CLINICAL CASE REPORT (“Puzzle”) Mary Grace Gan Chua, MD
advertisement

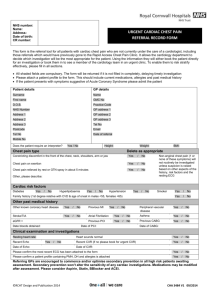
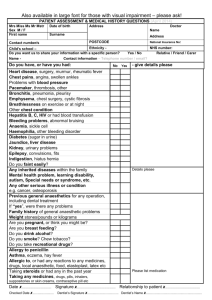
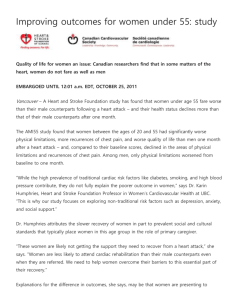
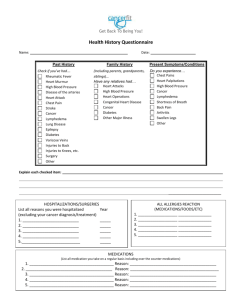
CLINICAL CASE REPORT (“Puzzle”) Mary Grace Gan Chua, MD Introduction: Care and dealing in our patient everyday is like a “JIGSAW PUZZLE”. It is built to last, sometimes fall apart. It is sometimes complicated and hard to figure out. Often times we lose the pieces, and when things get hard, we want to give up. But like a puzzle, when it is formed complete, it is like a work of art, and sometimes it is not what we had expected from the picture on the box. A pleasant morning to everyone. I am Mary Grace Gan Chua, a just turned 2nd year resident, and I will be presenting a clinical case entitled “Puzzle”. Objective: The objective of this presentation is as follows: 1. To present a case of a chest pain in an adolescent with accompanying multiple symptoms 2. To discuss the differential diagnoses for the case 3. To discuss the management of the case using clinical and biopsychosocial approach 4. To formulate a wellness plan for the continuing health of my patient. 5. To share my insight in managing the case. Rationale: I chose to present the case because it highlights the role of the family physician as a clinician and as a counselor in managing a chronic disease in an adolescent age group. Our role as a primary care physician, and work as a team with different specialties. CLINICAL PRESENTATION: Our patient is J.T., a 17 year old female, single, a Grade 12 student, a Born Again Christian, from Binan, Laguna, with no known co-morbidities, seen at the Ambulatory Clinic due to chest pain. 3 days prior to consult, J.T. started to have chest pain, characterized as sharp, pain score of 4-10/10, between 3rd – 5th interspaces, bilateral parasternal area, radiating at the left upper back, usually lasted about 2 hours, intermittent, aggravated by inspiration and mostly when in supine position, slightly resolved by rest. No other S/Sx like chest heaviness, dyspnea, orthopnea, edema, cough, colds, fever, chest trauma and emotional distress. No medication taken. No consult done. 3 hours PTC, above same condition persisted, pain score of 5/10, same character as above, prompted consult at the Ambulatory clinic. For the Review of Systems, it was unremarkable. For the Past Medical History, J.T. was born to a 25y/o G5P4 (4004), full term, physician assisted at Binan Hospital, with regular prenatal check-up and no feto-maternal complication was noted. Was breastfed until 1 year old, and was given complementary food at 6 months of age. Immunization for children was claimed complete care of the Local Health Center. The most recent was Flu shot given July 2014. J.T was breastfed until 1 year old, given complementary feeding at 6months of age. She is not a picky eater. There were no concerns regarding her motor, language, socialization or adaptive behaviors. Currently not known having any illnesses, allergies to food and drugs, surgical operations or hospitalizations. For the Family Medical History, it was unremarkable, except for her mother with hypertension and father who was noted with gallstone and died 6 years ago after his cholecystectomy because of the infection caused by removal of his tubing by accident at home. For the Genogram, noted that she belongs to the 2nd family of his father. The first wife of her father died of Breast Cancer at about age 40’s when her elder 2 half sisters was only 4 and 1 year old. It was already her mother who was taking care of 2 half sisters when they were young and got married to his father blessed with 3 more children, and it is our patient J.T. as the youngest. Currently J.T. lives with her mother together with her 2 half sisters and a brother. The eldest brother was away in Japan working as a factory worker. For the Gynecologic History, Menarche was 12 years old. Regular interval of 28-30 days, lasted for about 5 days, consuming 3 soaked pads/day. LMP was March 14, 2014. No dysmenorrhea, No bloody or purulent vaginal discharge. For the Psychosocial History, J.T. lives with her mother, a brother and 2 half sisters. Father died 6 years ago due to said complication. [Home]The whole family members are in good relationship in each other. She is close to her mother and elder brother. Her mother serves as the breadwinner and works