Consultation Decision Analytic Protocol (DAP) to guide the
advertisement

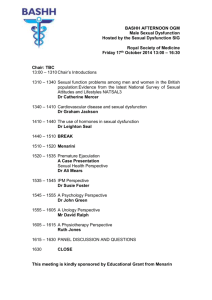
Consultation Decision Analytic Protocol (DAP) to guide the assessment of sexual health medicine professional attendance and case conferencing items (Application 1171) January 2012 Table of Contents MSAC and PASC.............................................................................................. 3 Purpose of this document ........................................................................... 3 Summary of key matters for which PASC seeks input from stakeholders ....................................................................................................................... 4 Purpose of application ................................................................................... 5 Background .................................................................................................... 5 Current arrangements for public reimbursement ........................................ 5 Intervention ................................................................................................... 6 Description .................................................................................................. 6 Prerequisites ............................................................................................... 7 Co-administered and associated interventions ............................................ 8 Listing proposed and options for MSAC consideration ................................... 8 Proposed MBS listing ................................................................................... 8 Clinical place for proposed intervention .................................................... 10 Comparator .................................................................................................. 14 Clinical claim ................................................................................................ 15 Outcomes and health care resources affected by introduction of proposed intervention ................................................................................................. 15 Clinical outcomes ...................................................................................... 15 Health care resources................................................................................ 15 Proposed structure of economic evaluation (decision- analytic).............. 16 2 MSAC and PASC The Medical Services Advisory Committee (MSAC) is an independent expert committee appointed by the Minister for Health and Ageing (the Minister) to strengthen the role of evidence in health financing decisions in Australia. MSAC advises the Minister on the evidence relating to the safety, effectiveness, and cost-effectiveness of new and existing medical technologies and procedures and under what circumstances public funding should be supported. The Protocol Advisory Sub-Committee (PASC) is a standing sub-committee of MSAC. Its primary objective is the determination of protocols to guide clinical and economic assessments of medical interventions proposed for public funding. Purpose of this document This document is intended to provide a draft decision analytic protocol that will be used to guide the assessment of an intervention for a particular population of patients. The draft protocol will be finalised after inviting relevant stakeholders to provide input to the protocol. The final protocol will provide the basis for assessment of the intervention. The protocol guiding the assessment of the health intervention has been developed using the widely accepted “PICO” approach. The PICO approach involves a clear articulation of the following aspects of the question for public funding the assessment is intended to answer: Patients – specification of the characteristics of the patients in whom the intervention is to be considered for use Intervention – specification of the proposed intervention and how it is delivered Comparator – specification of the therapy most likely to be replaced by the proposed intervention Outcomes – specification of the health outcomes and the healthcare resources likely to be affected by the introduction of the proposed intervention 3 Summary of key matters for which PASC seeks input from stakeholders The PASC welcomes comments on any aspect of this draft DAP but would particularly appreciate comment from stakeholders on the following issues: Whether the proposed Medicare Benefits Schedule (MBS) items as included in Table 1 on p.7 are appropriately worded and structured. In particular, PASC seeks comment on whether the item descriptor(s) for the proposed items should include clauses limiting the number of times the items should be claimable in a 12 month period; Potential sources of estimates for: o likely rates of transfer from current MBS items to proposed MBS items; o likely rates of transfer from services delivered in the public to private sector as a consequence of listing the proposed items; and likely rates of expansion of the population who will receive treatment from a sexual health o medicine specialist as a consequence of listing the proposed items What outcomes could be used as a basis for determining the effectiveness of provision of services by sexual health medicine specialists compared with no availability of services The relationship between any surrogate outcomes upon which judgement of comparative effectiveness could be made and final patient-relevant outcome of quality-adjusted survival term How the structure for the economic evaluation might be advanced (e.g., definition of the ‘successful outcome’; definition of the services delivered in each branch of the tree shown) How broader considerations besides the impact on a patient’s quality-adjusted survival could be incorporated into the economic analysis. 