Alan Merry Interview Kim Hill
advertisement

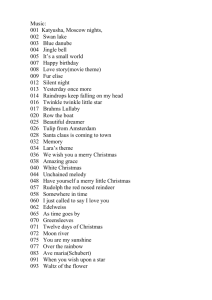
Radio NZ National Saturday Morning with Kim Hill – 12 March 2011 – 08.46am Professor Alan Merry talks about the World Health Organisation’s Safe Surgeries Saves Lives Programme, founded by Dr Atul Gawande. KIM HILL: Last week I spoke to surgeon and writer, Dr Atul Gawande, whose latest book about the complex business of surgery is called: The Checklist Manifesto, How to Get Things Right. A basic checklist, it's a simple thing, plenty of other complex endeavours use it, construction, aviation. Dr Gawande found that it helps save lives in the OR, the Operating Room. He heads the World Health Organisation's Safe Surgeries Saves Lives program and we're talking about that and as he said, Auckland Hospital is one of eight around the world to trial the checklist. Professor Alan Merry, Head of the Department of Anaesthesia - I've been practicing – Anaesthesiology, say it for me. ALAN MERRY: Anaesthesiology. [Laughs] KIM HILL: I knew you'd say it right. I suppose you had to go to university to say that, heads the Save Anaesthesia Group of the WHO's program and he's with me now in our Auckland studio, good morning and welcome. ALAN MERRY: Good morning Kim. KIM HILL: Just going back to Dr Gawande's book, The Checklist Manifesto, he says that when the results first came in from your hospital and the seven others on the trial, the results were so astonishing that he had to go back and start looking for mistakes. Because the rate of major complications for surgical patients in all eight hospital fell by 36 per cent after introduction of the checklist and deaths fell by 47 per cent. Now, was that your specific experience or we're talking about an average that's raised up by others, if you see what I mean? ALAN MERRY: No, that is an average. The effect size was greater in the low income countries as you might expect and in a country like New Zealand and other places like Seattle, where the standards were already high, the effect was smaller. But it was still more than I would have expected and still quite convincing. KIM HILL: Just run it past me again, how did you employ the checklist - what was it? How did it work? ALAN MERRY: Well we're still doing it, of course. But it's basically three phases, so the first phase is when the patient is brought into the operating room there are checks done in the operating room involving not just, as is often in the past been the case, one person, say the nurse, but actually involving more than one of the teams. Ideally all three, but as a minimum the anaesthetist and the nurse checking together, because… KIM HILL: What's the thinking behind that? ALAN MERRY: Well it's to get people talking to each other and engaging. The checklist isn't just about the checks, it's actually designed to promote communication and teamwork. And so the other thing, of course, is that many of these checks – people often ask, weren't these done before? Well they were, but typically these checks were done in the holding area. Now in the last… KIM HILL: You mean before they got to the operating room, yes? ALAN MERRY: Before they got to the operating room and in the last 20 years or so I have had three occasions when patients were checked in the holding area and then taken to the wrong operating room and so I've ended up with a patient on the table in front of me that was, in fact, meant to be in the operating room next door. KIM HILL: And so you've raised the completely wrong operation, that's everybody's nightmare. ALAN MERRY: Well it's interesting because one of the things that - so I work in the cardiac unit at Auckland Hospital now, it used to be Greenlane and I do a regular tutorial on how to check the anaesthesia machine and one of things that I actually do with the trainees is I get one of them to role model being the patient. And the aim is for them to actually show that they will check the patient, which they frequently don't, despite that strong hint. And my point is you can be really clever, you can do very good anaesthesia and surgery and be utterly brilliant, but if you've got the wrong patient, it's not very good. KIM HILL: So really, just... ALAN MERRY: So it's a very fundamental… KIM HILL: Yeah… ALAN MERRY: Very fundamental. KIM HILL: Shaking assumptions that are made so easily that nobody bothers to think about them. ALAN MERRY: Well that's right and one of the great risks - and it's a risk even with our checklist - is that the people get into the mindset of going through the motions. And one of the things that we really are trying to do is get people to engage in it. There's some small print at the bottom that says that you can modify for local conditions and that's important, because what we want is for people to think about how to make it work in their own operating room. There