FAQs: Critical Care 2012 - UC San Diego Health Sciences
advertisement
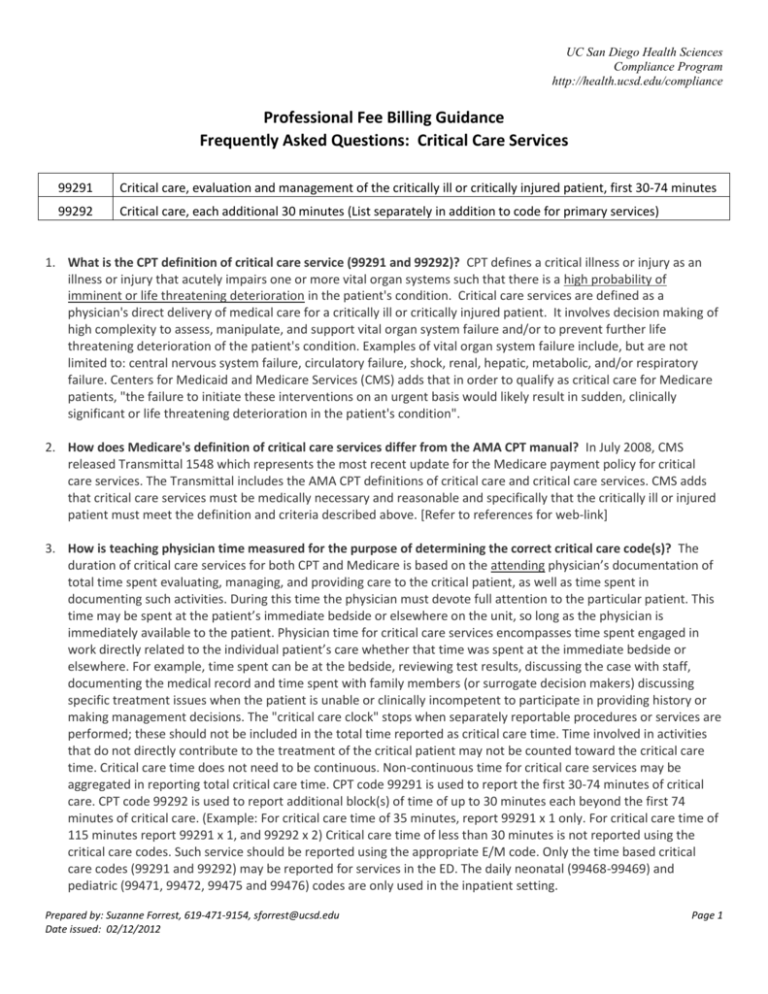
UC San Diego Health Sciences Compliance Program http://health.ucsd.edu/compliance Professional Fee Billing Guidance Frequently Asked Questions: Critical Care Services 99291 Critical care, evaluation and management of the critically ill or critically injured patient, first 30-74 minutes 99292 Critical care, each additional 30 minutes (List separately in addition to code for primary services) 1. What is the CPT definition of critical care service (99291 and 99292)? CPT defines a critical illness or injury as an illness or injury that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life threatening deterioration in the patient's condition. Critical care services are defined as a physician's direct delivery of medical care for a critically ill or critically injured patient. It involves decision making of high complexity to assess, manipulate, and support vital organ system failure and/or to prevent further life threatening deterioration of the patient's condition. Examples of vital organ system failure include, but are not limited to: central nervous system failure, circulatory failure, shock, renal, hepatic, metabolic, and/or respiratory failure. Centers for Medicaid and Medicare Services (CMS) adds that in order to qualify as critical care for Medicare patients, "the failure to initiate these interventions on an urgent basis would likely result in sudden, clinically significant or life threatening deterioration in the patient's condition". 2. How does Medicare's definition of critical care services differ from the AMA CPT manual? In July 2008, CMS released Transmittal 1548 which represents the most recent update for the Medicare payment policy for critical care services. The Transmittal includes the AMA CPT definitions of critical care and critical care services. CMS adds that critical care services must be medically necessary and reasonable and specifically that the critically ill or injured patient must meet the definition and criteria described above. [Refer to references for web-link] 3. How is teaching physician time measured for the purpose of determining the correct critical care code(s)? The duration of critical care services for both CPT and Medicare is based on the attending physician’s documentation of total time spent evaluating, managing, and providing care to the critical patient, as well as time spent in documenting such activities. During this time the physician must devote full attention to the particular patient. This time may be spent at the patient’s immediate bedside or elsewhere on the unit, so long as the physician is immediately available to the patient. Physician time for critical care services encompasses time spent engaged in work directly related to the individual patient’s care whether that time was spent at the immediate bedside or elsewhere. For example, time spent can be at the bedside, reviewing test results, discussing the case with staff, documenting the medical record and time spent with family members (or surrogate decision makers) discussing specific treatment issues when the patient is unable or clinically incompetent to participate in providing history or making management decisions. The "critical care clock" stops when separately reportable procedures or services are performed; these should not be included in the total time reported as critical care time. Time involved in activities that do not directly contribute to the treatment of the critical patient may not be counted toward the critical care time. Critical care time does not need to be continuous. Non-continuous time for critical care services may be aggregated in reporting total critical care time. CPT code 99291 is used to report the first 30-74 minutes of critical care. CPT code 99292 is used to report additional block(s) of time of up to 30 minutes each beyond the first 74 minutes of critical care. (Example: For critical care time of 35 minutes, report 99291 x 1 only. For critical care time of 115 minutes report 99291 x 1, and 99292 x 2) Critical care time of less than 30 minutes is not reported using the critical care codes. Such service should be reported using the appropriate E/M code. Only the time based critical care codes (99291 and 99292) may be reported for services in the ED. The daily neonatal (99468-99469) and pediatric (99471, 99472, 99475 and 99476) codes are only used in the inpatient setting. Prepared by: Suzanne Forrest, 619-471-9154, sforrest@ucsd.edu