4 Purpose of application A proposal for an application requesting listing of four time-tiered professional attendance (consultation) and six time-tiered case conferencing items on the Medicare Benefits Schedule (MBS) to be provided by sexual health medicine specialists has been progressed by the Department of Health and Ageing (DoHA) in consultation with the Australasian Chapter of Sexual Health Medicine (AChSHM). Background Current arrangements for public reimbursement There are currently no specific sexual health medicine professional attendance or case conferencing items available on the MBS. Sexual health medicine was recognised as a speciality in 2009 by the Australian Medical Council. It was reported to PASC that there are currently approximately 115 sexual health medicine specialists in Australia and that a minority of sexual health medicine practice is provided in the private setting. In the 2010/11 Federal Budget, sexual health medicine specialists were granted access to the Group A3 specialist items on the MBS. Medicare data as of 26 October 2011 indicates 23 sexual health medicine specialists had registered to use A3 specialist attendance items. The large majority of sexual health medicine specialists have not registered with Medicare because they prefer to seek Medicare reimbursement for their services in the capacities as GPs, other medical practitioners, etc, as set out below rather than through items included in A3 of the MBS. It is suggested that this decision appears to be influenced by the fact that, given the mode of practice used to deliver sexual health medicine services, the A1, A2, and A15 item structures provide a higher level of remuneration than the A3 item structure. Reimbursement for services is currently claimed under the following groups of MBS services: GROUP A1 – GENERAL PRACTITIONER PROFESSIONAL ATTENDANCES Figures provided by the AChSHM indicate that 19% of sexual health medicine specialists hold Fellowship of the Royal Australian College of General Practitioners and are able access to this group of items. GROUP A2 – OTHER MEDICAL PRACTITIONER PROFESSIONAL ATTENDANCES Sexual health medicine specialists who are non-vocationally registered GPs, specialist trainees or other medical practitioners are able access to this group of items. GROUP A3 – SPECIALIST PROFESSIONAL ATTENDANCES October 2011 data indicates 23 medical practitioners have registered with Medicare Australia as sexual health medicine specialists and have access to this group of items. GROUP A4 – CONSULTANT PHYSICIAN PROFESSIONAL ATTENDANCES Figures provided by the AChSHM indicates that 10% of sexual health medicine specialists hold a Fellowship of the Royal Australasian College of Physicians (RACP) and are able to access to this group of items. 5 GROUP A8 – CONSULTANT PSYCHIATRIST PROFESSIONAL ATTENDANCES The Chapter has indicated that one sexual health medicine specialist holds a Fellowship of the Royal Australian and New Zealand College of Psychiatrists (RANZCP) and would have access to this group of items. GROUP A15 – CASE CONFERENCING There are no existing case conferencing items for specialists. However, sexual health medicine specialists who have not registered with Medicare Australia as Group A3 ‘specialists’, and for Medicare purposes are ‘GPs’, have access to existing Group A15 case conferencing items 721758. Consultant physicians have access to case conferencing items 820-858; and consultant psychiatrists have access to case conferencing items 861-880. The proposal notes that the traditional structure of specialist professional attendances (e.g., Groups A3 and A4 of the MBS) provide a more generously rebated item for an initial attendance and a less generously rebated item for a follow-up attendance. The AChSHM argues that the attendance items in this section of the MBS have been available to, and reflect the nature of the practice of procedural specialists, i.e. those whose practices also involve significant procedural work. The proposal suggests that this traditional structure does not suit discussion-based, cognitive specialties such as sexual health medicine, which rely on time spent with a patient to assess and resolve more complex issues. The AChSHM claims that the A3 items provide inadequate reimbursement for clinically effective sexual health medicine practice because they are a consulting rather than procedural specialty. Hence, it is proposed that an application requesting listing of four time-tiered professional attendance (consultation) and six time-tiered case conferencing items on the MBS to be provided by sexual health medicine specialists be submitted to MSAC. Intervention Description In relation to the professional attendance items, a sexual health medicine specialist would, typically, obtain a patient’s sexual clinical history, conduct expert examination, order relevant testing, and provide follow-up treatment and management (via a number of consultations, as required). As initial and follow-up consultations can be either shorter or longer, depending on a patient’s needs, time-tiered items have been proposed to enable sexual health medicine specialists to bill the relevant item based on time spent with a patient. 