View the attachment
advertisement
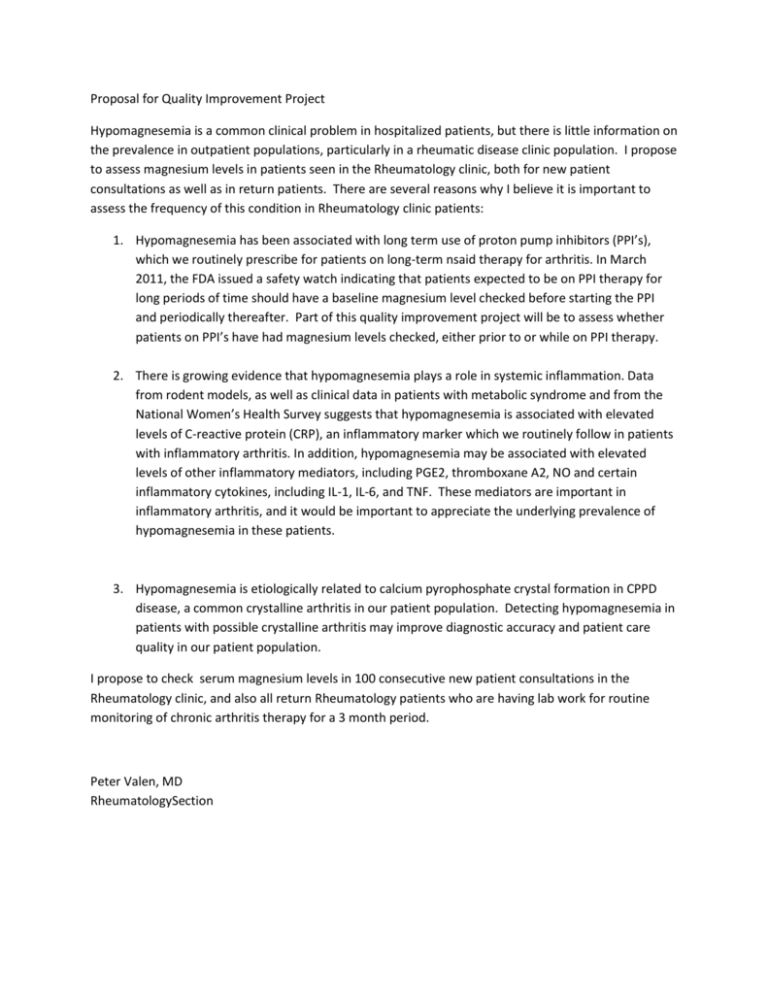
Proposal for Quality Improvement Project Hypomagnesemia is a common clinical problem in hospitalized patients, but there is little information on the prevalence in outpatient populations, particularly in a rheumatic disease clinic population. I propose to assess magnesium levels in patients seen in the Rheumatology clinic, both for new patient consultations as well as in return patients. There are several reasons why I believe it is important to assess the frequency of this condition in Rheumatology clinic patients: 1. Hypomagnesemia has been associated with long term use of proton pump inhibitors (PPI’s), which we routinely prescribe for patients on long-term nsaid therapy for arthritis. In March 2011, the FDA issued a safety watch indicating that patients expected to be on PPI therapy for long periods of time should have a baseline magnesium level checked before starting the PPI and periodically thereafter. Part of this quality improvement project will be to assess whether patients on PPI’s have had magnesium levels checked, either prior to or while on PPI therapy. 2. There is growing evidence that hypomagnesemia plays a role in systemic inflammation. Data from rodent models, as well as clinical data in patients with metabolic syndrome and from the National Women’s Health Survey suggests that hypomagnesemia is associated with elevated levels of C-reactive protein (CRP), an inflammatory marker which we routinely follow in patients with inflammatory arthritis. In addition, hypomagnesemia may be associated with elevated levels of other inflammatory mediators, including PGE2, thromboxane A2, NO and certain inflammatory cytokines, including IL-1, IL-6, and TNF. These mediators are important in inflammatory arthritis, and it would be important to appreciate the underlying prevalence of hypomagnesemia in these patients. 3. Hypomagnesemia is etiologically related to calcium pyrophosphate crystal formation in CPPD disease, a common crystalline arthritis in our patient population. Detecting hypomagnesemia in patients with possible crystalline arthritis may improve diagnostic accuracy and patient care quality in our patient population. I propose to check serum magnesium levels in 100 consecutive new patient consultations in the Rheumatology clinic, and also all return Rheumatology patients who are having lab work for routine monitoring of chronic arthritis therapy for a 3 month period. Peter Valen, MD RheumatologySection