Date issued: 02/12/2012 Page 1 UC San Diego Health Sciences Compliance Program http://health.ucsd.edu/compliance 4. What are the key documentation requirements for use of the critical care service codes 99291 and 99292? Providing medical care to the critical patient qualifies as a critical care service only if both the illness or injury and the treatment being provided meet the above requirements. The attending physician’s medical record documentation must provide substantive information: a. The patient’s condition must meet the definition of a critical illness or injury described above. b. The total critical care time delivered must be documented and must be a minimum of 30 minutes, exclusive of separately reportable procedure time(s). c. Clinical reassessments and documentation must support the amount of critical care time aggregated and should include a description of all of the physician's interval assessments of the patient's condition, any "impairments of organ systems" based on all relevant data available to the physician (i.e., symptoms, signs and diagnostic data), the rationale and timing of interventions and the patient's response to treatment. d. It is recommended that the physician note that "time involved in the performance of separately reportable procedures was not counted toward critical care time". Failure to do so might result in the critical care time being reduced by payers to account for any concurrent separately billable services. 5. What are the key performance and documentation requirements for use of the critical care service codes with regard to Medicare’s Teaching Physician criteria? Time spent alone by the resident (i.e., performing critical care activities in the absence of the teaching physician) cannot be counted toward critical care time. Only time spent performing critical care activities by the resident and the teaching physician together or the teaching physician alone can be counted toward critical care time. The teaching physician may tie into the resident’s documentation and may refer to the resident’s documentation for specific patient history, physical findings and medical assessment. However, the teaching physician must still document a statement of the total time the teaching physician personally spent providing critical care, that the patient was critically ill when the teaching physician saw the patient, what made the patient critically ill, and the nature of the treatment and management provided by the teaching physician. a. Example of unacceptable teaching physician documentation: “I came and saw (the patient) and agree with (the resident)”. b. Example of acceptable teaching physician documentation: "Patient developed hypotension and hypoxia. I spent 45 minutes while the patient was in this condition, providing fluids, pressor drugs, and oxygen. I reviewed the resident's documentation and I agree with the resident's assessment and plan of care." 6. Can a critical care service code be reported with an E/M code for a patient cared for by the same physician on the same calendar day? Yes! CPT allows for reporting both an E/M service and a critical care service on the same day. Additionally, CPT does not distinguish as to site of service or which service comes first. Some payers may require the modifier -25 to be attached to the non-critical care EM service (see below). 7. Can a critical care service code be reported with an E/M code for a Medicare patient cared for by the same physician on the same calendar day? CMS Transmittal 1548 specifically addresses this question with regard to the emergency department. It states that when critical care services are required upon arrival into the emergency department, only critical care codes (99291 - 99292) may be reported. An emergency department E/M code (9928199285) may not also be reported (by the same physician). Although CMS understands that a patient may need critical care services on the same day where the patient may have only required an inpatient or office/outpatient E/M service earlier in the day, Transmittal 1548 clearly states that hospital emergency department services are not payable for the same calendar date as critical care services when provided by the same physician (which includes any physician of the same specialty in the same group) to the same patient. In other words, if a Medicare patient presents to the emergency department and receives a Level 5 ED E/M workup, and later in the shift unexpectedly Prepared by: Suzanne Forrest, 619-471-9154, sforrest@ucsd.edu