Neuroanatomy Ch 7 287-297 [4-20
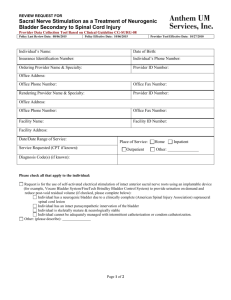
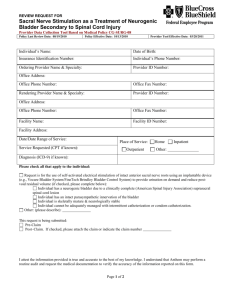
advertisement

Neuroanatomy Ch 7 287-297 Somatosensory Pathways Parasthesias – lesions of somatosensory pathways cause abnormal positive sensory phenomena -lesions of posterior column-medial lemniscal pathways cause tingling, numb sensation; tight bandlike sensation around waist, or gauze on fingers when trying to palpate -lesions of anterolateral pathways cause sharp, burning, searing pain -lesions of parietal lobe/primary sensory cortex can cause contralateral numb, tingling -lesions of thalamus can cause severe contralateral pain (Dejerine-Roussy syndrome) -lesions of C spine can cause Lhermitte’s sign (electricity like sensation down back/extremities during neck flexion) -lesions of nerve roots cause radicular pain that radiates down limb through dermatome; numbness, tingling -dysthesia (unpleasant sensation), allodynia (painful sensations caused by nonpainful stimuli), hyperpathia/hyperalgesia (enhanced painful stimuli), hypesthesia (decreased sensation) Spinal Cord Lesions – obvious when there is a sensory level/motor dysfunction corresponding to the level of the lesion; abnormal sphincteric function can help diagnosis -in acute lesions like trauma, there is initial phase of spinal shock (flaccid paralysis below lesion, loss of DTRs, decreased sympathetic flow to vascular smooth muscle) followed by spasticity and upper motor neuron signs later -chronic myelopathy (spinal cord dysfunction) is seen with degenerative disorders of spine, most commonly in CERVICAL or LUMBAR regions, where spine and nerve roots compressed causing combination upper/lower motor neuron signs -if caused by tumors, promptly resect or irradiate to prevent irreversible loss of ambulation -80% of patients treated for spine compression after losing ambulation will remain nonambulatory, 80% of patients treated before losing ambulation will retain it -Infarction of spinal cord due to ANT SPINAL ARTERY OCCLUSION, leading to anterior cord syndrome; causes are trauma, aortic dissection, thromboemboli, and disc emboli -spinal dural AVM can lead to permanent or transient episodes of spinal cord dysfunction -myelitis, which is inflammatory or infectious, can cause spinal cord dysfunction; pt’s present with spine dysfunction with rapid onset -Epidural Abscess – can cause irreversible damage Sensory Loss: Patterns and Localization: 1. Primary Somatosensory Cortex: deficit is CONTRALATERAL; discriminative touch and joint position sense are most severely affected; cortical sensory loss is present with extinction (decreased stereognosis) and gaphesthesia; 2. Thalamic Ventral Posterior Lateral (VPL) and Ventral Posterior Medial (VPM) Nuclei or Thalamic Somatosensory Radiations: Deficit is CONTRALATERAL; sensory loss does not begin at midline; may be more noticeable in face, hand and foot; all sensory modalities involved (sometimes no motor deficit) a. Larger lesions may be accompanied by hemiparesis or hemianopia; lesions of thalamic somatosensory radiations can cause contralateral hemisensory loss associated with hemiparesis 3. Lateral Pons or Lateral Medulla: causes pain and temp sensation on contralateral side of body, same side on FACE; involves anterolateral pathways and spinal trigeminal nucleus 4. Medial Medulla: contralateral loss of vibration and joint position sense (medial lemniscus) Spinal Cord Syndromes: Transverse Cord Lesion – whole level is cut, all sensory/motor pathways disrupted with a sensory level (all dermatomes below lesion are affected), caused by trauma, tumor, MS Hemicord Lesions: Brown-Séquard Syndrome – damage to lateral corticospinal tract causes IPSILATERAL upper motor neuron weakness; damage to posterior columns causes IPSILATERAL loss of vibration and joint position sense loss with CONTRALATERAL loss of pain/temp sensation -often begins slightly below lesion because anterolateral fibers ascend 2-3 segments as they cross in the anterior commissure -may be a strip of pain/temp loss ipsilaterally due to damage of dorsal horn before neurons crossed oer -causes are penetrating injuries, MS, compression from tumors Central Cord Syndrome – in small lesions, damage to spinothalamic fibers crossing anterior commissure causes bilateral regions of suspended sensory loss to pain/temp -lesions of cervical cord cause cape distribution -Large lesions, anterior horn cells are damaged to produce lower motor neuron deficits at level of lesion. Corticospinal