as a child caregiver and sometimes being supported by the elder brother. Nothing in the family she would like to change. [Education] She is a Grade 12 student at University of Manila, Science is her favorite subject, average grade is 87%, no problems with her teachers and classmates, never been suspended or expelled in school, planning to take Accountancy in College. [Activities] She likes to play violin and learned to play it herself and guitar with his brother. Uses internet only for research and Facebook, about 1-2x a month, and rarely watch TV. She stays at home doing household chores. She has 5 female close friends in school. No eating problem noted. [Drugs] She and her friends never tried tobacco, alcohol, and drugs neither sold them. [Sexual] No question about her appearance and is attracted to opposite sex. Never had a boyfriend, never dated and not sexually active. Typical dating for her are 2 couples eating out. No sexual or physical abuse, and never been touched in uncomfortable manner. [Suicide] No episode of extreme sadness, lack of motivation or loneliness. Never had suicidal thoughts or hurt others. [Safety] Patient observes safety precautions in commuting and crossing the street. Not been a member of gang or fraternity. She carries a 3cc syringe as weapon for protection. No firearms in the house. For the Physical Examination, patient is ambulatory, not in cardiorespiratory distress. BP was 110/70, Heart rate was 70, Respiratory rate was 19, Temperature at 36.7, BMI was 18.8 and with a Pain score of 5/10. There was noted point tenderness at the 3rd to 5th costochondral cartilage at the bilateral parasternal area on deep palpation. The chest are symmetrical, no retraction, breath sounds were clear without wheezing. The precordium was adynamic, with regular rate and rhythm, no murmur. Sexual maturity rating was appropriate. The rest of the PE Findings were unremarkable. Salient Features: We are presented a 17 year old female student, with a 3 day history of sharp bilateral parasternal chest pain radiated at the left upper back, resolved by rest and aggravated by inspiration, with no noted comorbidities. On Physical Examination there was point tenderness between 3rd and 5th bilateral parasternal costochondral area on deep palpation. Differential Diagnosis: Chest pain among adolescents, according to Pediatrics in Review, the official journal of the American Academy of Pediatrics dated January 2010, is not usually caused by serious diseases. It is second only to heart murmur for referral to a pediatric cardiologist. About more than 98% of chest pain is non-cardiac in origin, musculoskeletal or chest wall pain being the most common with a prevalence of 15-31%. The etiology of chest pain is categorized as Cardiac vs. Non-cardiac. This table 1 shows the Cardiac Causes of Chest Pain in Pediatrics, subcategorized to its etiology whether Inflammatory, Metabolic Demand, Coronary Artery Abnormalities, Drug Use, and Miscellaneous structural abnormalities. The next table shows the Non-cardiac Causes of Chest Pain in Pediatrics, subcategorized to Musculoskeletal, Pulmonary, Gastrointestinal and other Miscellaneous causes. Going back to our patient, I ruled out Gastrointestinal , Pulmonary and other Miscellaneous Non-cardiac causes of chest pain like Panic Disorder or Hyperventilation based on our patient’s history and physical examination. I came up differentiating the Cardiac Type and the Musculoskeletal Type of Chest Pain, also based on the Approach to Pediatric Chest Pain taken from Learn Pediatrics, Cardiology Section of the Univ. of British Columbia updated February 2011. This table 3 highlighted our patient’s features of chest pain all corresponds to the Musculoskeletal type of pain, having sharp, radiating, related to activity and inspiration and reproducible by palpation compared to Cardiac type of pain which is crushing, diffuse, heart pounding with tachyarrythmia accompanied by nausea, diaphoresis, syncope and dyspnea, usually exercise related which are all not present in our patient. I ruled out our patient’s chest pain as Cardiac cause and considering it as Musculoskeletal in origin, as supported as well by the epidemiology as been discussed. Among the Musculoskeletal Causes of Chest pain, I ruled out some as causes, like the Slipping Rib Syndrome, Precordial Catch and Xiphoidynia based on our patient’s history and physical findings, example is our patient’s