Date issued: 02/12/2012 Page 2 UC San Diego Health Sciences Compliance Program http://health.ucsd.edu/compliance clinically deteriorates requiring critical care services, according to CMS the "same" ED physician can only report either the ED E/M service or the critical care service -- but not both. 8. According to CPT which procedure codes are considered to be bundled into the critical care code? The following services are included in "critical care” clock time when performed during the critical period by the same physician(s) providing critical care and should not be reported separately. Any services performed that are not listed below may be reported separately. : a. Interpretation of cardiac output measurements (CPT 93561, 93562) b. Pulse oximetry (CPT 94760, 94761, 94762) c. Chest x-rays, professional component (CPT 71010, 71015, 71020) d. Blood gases and information data stored in computers (e.g., ECGs, blood pressures, hematologic data, CPT 99090) e. Gastric intubation (CPT 43752, 91105) f. Transcutaneous pacing (CPT 92953) g. Ventilator management (CPT 94002-94004, 94660, 94662) h. Vascular access procedures (CPT 36000, 36410, 36415, 36591, 36600) 9. Does Medicare differ from CPT in the way it addresses bundling of critical care services and procedures? Medicare bundles the same services included in critical care by CPT (see FAQs #7 & #8 above) when performed by the same physician(s) reporting critical care. However, Medicare differs in that the relevant time frame for bundling pertains to the entire calendar day for which critical care is reported, rather than limiting the time frame to just the period of time that the patient is critically ill or injured during that calendar day. 10. What are some examples of procedures that could be billed separately from critical care? The "critical care clock" stops when performing non-bundled, separately billable procedures. Examples of common procedures that may be performed for a critically ill or injured patient include (but not limited to): a. CPR (92950) (while being performed) b. Endotracheal intubation (31500) c. Central line placement (36555, 36556) d. Intraosseous placement (36680) e. Tube thoracostomy (32551) f. Temporary transvenous pacemaker (33210) g. Electrocardiogram - routine ECG with at least 12 leads; interpretation and report only (93010) h. This is not an exhaustive list of possible separately billable procedures, but only serves as an example that could be report. 11. What is the appropriate use of modifier -25 when billing for critical care services and separately billable services or procedures? CPT does not require the use of modifier -25 when billing for critical care services and separately billable (i.e., non-bundled) procedures. However, critical care services provided to a patient may not be paid by some payers (e.g., Medicare) on the same day the physician also bills a non-bundled procedure code(s) unless critical care is billed with the CPT modifier -25 to indicate that the critical care is "a significant, separately identifiable E/M service above and beyond the other service provided or beyond the usual preoperative care associated with the procedure that was performed." For such payers, when services such as endotracheal intubation (CPT code 31500) and CPR (CPT code 92950) are provided, separate payment may be made for critical care in addition to these services, if the critical care was a significant separately identifiable service and it was reported with modifier -25. The Prepared by: Suzanne Forrest, 619-471-9154, sforrest@ucsd.edu Date issued: 02/12/2012 Page 3 UC San Diego Health Sciences Compliance Program http://health.ucsd.edu/compliance time spent performing the pre, intra, and post procedure work of these unbundled services is excluded from the determination of the time spent providing critical care. 12. Ventilator Management & Critical Care Services: Not billable on the same day! Medicare recognizes the ventilator codes (CPT codes 94002 - 94004, 94660 and 94662) as physician services payable under the physician fee schedule. Medicare Part B under the physician fee schedule does not pay for ventilator management services in addition to an E/M service (e.g., critical care services, CPT codes 99291 - 99292) on the same day for the patient even when the E/M service is billed with CPT modifier -25. 