tracts are affected, causing upper motor neuron signs/posterior columns also affected -may be near complete loss of pain/temp below lesion EXCEPT for a region of sacral sparing -causes include contusion, nontraumatic or posttraumatic syringomyelia, tumors Posterior Cord Syndrome – loss of vibration and position below level of the lesion; causes include trauma, compression from tumors, and MS Anterior Cord Syndrome – damage to anterolateral pathways cause loss of pain/temp below level of lesion, and damage to anterior motor horn cells produces lower motor neuron weakness at level of lesion -larger lesions may cause lateral corticospinal tracts to be involved -causes include trauma, MS, anterior spinal artery infarct Anatomy of Bowel, Bladder, Sexual Function – parasympathetics arise from S2,3,4 (sacral parasympathetic nuclei) and sympathetics arise from T11-L1 (intermediolateral column) -voluntary somatic motor fibers arise from anterior horn form S2-4 to control pelvic floor muscles; and from sphincteromotor nucleus of Onuf at S2-4 to control urethral and anal sphincters Bladder Function – bladder emptying is under voluntary control; sense of bladder fullness in somatosensory cortex initiates descending pathway from medial frontal micturition centers that activate voiding (detrusor) reflex; the detrusor reflex is mediated by intrinsic spine circuits and regulated by pontine micturition center -reflex is initiated by voluntary relaxation of external urethral sphincter, which triggers inhibition of sympathetics to the bladder neck, causing it to relax activation of parasympathetics to cuase detrusor muscle contraction -urine flow through urethra activates sphincter relaxation and detrusor contraction -urine flow stoppage causes sphincter contraction, detrusor relaxation through urethral reflex -Lesions affecting BILATERAL medial frontal micturition centers result in reflex activation of pontine and spinal micturition centers when bladder is full, causing bladder emptying NOT to be under voluntary control; causes are hydrocephalus, parasagittal meningioma, bifrontal glioblastoma -lesions BELOW pontine micturition center and above conus medullaris (S2-4) cause a flaccid, acontractile bladder which evolves to a hyperreflexic (spastic) bladder -in an ATONIC bladder, reflex contractions of urethral sphincters persist to cause urinary retention and bladder distention -post-void residual volume is increased -in a hyperreflexive bladder, detrusor-sphincter dyssnergia occurs where both the detrusor muscle and urethral sphincter tone are increased in an uncoordinated fashion which may cause a sense of urinary urgency or urge incontinence; residual volume increases -lesions of PERIPHERAL nerves or of S2-4 cause a flaccid areflexic bladder, or a significantly impaired bladder contractility resembling acontractile bladder; due to loss of parasympathetic outflow to detrusor and/or loss of afferent sensory information from bladder -overflow incontinence is often present -causes are diabetic neuropathy and compression of conus medullaris by trauma, tumor -urinary retention is also caused by conditions such as prostatic hypertrophy, urethral strictures, instrinsic sphincter deficiency Neurogenic bladder = flaccid + hypperreflexic bladder Bowel Function – fecal continence is controlled by descending pathways originating in medial frontal lobes; anal sphincter closure is maintained by internal smooth muscle sphincter innervated by parasympathetics, while an external striated muscle sphincter innervated by pelvic nerves from S2-4 and pelvic floor muscles innervated by sacral anterior horn cells -GI motility depends on parasympathetics from S2-4 for colorectal smooth muscle beyond splenic flexure -fecal incontinence can be caused by diffuse cerebral or medial frontal lesions, spinal lesions, or lesions of sacral nerve roots -in acute spinal lesions, anal sphincter is completely flaccid and constipation Sexual Lubrication, Erectile, and Ejaculatory Function – genitalia sensation is conveyed by pudendal nerve (S2-4) -in female, lubrication is secreted by bartholin’s glands by parasympathetic innervation, and increased vaginal blood flow and secretions are sympathetically mediated -both sympathetics and parasympathetics are involved in erection -ejaculation occurs through sympathetically mediated contraction of smooth muscle, causing emission of semen into urethra, followed by rhythmic reflex contractions of striated muscles to result in forceful expulsion of semen