lack of history of trauma, timing, and the location of the pain. Table 4 shows our patient’s features of pain as being compared to other musculoskeletal causes of chest pain, which are Costochondritis, Tietze Syndrome and Muscle Strain. The highlighted features shown all correspond to Costochondritis, characterized with sharp pain in 2 or more contiguous costochondral joints, with no signs of inflammation, and having reproducible tenderness. With the differentials discussed my Assessment was Costochondritis. For my plan I gave Naproxen 275mg/tab BID for 5 days then as needed for pain. I advised passive stretching of the muscles. Watch out it with persistent severe chest pain and dyspnea to go to Emergency room. Follow-up at FMC-OPD after 2 weeks under my service. PROGRESS ON FOLLOW-UP 1ST Follow Up 2 weeks after the initial consult, patient claimed only had 2 episodes of chest pain noted after laughing. She noticed easy fatigability after climbing 2 nd and 3rd floor in the past 2 weeks. She claimed that he had that episode but was year ago after climbing several flight of stairs. No cough and colds, edema, chest heaviness and orthopnea. On PE Findings, patient was tachycardic at 110, with minimal point tenderness at left lower parasternal area. Precordium was dynamic, with regular rhythm, Grade 1 holosystolic murmur. With our patient’s new presentation, of easy fatigability with cardiac findings lead me considering a new disease entity. Table 4 shows the Causes of Fatigue in Children from a journal of the American Academy of Pediatrics, Pediatrics in Review, Adolescent Medicine in 2002. Fatigue is defined as exhaustion after usual activities. Causes may came from several systemic conditions. Based on our patient’s clinical features and physical examinations, other systemic causes were ruled out like the Connective tissue, Endocrine, Gastrointestinal, Genitourinary, Granulomatous, Hematologic, Infectious, Neurologic, Otolaryngologic, Pulmonary and Psychosocial disorders, due to lack of other supporting symptoms and findings pertinent on each disease……(to follow differentials came up to CHF) My working impression was T/C Congestive Heart Failure Class II probably sec. to VHD vs. Cardiomyopathy; Costochondritis, Resolving. For the plan, 12 lead ECG was requested to see for any cardiac ischemia, irregularities, blocks or chamber enlargement. Chest X-ray was ordered to check for cardiomegaly, bony lesions and parenchymal lung disease that could possibly be present. Ideally 2D echo needs to be done for to see if there is any structural cardiac anomalies. Patient may continue the medication as needed for any recurrence of symptom. 2nd Follow-up Patient has no episode of chest pain, only noted on bending. She claimed with rhinorrhea for 2 days, which she claimed intermittent for 1 month. Minimal nonproductive cough for 1 week. She also claimed had epistaxis, 2 episodes in a day claimed during under warm climate. She also had dyspnea on exertion after climbing 2nd to 3rd floor. On Physical examination, she was tachycardic at 101 and noted with clear watery nasal discharge on both nostrils with minimal crusted excoriation on both nostrils. There was minimal point tenderness on the 5th costochondral area, and same cardiac finding. 12 lead ECG result revealed Sinus tachycardia, Normal Axis, No chamber enlargement. Chest X-ray revealed Pulmonary Arterial Hypertension, Considered. 2D echo correlation may be done for further evaluation, as clinically warranted. My working impression was T/C CHF FC II probably secondary to Valvular Heart Disease, Costochondritis , Resolving, Allergic Rhinitis, Epistaxis? Ruling Out Blood Coagulopathy. For my plan, patient was still for 2D-echo, CBC to check for thrombocytopenia or anemia that might also contribute to her easy fatigability, and PT/APTT as another bleeding parameter. Patient was prescribed with Cetirizine 10 mg/tablet OD and continue Naproxen as needed for pain. Patient was taught to do nasal douching and may follow up under my service once with result. In the interim, Patient texted me if I she could see me in the OPD. I answered yes. She then informed me that she was told that her 2D-echo cannot be performed just and should be referred and seen first by Pediatric Adolescent, then will be referred to Pediatric Cardiologist. I said if that will be the case, I then go referred the patient to Pediatric Adolescent. Pediatric Adolescent