1. In relation to the case conferencing items, it is proposed that these items would only apply to a service in relation to a patient who suffers from at least one disorder/condition, across the medical specialties, that has been (or is likely to be) present for at least 6 months, or that is terminal, and has complex needs requiring care from a multidisciplinary team. PASC presumes that a note would be included in the item descriptor for case conferencing items directing physicians to explanatory notes associated with the item that specify these criteria. The case conferencing items would enable a multidisciplinary team to carry out the following: discuss a patient’s history; identify a patient’s multidisciplinary care needs; identify outcomes to be achieved by members of the case conference team giving care and service to the patient; 6 identify tasks that need to be undertaken to achieve these outcomes, and allocating those tasks to members of the case conference team; and assess whether previously identified outcomes (if any) have been achieved. Prerequisites REFERRAL The proposed item descriptors (provided in Table 1) indicate that the patient must be referred for the intervention by a medical practitioner who is not the sexual health medicine specialist providing the intervention. The referral process will be in accordance with the MBS G6.1 Referral of Patients to Specialist or Consultant Physician. Although the proposed item descriptors for professional attendances include the requirement for a referral from a medical practitioner, the proposal notes that the need to obtain a referral from a GP may compromise access to timely sexual health specialist advice and treatment. TRAINING It is proposed that only qualified sexual health medicine specialists will be able to claim for the delivery of the proposed MBS items. In order to be accepted into the training program to acquire fellowship of the AChSHM, an applicant must firstly satisfy all three of the following conditions: (i) Be a registered medical practitioner in Australia or New Zealand. (ii) EITHER hold Fellowship of one of the following Colleges or Faculties: Physicians (FRACP) Adult Internal Medicine or Paediatrics & Child Health Dermatology (FACD) Obstetrics and Gynaecology (FRANZCOG) General Practice (FRACGP and FRNZCGP) Pathology (FRCPA) Psychiatry (FRANZCP) Public health Medicine (FAFPHM) Rural and Remote Medicine (FACRRM) Surgery (FRACS – urology) OR in the case of overseas trained specialists (including general practitioners), have been considered equivalent by the relevant Australian or New Zealand medical college OR have completed Basic Training of the RACP (including success in the FRACP Examination) (iii) have a satisfactory practice history (no professional misconduct or disciplinary issues). Trainees are then expected to complete formal instruction via units in university courses in the following areas: Fertility regulation Sexual health counselling HIV medicine Sexual health medicine Epidemiology 7 Biostatistics Sexual assault Principles of adult education The proposal for an application notes that, by requiring fellowship with another accredited medical college and then requiring a further three years advanced training in sexual health medicine, specialists in sexual health medicine in effect train for approximately 10 years. Co-administered and associated interventions As noted above, a requirement will be that referral from a medical practitioner be required prior to a professional attendance by a sexual health medicine specialist. No other specific services are required to be administered prior to, with or following the proposed medical services. However, follow-up services that might need to be rendered following a sexual health medicine service would be discussed during the consultation. A sexual health medicine specialist may order various pathology tests or diagnostic imaging services during an initial or subsequent consultation for assessment of a patient’s status. Listing proposed and options for MSAC consideration Proposed MBS listing The proposed MBS item descriptors are provided in Table 1. Table 1: Proposed MBS item descriptor for proposed sexual health medicine services Category 1 – Professional attendances MBS Item XXX Professional attendance by a sexual health medicine specialist in the practice of his or her specialty, following referral of the patient to him or her by a medical practitioner - an attendance of not more than 15 minutes duration Fee: $TBA Benefit: 75% = $TBA 85% = $TBA MBS Item XXX Professional attendance by a sexual health medicine specialist in the practice of his or her specialty, following referral of the patient to him or her by a medical practitioner - - an attendance of more than 15 minutes, but not more than 30 minutes duration Fee: $TBA Benefit: 75% = $TBA 85% = $TBA MBS Item XXX Professional attendance by a sexual health medicine specialist in the practice of his or her specialty, following referral of the patient to him or her by a medical practitioner - an attendance of more than 30 minutes, but not more than 45 minutes duration Fee: $TBA Benefit: 75% = $TBA 85% = $TBA MBS Item XXX Professional attendance by a sexual health medicine specialist in the practice of his or her specialty, following referral of the patient to him or her by a medical practitioner - an attendance of more than 45 minutes duration Fee: $TBA 8 Benefit: 75% = $TBA 85% = $TBA Table 1: Proposed MBS item descriptor for proposed sexual