are actually three phases. There's another phase just before the incision, which is called the time-out, where you just stop everything and check that you really are on track and that everybody's got the right mindset. And at that point, there's actually a very novel thing which is introducing each other, particularly new people or people that aren't known. KIM HILL: Back to the team thing. ALAN MERRY: That's right. Now interestingly I thought that would be a real - go down like a lead balloon idea. KIM HILL: Like let's all hold hands and make friends. ALAN MERRY: And obviously if you're in a particular, very close knit team where everybody's worked together for 20 years and it's all - everybody knows each other then all you need to do is just say, we all know each that's fine. But what's been intriguing to me is that it's turned out, I'm not the only person with a bad memory for names and I think some of the surgeons have been quite pleased to have an excuse to say, you know, let's just introduce ourselves… KIM HILL: Why don't you wear nametags? ALAN MERRY: Well we do to some extent, but you know you're in greens, they're often quite hard to read. I don't know if you've noticed that, but even in social functions when people have nametags, you can sort of end up peering rather hard at them to try to see what they're saying. KIM HILL: Yes, I have. ALAN MERRY: And so it is a very good thing just to do the introduction. KIM HILL: Dr Gawande said that he, in the process of trying to set this up - this trial of the eight hospitals, he was thrown out of more operating rooms than he could count. There was resistance to the idea and you've hinted at this. Why? ALAN MERRY: Well it's a glass three-quarters full. I think that the good news is that the major people and most of the people at Auckland Hospital really got behind it, and the university as well. So we did it as a combined thing and there was a lot of support. But people are resistant to change and I think part of it is that everybody is trying to do the right thing. They put a lot of time and effort into getting their own systems working well and then somebody comes along with a new idea and says why aren't you doing this, or please would you do this? I think it's a bit natural to be resistant. And the thing that flipped it of course was getting the data that showed actually this makes a difference. And then it becomes much harder to say well, I don't want to do it. KIM HILL: I mean presumably there are what Atul Gawande would call heroic surgeons, I suspect who say, this is bureaucracy gone mad and I don't need this stupid business and leave me alone, I've got a patient to operate on here. ALAN MERRY: Well more reasonably I think there's a view that there is too much paperwork and too many things that we have to go through. And there is this risk that it becomes just a go through the motion… KIM HILL: Another form…yeah. ALAN MERRY: And that is something that has to be managed and Dr Gawande last week talked a bit about the design of checklists and the importance of getting them short and meaningful. KIM HILL: And the difficulty of what you leave out. ALAN MERRY: Precisely, it's more about what you leave out then what you put in. KIM HILL: You've been involved in the Health, Quality and Safety Commission. This presumably incorporates this concept. ALAN MERRY: It's one of the initiatives. We actually - the initiative was ahead of that, but it is one of the ones that we are going to be putting weight behind, if you like. Keeping that momentum going, because all of these things have a tendency to get off to a good start and then to drift a bit. So I think we do need to do some reinforcement of it. But it's only one of many initiatives that we will be looking at over the next year and beyond. KIM HILL: What are some of the other ones? ALAN MERRY: Well one of the big problems that occurs in healthcare is medication errors and there is a long-term plan to move New Zealand towards a much more systematic electronic prescribing and checking of medications. But that will take some years and a lot of money. And the first step is that we are trying, this year, to roll-out a standardised adult in-patient prescribing form for all hospitals in New Zealand, which means that staff that move around - junior staff and some nurses - wherever they are, they'll be using the same prescription form. And not only that, but it will be one that's been well designed. So for example, some of the errors that occur involve the decimal point and that's actually quite serious errors if you get in the wrong place. KIM HILL: You get 10 times too much. ALAN MERRY: Precisely, or too little - equally bad actually depending on the circumstances – but the form has a pre-printed decimal point and it's standardised. It's got a standardised way of writing prescriptions. . And