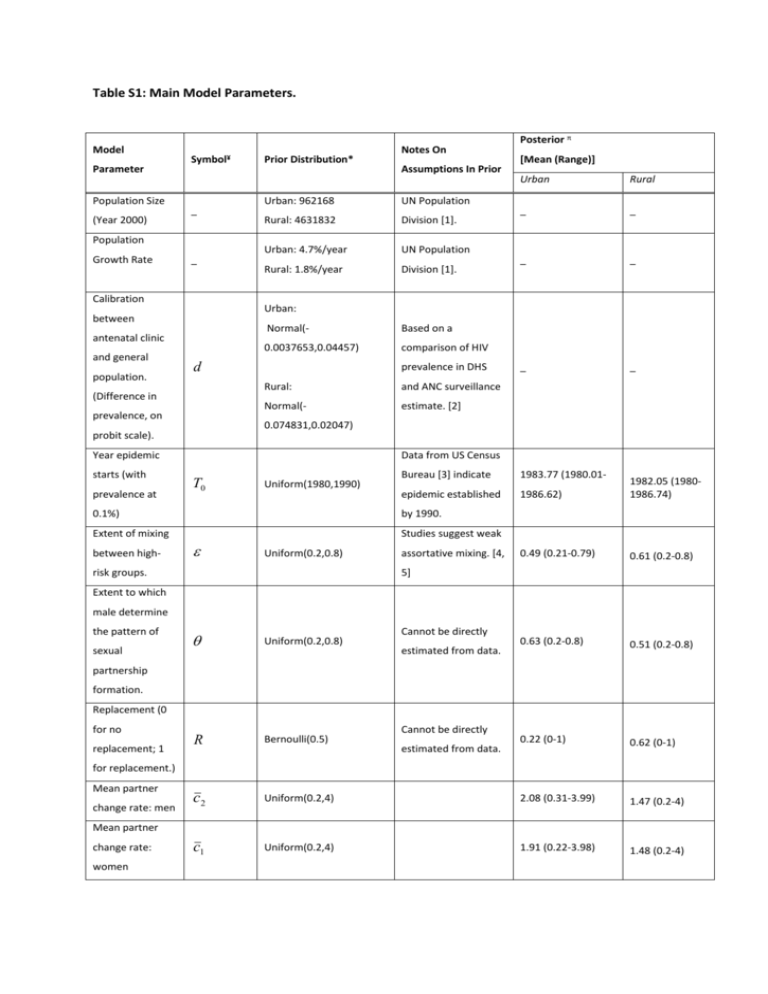
Table S1: Main Model Parameters.
Model
Parameter
Population Size
(Year 2000)
Symbol¥
_
Population
Growth Rate
_
Calibration
antenatal clinic
population.
Urban: 962168
UN Population
Rural: 4631832
Division [1].
Urban: 4.7%/year
UN Population
Rural: 1.8%/year
Division [1].
Normal(-
Based on a
0.0037653,0.04457)
comparison of HIV
d
(Difference in
prevalence, on
prevalence in DHS
Rural:
and ANC surveillance
Normal(-
estimate. [2]
Year epidemic
prevalence at
Urban
Rural
_
_
_
_
_
_
Data from US Census
T0
Uniform(1980,1990)
Bureau [3] indicate
1983.77 (1980.01-
epidemic established
1986.62)
1982.05 (19801986.74)
0.49 (0.21-0.79)
0.61 (0.2-0.8)
0.63 (0.2-0.8)
0.51 (0.2-0.8)
0.22 (0-1)
0.62 (0-1)
0.1%)
by 1990.
Extent of mixing
Studies suggest weak
between high-
[Mean (Range)]
0.074831,0.02047)
probit scale).
starts (with
Assumptions In Prior
Posterior π
Urban:
between
and general
Prior Distribution*
Notes On
Uniform(0.2,0.8)
risk groups.
assortative mixing. [4,
5]
Extent to which
male determine
the pattern of
sexual
Cannot be directly
Uniform(0.2,0.8)
R
Bernoulli(0.5)
c2
Uniform(0.2,4)
2.08 (0.31-3.99)
1.47 (0.2-4)
c1
Uniform(0.2,4)
1.91 (0.22-3.98)
1.48 (0.2-4)
estimated from data.
partnership
formation.