health medicine services Category 1 – Professional attendances Case conferencing items MBS Item XXXX CASE CONFERENCES - SEXUAL HEALTH MEDICINE SPECIALIST Attendance by a sexual health medicine specialist, as a member of a case conference team, to ORGANISE AND COORDINATE A CASE CONFERENCE, where the conference time is at least 15 minutes, but less than 30 minutes, with a multidisciplinary team of at least three other formal care providers of different disciplines Fee: $TBA Benefit: 75% = $TBA 85% = $TBA MBS Item XXXX Attendance by a sexual health medicine specialist, as a member of a case conference team, to ORGANISE AND COORDINATE A CASE CONFERENCE, where the conference time is at least 30 minutes, but less than 45 minutes, with a multidisciplinary team of at least three other formal care providers of different disciplines (Fee: $TBA Benefit: 75% = $TBA 85% = $TBA MBS Item XXXX Attendance by a sexual health medicine specialist, as a member of a case conference team, to ORGANISE AND COORDINATE A CASE CONFERENCE, where the conference time is at least 45 minutes, with a multidisciplinary team of at least three other formal care providers of different disciplines Fee: $TBA Benefit: 75% = $TBA 85% = $TBA MBS Item XXXX Attendance by a sexual health medicine specialist, as a member of a case conference team, to PARTICIPATE IN A CASE CONFERENCE, (other than to organise and to coordinate the conference) where the conference time is at least 15 minutes, but less than 30 minutes, with a multidisciplinary team of at least two other formal care providers of different disciplines Fee: $TBA Benefit: 75% = $TBA 85% = $TBA MBS Item XXXX Attendance by a sexual health medicine specialist, as a member of a case conference team, to PARTICIPATE IN A CASE CONFERENCE, (other than to organise and to coordinate the conference) where the conference time is at least 30 minutes, but less than 45 minutes, with a multidisciplinary team of at least two other formal care providers of different disciplines Fee: $TBA Benefit: 75% = $TBA 85% = $TBA MBS Item XXXX Attendance by a sexual health medicine specialist, as a member of a case conference team, to PARTICIPATE IN A CASE CONFERENCE, (other than to organise and to coordinate the conference) where the conference time is at least 45 minutes, with a multidisciplinary team of at least two other formal care providers of different disciplines Fee: $TBA Benefit: 75% = $TBA 85% = $TBA TBA = to be advised. Fees will be calculated based on cost inputs for time-based professional attendances. PASC determined that it should seek input from stakeholders on whether the proposed items are appropriately worded and structured. PASC noted that there are substantial differences between the proposed items shown in Table 1 and other items that may be comparable and that are included on the MBS (e.g., MBS items 132 and 133 for complex assessment and preparation of management plans for patients are limited to consultant physicians): Other items provide some specification of the service that is expected to be delivered in a complex assessment (e.g., the items specify what is involved in conducting an assessment or a review of a patient and what is included in a treatment and management plan for a patient) whereas the proposed items do not provide any indication of what services are expected to be delivered. 9 Unlike other items such as MBS items 132 and 133 that are claimable only once in a 12 month period, the proposed listing does not limit the number of times the proposed items can be claimed in a 12 month period. The proposed item descriptors do not specify any criteria that need to be satisfied to trigger an assessment by a sexual health medicine specialist. In contrast, it was noted that only one item 132 and one item 133 is claimable in a 12 month period. PASC considered that it should seek input on whether the item descriptor(s) for the proposed items should include clauses limiting the number of times the items should be claimable in a 12 month period. Although the proposed item descriptors do not specify the patient population to whom the items may be delivered, PASC considered it reasonable to assume that a sexual health medicine specialist would only be attending to patients with sexual health problems. However, it noted that patients requiring the services of a sexual health medicine specialist are a heterogenous group. PASC agreed that no specification of the patient population to whom the items may be delivered needs to be included in the MBS item descriptors. Clinical place for proposed intervention Patients of sexual health medicine include people of all ages who suffer from any type of sexual health disorder. Sexual health medicine involves the assessment, diagnosis and treatment of a variety of sexual-related diseases and symptoms (e.g. HIV and other sexually transmitted diseases; genital pain; sexual function; and skin problems). Sexual health specialists manage a range of complex medical and other issues with patients. It is claimed that access to specialists ensures patients are exposed to greater expertise than otherwise would be available. Benefits flow to partners, families and the community as a whole. The proposal for an application indicates that the clinical place for a professional attendance by a sexual health medicine specialist occurs at the point at which a general practitioner makes a clinical judgement that such an attendance is necessary. The current management algorithm and the management algorithm that would apply should the proposed MBS items be listed are summarised in Figure 1 and Figure 2, respectively. 