Consult She still has rhinorrhea, nasal excoriation, dyspnea on exertion and easy fatigability with new findings of 3 pillows orthopnea and intermittent gum bleeding while brushing teeth. No episode of epistaxis. On PE, she was tachycardic at 105, no murmur (Split S2). Their impression was T/C CHF FC II-III prob. Sec. to Congenital Heart Disease (ASD?) vs Valvular Heart Disease prob sec to Rheumatic Heart Disease; Skin Infection, Anterior Nares. She was reordered to do ASO, ESR, CRP and reordered 12 lead ECG. Treatment was Mupirocin ointment TID on anterior nares and Cloxacillin 500mg/tab every 6 hours then was referred to Pediatric-Cardiology. On 3rd Follow-up, Patient still with easy fatigability, orthopnea and now noted with foul smelling anterior nares wound lesion and absence of chest pain. Cardiac finding on PE was the same. CBC result revealed Hgb=99 Hct=0.32 WBC=9.9 Plt=177, Neutrophil=0.67, Lymphocyte=0.25. PT=14.1 Reference PT=13.1, PT INR=1.1, APTT=33.1 APTT Reference=29. Working impression and plan were maintained and was scheduled for follow-up with laboratory results. In the Interim, Patient texted if she could see me for a check. I replied yes. I went down and saw the patient quickly with some erythematous rashes on lower extremities which seemed like Vasculitis, she claimed happened after intake of Cloxacillin. I requested her to stop taking the medication for now then to see Dermatology for the mean time because I don’t have her chart and needed to go back to my post soon, in my outside rotation. I rescheduled her to an earlier appointment. Derma Consult, Patient was diagnosed with Vasculitis, and was ordered for scheduled Punch Biopsy 4mm/LA with suture and was prescribed with Betamethasone valerate on affected area. On 4th Follow-up, Patient with slight resolution of the crusted lesion on the anterior nares, but now noted with slight erythema on the hands and some rashes on the feet. Vital signs were normal. On PE, still with crusted nasal lesion, now noted with some erythematous, non-blanching, macular to papular lesions, claimed slightly pruritic. Laboratory results for ASO was normal to <200 (NV=<200) and ESR was elevated at 56 (NV=0-20). While the patient is away to claim her 12 lead ECG result, her mother stayed with me for her consult, started crying a bit and asking me if her child was serious. She said that her child is a strong person with a lot of dreams and would like to be like me someday helping the sick. I reassure the mother and advised her to be strong for her daughter and just keep on following up and we will do our best we can for her child. 12 lead ECG revealed Sinus Rhythm, No Chamber Enlargement, Normal Axis. At that point, I started thinking that our patient presented with multiple symptoms might have a systemic disorder, likely an autoimmune disease. I maintained my diagnosis and now considering Hypersensitivity Reaction probably secondary to Drug Intake (Cloxacillin) vs. Autoimmune Disorder probably SLE. She was still waiting for her scheduled 2D-echoardiography, now advised ideally for ANA testing. I then referred the patient to Immunology Clinic for further evaluation and management. Immunology/Allergy Clinic Consult, Their impression was Allergic Rhinitis; Adverse Drug Reaction to MV by History; Adverse Food Reaction to Tulingan (Urticaria) by History; Anaphylaxis sec to Shrimps; T/C CHF FC II-III prob sec to RHD;PAH Vasculitis prob sec to Autoimmune Disease Ruling in Systemic Lupus Erythematosus. Plan was for ANA, for aeroallergens and food allergen skin test. Prescribed with 1. Levocetirizine + Montelukast 10/5 OD x 2 weeks 2. Fluticasone 50mcg 2 sprays BID 3. Prednisone 20 mg BID x 5 days. Then was advised for Dermatology follow-up and referred to Rheumatology Clinic. Immunology/Allergy Clinic Follow-up, Impression was maintained. Anti-dsDNA was added and resumed the medications except for Prednisone. Her Patch Test Result revealed allergic to Housedustmites and Cockroach and B. isda. Cardiology Consult, Impression was T/C Autoimmune Disorder, possible SLE. Plan was 2D-echo, anti-dsDNA. Plan was no cardiac meds for now. Referred to Rheumatology for evaluation. Follow-up once with 2D-echo result. Cardiology Follow-up, No complaints of chest pain and dyspnea. 