Replacement (0
for no
replacement; 1
Cannot be directly
estimated from data.
for replacement.)
Mean partner
change rate: men
Mean partner
change rate:
women
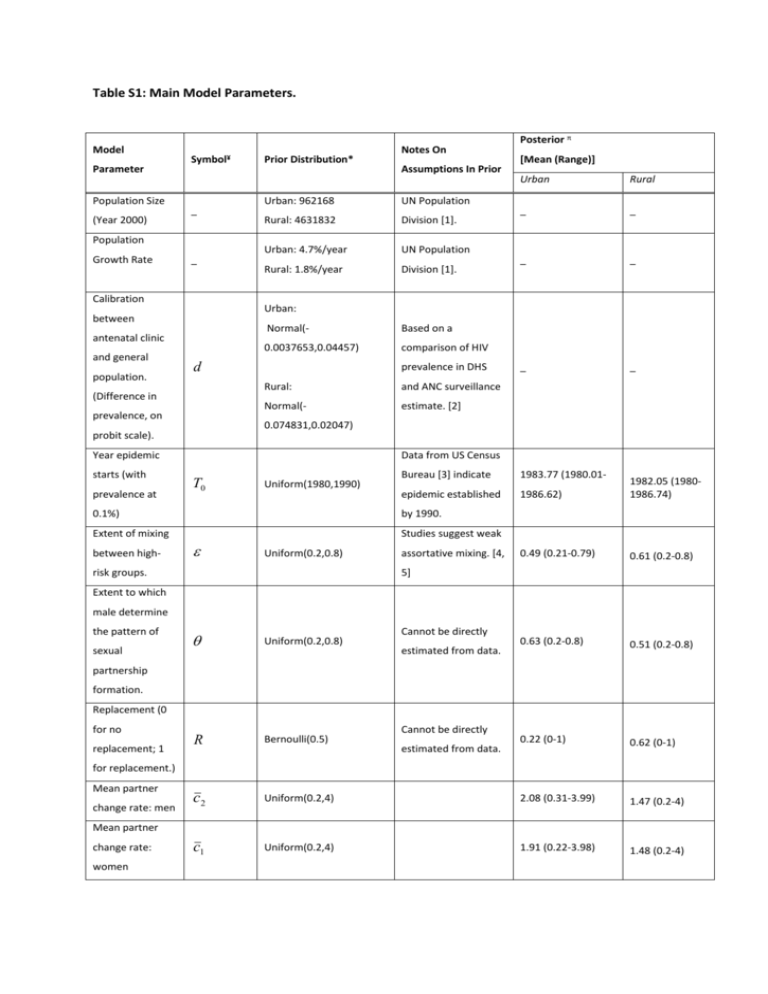
Fraction of men
in high risk
1 2,3
groups (groups I
2,1 2, 2
Uniform(0.05,0.50)
Cannot be directly
estimated from data.
0.42 (0.05-0.5)
0.22 (0.05-0.5)
0.6 (0.2-0.79)
0.46 (0.2-0.8)
0.25 (0.06-0.49)
0.19 (0.05-0.5)
0.46 (0.21-0.8)
0.45 (0.2-0.8)
40.09 (2.2-49.7)
22.92 (2.0249.92)
48.77 (10.69-99.9)
63.07 (10.0199.99)
24.89 (2.17-49.99)
22.84 (2.0249.98)
52.22 (10.09-99.54)
65.98 (10.08100)
0.25 (0.02-0.49)
0.21 (0-0.49)
and II).
Fraction of men
with casual
partners that
have large
2,1 1 2,3
numbers of
Uniform(0.20,0.80)
Cannot be directly
estimated from data.
partners (group I
as a fraction of
groups I and II).
Fraction of
women in high
1 1,3
risk groups
1,1 1, 2
Uniform(0.05,0.50)
Cannot be directly
estimated from data.
(groups I and III).
Fraction of
women with
casual partners
that have large
1,1 1 1,3
numbers of
Uniform(0.20,0.80)
Cannot be directly
estimated from data.
partners (group I
as a fraction of
groups I and II).