13. Can both CPR and critical care be reported for the same patient encounter? Yes, as long as the respective requirements for each service are satisfied and evident from the medical record. Both AMA CPT and Medicare agree on this point. a. CPR is a non-E/M service encompassing such activities as supervising or performing chest compressions, adequate ventilation of the patient (e.g., bag-valve-mask), etc. CPT does not list a typical time to qualify for providing CPR. As a separately reportable service with critical care, the time spent providing CPR cannot be counted toward calculating total critical care time. b. Critical care is an E/M service encompassing time spent in work directly related to care of the individual patient's critical illness/injury, whether that time was spent at the immediate bedside or elsewhere on the floor or unit. For example, time spent on the unit or at the nursing station on the floor reviewing test results or imaging studies, discussing the critically ill patient's care with other medical staff or documenting critical care services in the medical record would be reported as critical care, even though it does not occur at the bedside. Also, when the patient is unable or clinically incompetent to participate in discussions, time spent on the floor or unit with family members or surrogate decision makers obtaining a medical history, reviewing the patient's condition or prognosis, or discussing treatment or limitation(s) of treatment may be reported as critical care, provided that the conversation bears directly on the management of the patient. Critical Care is a time-dependent E/M service. If the minimum total time requirement is not satisfied and/or documented, then an appropriate other E/M code should be reported. Of course, any site of service, and key components (i.e., history, physical examination, and medical decision making, etc.) criteria for such alternative E/M will have to be satisfied and documented. c. Some payers require that modifier -25 be appended to the critical care E/M or alternative E/M code in order to indicate that it is a separately identifiable E/M service. 14. Can time spent in Family Counseling / Discussion be included in critical care time? It depends. Routine daily updates to family members are considered part of critical care services and not separately billable. However, time spent with family member or other surrogate decision makers may be counted toward critical care time when these criteria are met: a. The patient is unable or clinically incompetent to participate in giving a history and/or decision making; and b. The discussion is necessary for determining treatment decisions c. A summary of any family discussion is to be documented within the medical record and should include that the patient was unable or incompetent to participate and the necessity of the discussion and any treatment decisions made, e.g., "no other source was available to obtain a history" or "because the patient was deteriorating so rapidly I needed to immediately discuss treatment options with the family". d. Telephone calls to family members and/or surrogate decision makers may be counted provided that they meet the same criteria as described above. e. All other family discussions, no matter how lengthy, may not be counted towards critical care time. Prepared by: Suzanne Forrest, 619-471-9154, sforrest@ucsd.edu Date issued: 02/12/2012 Page 4 UC San Diego Health Sciences Compliance Program http://health.ucsd.edu/compliance 15. What are the performance and documentation requirements for use of the critical care service codes with regard to Medicare's “split / shared service” rules for services involving physicians practicing with qualified non-physician practitioners (NPP) (e.g., physician assistants and nurse practitioners who are eligible for professional fee billing)? A split/shared E/M service performed by a physician and a qualified NPP of the same group practice cannot be reported as a critical care service. Critical care codes shall reflect the evaluation, treatment and management of a patient by an individual physician or qualified NPP and shall not be representative of a combined service between a physician and a qualified NPP. When CPT code time requirements for both 99291 and 99292 and critical care criteria are met for a medically necessary visit by a qualified NPP, the service shall be billed using the NPP’s appropriate individual NPI number. The provision of critical care services must be within the scope of practice and licensure requirements for the State in which the qualified NPP practices and provides the service(s). Collaboration, physician supervision and billing requirements must also be met. A physician assistant shall meet the general physician supervision requirements. 