10 Figure 1: Management algorithm that applies currently for sexual health medicine professional attendances 11 Figure 2: Management algorithm that would apply should sexual health medicine professional attendance and case conference item MBS as proposed The above management algorithms that are postulated to apply in the presence and absence of the proposed items are essentially identical except for changes in the remuneration available to sexual health medicine specialists for services currently provided. It is claimed that the current structure for professional attendance items does not adequately reimburse sexual health medicine specialists for the time spent with patients particularly in the case of subsequent consults. It is suggested that the length of consult is driven by the needs of the patient. It is suggested that, in the scenario where the proposed items are included on the MBS, the fee charged can appropriately be related to the duration of the consult, which will be dependent on the severity of patient’s condition and their clinical needs. The AChSHM claim that proposed items better support a stepped model of care (being able to ‘step up’ or ‘step down’ to and from more intense support and treatment when necessary; i.e. from GP to specialist and back again) and appropriately remunerate discussion-based, cognitive specialists for the time they require to meet the clinical needs of patients (e.g. HIV-positive patients with chronic co- morbidities require longer consultations - their care needs do not fit within the existing MBS A3 item structure). It is anticipated that, in the absence of MBS time-tiered items, sexual health medicine specialists with MBS access will continue to claim a range of existing MBS items that currently suit their purposes (e.g. Group A1 ‘General Practitioner’ items and Group A2 ‘Other Medical Practitioner’ items). The proposal acknowledges that there may be some transfer of services from the public to the private sector as a consequence of incentives generated by the listing of the proposed items. The AChSHM estimate that the rate of transfer from the public to the private sector is likely to be in the range of 0.1 to 0.25 FTE per practitioner. 12 PASC noted that the proposal does not take into account any potential expansion of sexual health medicine services that may occur as a consequence of listing the proposed items. However, the proposal noted that the risk of expansion of services in this field is limited as the current number of trainees in sexual health medicine is insufficient to replace the retiring workforce. PASC considered that the assessment report should include an investigation of the likely extent of expansion of availability of sexual health medicine services as a consequence of listing of the proposed items. The proposal presents an alternate diagrammatic representation of the scenarios with and without the proposed MBS items. This diagram is re-produced at Figure 3. Figure 3: Diagrammatic representation of the scenarios with and without the proposed MBS items PASC determined that the appropriate clinical place for the proposed item(s) means that the new items would be used as: (i) a direct substitute for currently available items (such that utilisation of the substituted items will fall as utilisation of the proposed items increases); (ii) a direct substitute for currently available services provided in the public sector; and/or (iii) used to satisfy some previously unmet clinical need. PASC noted that, ideally, information to populate the probabilities in Figure 4 would be desirable. Such information would permit an understanding of the likely switching patterns that would occur should the requested MBS items be made available. PASC agreed that input from stakeholders on potential sources to populate the probabilities in Figure 4 would be desirable. It resolved to seek advice from stakeholders as to potential sources of estimates for: likely rates of transfer from current MBS items to proposed MBS items o likely rates of transfer from services delivered in the public to private sector as a consequence of listing the proposed items; and o 13 likely rates of expansion of the population who will receive treatment from a sexual health medicine specialist as a consequence of listing the proposed items o Figure 4: Diagrammatic representation of management options in the current and proposed scenarios Comparator PASC recognised that the usual definition of the appropriate comparator when considering a request for inclusion of a new item on the MBS was the intervention most likely to be replaced. However, PASC recognised that the proposed application was not requesting listing of a new item but instead sought a change to the current reimbursement arrangements for services currently delivered to patients. The change to the current arrangements would be likely to be associated with an overall increase in average fees paid to specialists. Thus, in the scenario where the proposed items were direct substitutes for the current items, there would be an increase in costs with no associated improvement in outcomes and a determination of dominance of the current scenario over the proposed scenario is a foregone conclusion. Thus, PASC resolved that the usual approach of comparing costs and benefits associated with the current scenario with costs and benefits associated with the proposed scenario was unlikely