Relative rates of
partner change:
group II versus
2, 2
Uniform(2,50)
2,1
Uniform(10,100)
1, 2
Uniform(2,50)
1,1
Uniform(10,100)
Cannot be directly
estimated from data.
group III: men.
Relative rates of
partner change:
group I versus
Cannot be directly
estimated from data.
group III: men.
Relative rates of
partner change:
group II versus
Cannot be directly
estimated from data.
group III: women.
Relative rates of
partner change:
group I versus
Cannot be directly
estimated from data.
group III: women.
Fraction of sex
acts in casual
q1
Triangular(0.1,0.50,0.15)
Modal value based on
point estimate of
partnerships
reported partners in
protected by
last year by men,
condom.
2000 DHS [6].
Number of sex
Limits based on
acts in casual
partnerships per
n1
Uniform(10,80)
reports in
observational cohort
year.
in rural Zimbabwe b.
Number of sex
Limits based on
acts in regular
partnerships per
n2
Uniform(50,300)
Chance of HIV
147.27 (52.46-
observational cohort
298.73)
captures influence of
sex act from
Triangular(0.000666,0.00
2,0.001)
(average value
co-factor STIs as well
0.00118 (0.00069-
and other aspects of
0.00192)
risk not explicitly
0.00114
(0.000680.00197)
captured in the model
for men and
[7].
women).
Relative coital
Cannot be directly
frequency for
estimated from data,
those with
but available data do
symptoms of
131.5 (50.03299.81)
This parameter
transmission per
latent infection
reports in
46.23 (10.0879.94)
in rural Zimbabwe b.
year.
individuals with
50.03 (12.45-79.99)
h
Uniform(0.0,0.5)
suggest reduction in
immune
coital frequency for
suppression
those in stable
versus others. c
partnerships. [7]
0.29 (0-0.5)
0.26 (0-0.5)
0.54 (0.32-0.65)
0.49 (0.31-0.66)
Bbased on observed
survival rate in cohort
studies [8, 9]. Overall
survival time is
manipulated by
changing duration of
Rate of
progression of
_
Uniform(0.313,0.655)
latent infection stage
( 1 3 1 4 1 5 )
HIV.
and stated range
corresponds to net
survival with infection
between 8.5 and 12.5
years.
Year behaviour
change starts
Uniform(2000,2004)
Years of surveys
2000.44 (2000-
between which
2003.25)
-π
behaviour changes
observed.
Years until new
value for
behavioural
F
Uniform(1,5)
Vague prior.
2.39 (1.02-4.94)
-π
1.13 (0.54-1.47)
-π
0.64 (0.52-1.06)
-π
0.84 (0.52-1.33)
-π
0.8 (0.8-0.8)
0.36 (0.12-0.78)
parameters
reached
Modal value based on
point estimate of
Relative change
change in fraction of
in condom use in
casual
partnerships
men and women that
3
Triangular(0.5,1.5,1.23)
used condom in last
sex act with non-
(1=stays the
regular partner,
same)
between the 2004
and 2000 DHS [6, 10].
Modal value based on
point estimate of
change in mean
Relative change
in mean partner
2
Triangular(0.5,1.5,0.62)
change rate: men
numbers of partners
reported by women
in the last year,
between the 2004
and 2000 DHS [6, 10].
Modal value based on
point estimate of
Relative change
in mean partner
change rate:
change in mean
1
Triangular(0.5,1.5,1.00)
numbers of partners
reported by women
women
in the last year,
between the 2004
and 2000 DHS [6, 10].
It is estimated that in
2006, coverage of
treatment (=number
on treatment / total
Rate of scale-up
of access to ART
arate
Triangular(0.11,0.80,0.17
in need of treatment)
7)
was 27% (credible
interval 43-89%)
(based on need at
CD4 cell counts below
200 cells per
microlitre) [11]. In the
model, this
corresponds to the
stated scale-up rates
of access to
treatment; the mode
of the prior is the
estimated value, and
the limits are the
bounds of the
credible interval.