2D echocardiography revealed Severe Pulmonary Arterial Hypertension. Severe Tricuspid Regurgitation. Mild Pulmonary Regurgitation. Right Atrial and Ventricular Enlargement. Questionable PDA, R-L Shunting. Anti-dsDNA revealed positive at 18.1 (NV=>15) and ANA is positive at 32 (NV=…). Assessment was Severe Pulmonary Hypertension; Severe Tricuspid Regurgitation, Mild Persistent; Questionable Patent Ductus Arteriosus. Plan was for CT angiography and advised followup. Rheumatology Consult, Assesment was Systemic Lupus Erythematosus (acute cutaneous rash, discoid rash, arthritis, alopecia, serositis, anemia, ANA +, dsDNA+). Plan was for CBC, SGOT and SGPT. She was prescribed with 1.Prednisone 20mg 1 tab BID and 2. Cetirizine + Montelukast 1 tab OD. To start HCQ200mg 1 tab BID if Ophtha cleared. She was then advised to have enough sleep, eat healthy, use sunblock for protection SPF 30, avoid contact to sick individual and wear mask,and exercise. Ophthalmology Consult, Assessment was Error of Refraction, OU; No sign of SLE Retinopathy. No new corrective lenses for patient was satisfied with her current lenses. Advised follow-up after 6 months for evaluation or new onset of blurring of vision. On 5th Follow-up, Patient with no subjective complaints. No noted chest pain, dyspnea, abdominal pain, bleeding signs or rashes, except for colds for 8 days. PE was unremarkable except for noted puffiness of the face, due to steroid intake. CBC now with Hemoglobin of 127 and Hematocrit of .40. AST and ALT revealed normal. [to follow brief discussion or approach to SLE]. My assessment was Systemic Lupus Erythematosus with Pulmonary Hypertenson and Tricuspid Regurgitation. I ordered urinalysis, BUN and Creatinine for baseline renal evaluation. Maintained the drugs prescribed by Rheumatology. I explained the importance of sun protection by applying sunblock and use of umbrella, avoiding stress, and wearing mask. I also explained her condition and asked her if she has any questions or clarifications regarding her illness. I asked her how she feels about her condition and answered she felt normal, except that she has to miss some of her school hours for the hospital appointments but she claimed not actually a problem because her teachers know her condition and was flexible and cooperative with her school schedule especially when she has an appointment. I asked what she has been thinking about her current condition, she said that she was positive and understands her condition. She didn’t feel bad about it, accepted her condition as it is and believes that things are according to God’s plan for us. I asked if there are thing that bothers her, she said that nothing bothers her. She said that praying and family’s support helps her everyday. I commended the patient in her great attitude and perspective and advised her to maintain that outlook and her sickness should not be a hindrance to live in the fullest. I offered my service to her anytime I am available. For my therapeutics, I maintained medications prescribed by Rheumatology and started her on Calcium plus Vitamin D, 1 capsule a day, to avoid brittle of the bone caused by steroid use especially on prolonged use and to avoid Vitamin D deficiency for she is now less exposed to sunlight. I encourage her to have a Pneumococcal vaccine as her protection. Follow-up once with result under my service. For my long term goals, 1.To monitor the patient’s symptoms, compliance and follow-ups with subspecialties. 2. To relieve the symptoms. 3. To let the patient function daily in school and personal concerns. 4. To enroll patient in a support group. 4. To prevent the symptoms and flares. 5. To prevent its complications. For my wellness plan, 1. Vital signs monitoring 2. Vaccination with Pneumococcal and Flu vaccine 3.Regular preventive measures like sunscreen protection 4. Intake of Calcium with Vitamin D daily. My insight in dealing with this case is as a primary physician, everyday is like a puzzle solving. We have to connect the only piece of puzzle available in our hand and patience is a requirement until we get the best pieces of the puzzle that will help us for the whole construction. In doing this, never give up and sometimes asking help is an option, for us to see the brighter outcome. We sometimes think we only have a plain simple puzzle in the start but we would not know until we finish it entirely and surprisingly found that it is a rare splendid one. Last slide (sharing the picture of my patient playing violin after FMC clinic for me, according to her as her gift of thanks last December during Christmas time.)