to be informative for MSAC. An alternate approach of presenting a comparison of the proposed scenario with a hypothetical scenario where there is no delivery of services by sexual health medicine specialists (but which may include delivery of services by others) was suggested by PASC as such an approach would provide information that MSAC could use to make a decision in relation to the cost-effectiveness of the proposed listings. In addition to a comparison of the proposed scenario with a scenario where there is no delivery of services by sexual health medicine specialists, PASC also considered that information should be presented in an application on the likely impact of transfer of sexual health medicine services from the 14 public to the private sector and on the likely impact of the expansion in number of patients that would be treated by a sexual health medicine specialist should the proposed items be made available on the MBS. Clinical claim PASC anticipated that an application considering the comparative effectiveness, safety and costeffectiveness of the proposed sexual health medicine professional attendance and case conferencing items to no availability of such services would claim that: • Patients who are provided with services by a sexual health medicine specialist, compared with patients who are not provided with such services (but who may be provided services by others) experience superior quality-adjusted survival • Appropriate funding (via the listing of the proposed items) for services provided by sexual health medicine specialists is likely to create a financial incentive for sexual health medicine specialists to provide additional services to patients in the private sector and this will have a positive impact to the community overall. On the basis of the likely claims of potential clinical superiority for the proposed items compared with no availability of such items, PASC considered that the application should present a costeffectiveness analysis. However, it also considered that an appropriate economic analysis would also incorporate costs and benefits associated with transfer of services delivered under the public system to the private system and also costs and benefits associated with expansion of availability of sexual health medicine services through the MBS. Outcomes and health care resources affected by introduction of proposed intervention Clinical outcomes The proposal for an application does not specify any clinical outcomes upon which the comparative effectiveness of a scenario where time-tiered professional attendance and case-conferencing items are available should be compared with the current scenario where current MBS items are used to deliver services to patients. PASC considered that stakeholder input should be obtained on what outcomes MSAC might rely upon to make a judgement as to the comparative effectiveness of the proposed services versus no availability of attendances and case conferencing items for sexual health medicine specialists. The PASC also noted that stakeholders should be invited to cite references that would inform the relationship between any surrogate and the final patient-relevant outcome of quality- adjusted survival. Health care resources The proposal for an application notes it would be appropriate for any comparative economic analysis to include the use of MBS resources. PASC considered that other resources besides MBS items might need to be included in an economic evaluation. It resolved to seek further advice from stakeholders 15 on other resources that might be impacted by the availability of services delivered by a sexual health medicine specialist. Proposed structure of economic evaluation (decisionanalytic) Table 2 summarises the extended PICO that it is proposed MSAC would consider. Table 2: Summary of extended PICO to define the question for public funding that assessment will investigate Patients Intervention Comparator Patients who have been referred to a sexual health Time-tiered professional medicine specialist. attendances with a sexual MBS items included in health medicine specialist Groups A1, A2, A3, A4, A8. Outcomes to be assessed Healthcare resources to be considered A metric of clinical MBS items and other “success” will need to be resources that might be defined.and may include impacted by the availability the impact on the health of services delivered by a of the patient partner/s sexual health medicine specialist. MBS items included in Group A15 Time-tiered case conferencing items The proposal for an application did not include a suggested structure for an economic evaluation. PASC suggested that the fundamental structure for the overall economic evaluation of professional attendance and case-conferencing items could be summarised as shown in Figure 5. PASC agreed to seek stakeholder input as to how the structure shown might be advanced (e.g., definition of the term ‘successful outcome’; definition of the services delivered in each branch of the tree shown). PASC also considered that it would be helpful to obtain advice from stakeholders as to how broader considerations besides the impact on a patient’s quality-adjusted survival (e.g., workforce issues, impacts on sexual partners and the sexually active community) could be incorporated into the economic analysis. 16 Figure 5: Fundamental structure for the economic evaluation that might be presented in the assessment of professional attendance and case-conferencing items for sexual health medicine specialists 17