16. Global Surgery: How is critical care billing handled during the post-op period, e.g., surgery with global surgery days? Critical care services shall not be paid on the same calendar date the physician also reports a procedure code with a global surgical period unless the critical care is billed with CPT modifier -25 to indicate that the critical care is a significant, separately identifiable evaluation and management service that is above and beyond the usual pre and post-operative care associated with the procedure that is performed. This policy applies to any procedure with a 0, 10 or 90 day global period. 17. Global Surgery: Medicare Rules for Critical Care Services provided during the Pre-Op & Post-Op portion of global period of procedure with 90 day global period in Trauma & Burn Cases. a. Pre-op period. Preoperative critical care may be paid in addition to a global fee if the patient is critically ill and requires the full attention of the physician, and the critical care is unrelated to the specific anatomic injury or general surgical procedure performed. Such patients may meet the definition of being critically ill and criteria for conditions where there is a high probability of imminent or life threatening deterioration in the patient’s condition. Preoperatively, in order for these services to be paid, two reporting requirements must be met. Codes 99291 - 99292 and modifier -25 (significant, separately identifiable evaluation and management services by the same physician on the day of the procedure) must be used, and documentation identifying that the critical care was unrelated to the specific anatomic injury or general surgical procedure performed shall be submitted. An ICD-9-CM code in the range 800.0 through 959.9 (except 930.0 – 939.9), which clearly indicates that the critical care was unrelated to the surgery, is acceptable documentation. b. Post-operative period. Postoperatively, in order for critical care services to be paid, two reporting requirements must be met. Codes 99291 - 99292 and modifier -24 (unrelated evaluation and management service by the same physician during a postoperative period) must be used, and documentation that the critical care was unrelated to the specific anatomic injury or general surgical procedure performed must be submitted. An ICD-9-CM code in the range 800.0 through 959.9 (except 930.0 – 939.9), which clearly indicates that the critical care was unrelated to the surgery, is acceptable documentation. 18. How are units of service calculated for critical care time? The following table illustrates how units of critical care service are determined. a. 99291 = 1st hour of critical care services (30 min to 1 hr 14 min) b. 99292 = each additional 30 minutes of critical care services c. Note: Consult the CPT book for applicable codes for critical care services provided to neonates, infants and children. Prepared by: Suzanne Forrest, 619-471-9154, sforrest@ucsd.edu Date issued: 02/12/2012 Page 5 UC San Diego Health Sciences Compliance Program http://health.ucsd.edu/compliance Time Unit CPT Code Less than 30 minutes Choose the appropriate E/M code, e.g., 99231-99233 30 – 74 minutes (30 min - 1 hr 14 min) 99291 75 – 104 minutes (1 hr 15 min - 1 hr 44 min) 99291 (1 unit) + 99292 (1 unit) 105 – 134 minutes (1 hr 45 min - 2 hrs 14 min) 99291 (1 unit) + 99292 (2 units) 135 – 164 minutes (2 hr 15 min - 2 hrs 44 min) 99291 (1 unit) + 99292 (3 units) References: CMS Manual System, Pub 100-04 Medicare Claims Processing, Transmittal 1548, issued: 7/9/2008, Change Request 5993. Subject: “Critical Care Visits & Neonatal Intensive Care (Codes 99291 – 99292)”, http://www.cms.hhs.gov/Transmittals/Downloads/R1548CP.pdf CMS MLN Matters Number: MM5993, Effective date: 7/1/2008, “Critical Care Visits & Neonatal Intensive Care (Codes 99291 – 99292)”, http://www.cms.hhs.gov/MLNMattersArticles/downloads/MM5993.pdf CMS Medicare Claims Processing Manual, 100-4, Chapter 12, Physicians / Nonphysician Practitioners, Section 30.6.12 – Critical Care Visits & Neonatal Intensive Care (Codes 99291 – 99292), https://www.cms.gov/manuals/downloads/clm104c12.pdf Palmetto J1 Part B, “Critical Care & Global Surgery Package”, http://www.palmettogba.com/palmetto/providers.nsf/DocsCat/Providers~Jurisdiction%201%20Part%20B~Articles~ EM%20Help~8DHTBR8657?open&navmenu=Articles%7C%7C%7C%7C [California Medicare MAC] Prepared by: Suzanne Forrest, 619-471-9154, sforrest@ucsd.edu Date issued: 02/12/2012 Page 6