Notes to Table 1:
¥Following
notation in Hallett et al., 2009 [12].
*The distribution as parameterised in the following way: Uniform (lower limit, upper limit); Triangular(lower limit, upper
limit, mode); Normal(mean, standard deviation) (If not parameters specified, a fixed value was assumed).
π:Values reported are the model with behaviour change for Urban population and the model without behaviour change for
the Rural populations (in each case, this is the preferred model).
b: To assess the location and potential ranges for some model parameters, point estimates of behavioural indicators were
calculated for various sub-groups in a population-based study in rural Eastern Zimbabwe conducted 1998-2000 [13]. The
population was divided by sex, age (<20; 20-29; 30-39; 40-49), type of location (estate, subsistence farming area, roadside
trading venue or small town) and church (Traditional, Anglican, Roman Catholic or Other). Sub-groups in which the number
of respondents was less than 10 were ignored. The limits of the prior as the 1st and 99th percentiles across these 128 strata.
c: Individuals with symptoms of immune-suppressions include individuals with pre-AIDS or AIDS.
References
1.
2.
3.
4.
5.
6.
7.
8.
United Nations; Department of Economic and Social Affairs; Population Division. World
Urbanization Prospects: The 2003 revision. In. New York: United Nations; 2004.
Gouws E. Comparison of HIV prevalence in population-based national surveys and ANC
surveillance: Implications for calibrating surveillance data. In: Sex Transm Infect; 2008.
US Census Bureau. HIV/AIDS Surveillance data base. December 2006 release. (available
from: http://www.census.gov/ipc/www/hivaidsd.html) 2006.
Garnett GP, Hughes JP, Anderson RM, Stoner BP, Aral SO, Whittington WL, et al. Sexual
mixing patterns of patients attending sexually transmitted diseases clinics. Sex Transm Dis
1996,23:248-257.
Garnett GP, Anderson RM. Contact tracing and the estimation of sexual mixing patterns: the
epidemiology of gonococcal infections. Sex Transm Dis 1993,20:181-191.
Zimbabwe: DHS, 1999 - Final Report (English).
http://www.measuredhs.com/pubs/pub_details.cfm?ID=296&srchTp=advanced (accessed
10-5-07).
Wawer MJ, Gray RH, Sewankambo NK, Serwadda D, Li X, Laeyendecker O, et al. Rates of HIV1 transmission per coital act, by stage of HIV-1 infection, in Rakai, Uganda. J Infect Dis
2005,191:1403-1409.
Marston M, Todd J, Glynn JR, Nelson K, Rangsin R, Lutalo T, et al. Estimating 'net' HIV-related
mortality and the importance of background mortality rates. AIDS 2007,21:S65-S71.
9.
10.
11.
12.
13.
Todd J, Glynn JR, Marston M, Lutalo T, Biraro S, Mwita W, et al. Time from HIV
seroconversion to death: a collaborative analysis of eight studies in six low and middleincome countries before highly active antiretroviral therapy. AIDS 2007,21:S55-S63.
Gregson S, Nyamukapa C, Lopman B, Mushati P, Garnett GP, Chandiwana SK, et al. Critique
of early models of the demographic impact of HIV/AIDS in sub-Saharan Africa based on
contemporary empirical data from Zimbabwe. Proc Natl Acad Sci U S A 2007,104:1458614591.
World Health Organization, UNAIDS, UNICEF. Towards Universal Access: Scaling up priority
HIV/AIDS interventions in the health sector.
http://www.who.int/hiv/mediacentre/universal_access_progress_report_en.pdf (accessed
30/10/07) 2007.
Hallett TB, Gregson S, Gonese E, Mugurungi O, Garnett GP. Assessing evidence for behaviour
change affecting the course of HIV epidemics: A new mathematical modelling approach and
application to data from Zimbabwe Epidemics 2009,1:108-117
(doi:110.1016/j.epidem.2009.1003.1001).
Gregson S, Nyamukapa CA, Garnett GP, Mason PR, Zhuwau T, Carael M, et al. Sexual mixing
patterns and sex-differentials in teenage exposure to HIV infection in rural Zimbabwe.
Lancet 2002,359:1896-1903.