that may seem, again, like an obvious thing, but the fact is I don't think any country in the world has got a standardised form across its entire system. We will probably be the first. KIM HILL: So what everybody goes and gets their own sorts for forms? ALAN MERRY: Each hospital introduces its own. One of the intriguing things is that some of them are good. There's always this argument well, our form is actually already excellent. Why should we take the standardised one? KIM HILL: Yes. ALAN MERRY: Well the answer, of course - and the aviation people discovered this, because the way aviation safety improved was to move away from what you mentioned, the heroic concept of everybody trying to be the best, to say, actually what we need is something that's good that we know that works well and get everybody to do the same. Now as Dr Gawande said last week, that's not dumbing down and what's more it's not saying you shouldn't vary treatment around patients. Clearly every patient's different and clearly treatments need to be tailored in a very specific way to each individual. But once you've decided to actually administer a particular treatment, to give drugs for example, that's a process and it's the processes that we need to standardise. Now the adoption of process engineering - and the checklist is really just a process engineering tool - is something that healthcare's been a bit slow over. KIM HILL: One of the other things you're involved in - and we haven't got very long to talk about it actually – but it's Lifebox. And at this particular point, where the world does seem to be falling apart in a third world direction generally speaking, I thought it might be useful to talk about it. What's the Lifebox? ALAN MERRY: Well it's actually one of the elements on the checklist which is a pulse oximeter, which is a monitoring device that measures the oxygen in your bloodstream. When I started anaesthesia some 30 years ago, we didn't have that monitoring and we had to rely on looking at the colour of the patient and other signs to tell if their oxygen levels were falling. And that's actually quite difficult. This monitoring… KIM HILL: Because you mean they have to be quite far gone before they… ALAN MERRY: Because really it's quite a late sign so you can be quite bad before it becomes apparent that there's a problem. Whereas the pulse oximetry is a fantastic monitor which has changed the face of modern anaesthesia. And in a country like New Zealand, it's used universally. But there's a big gap. We've done some work that suggests that 77,000 operating rooms around the world - and some millions of operations are done without this monitoring. It's actually a symbolism on this because it goes without a lot of other things. Those other places that have poor standard of care, low qualifications of staff and many other things. So this is a project in which the primary thing is the - we've sourced and specified a very low cost pulse oximeter that is also very high quality. It's one that any of us would be happy to use in New Zealand in our patients. And we have built around that an educational package and advocacy package with the whole message of which is that the safe management of surgery does include safe anaesthesia, that does include the technology and it does include the skills and the resources to respond to the information on that technology. KIM HILL: Again, a very simple idea. ALAN MERRY: It is and it's been going now for some six or seven years. KIM HILL: Where's the money coming from? ALAN MERRY: Well we are looking to various sources. We've had a substantial donation from Smile Train. We've had various individual including I might say, Dr Gawande has contributed generously. It is possible to go online on the website and actually donate and that has gone live recently and we're hoping that many – particularly anaesthesia providers will be enthusiastic. Because for US$250 which is what one of these costs, you can conceive of actually putting one of these devices into an operating room and saving lives, which is quite an exciting idea really. KIM HILL: I just need to check, I talked to Atul Gawande about music and what music he likes to listen to. Do you ever - do people delivering the anaesthetic get to choose the music? ALAN MERRY: Yes, it varies - a lot depends on people's view. I am probably - I quite like quietish classical music but I do - one thing is though that there are - and it's the same cockpit in the aeroplane, there are times of the proceedings when actually what I need is quiet. The critical moments, at the beginning and end in particular or if something is going wrong, I just ask if we could please keep things quiet. KIM HILL: I'm sure that were I conscious, I'd agree with you. It's nice to talk to you, thank you. I've been talking to Dr Alan Merry, nine o'clock now.