- Royal College of Paediatrics and Child Health
advertisement

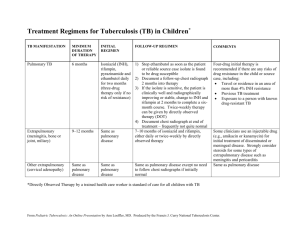
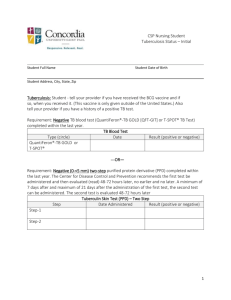
Jinja Regional Referral Hospital Nalufenya Road Jinja Uganda Management of Tuberculosis in Children Title of Guideline (must include the word “Guideline” (not protocol, policy, procedure etc) Guideline for Contact Name and Job Title (author) Dr C Gilhooley Dr J Morgan Dr Namasopo Directorate & Speciality Paediatrics Date of submission Date on which guideline must be reviewed (this should be one to three years) Explicit definition of patient group to which it applies (e.g. inclusion and exclusion criteria, diagnosis) March 2013 March 2016 Abstract This guideline describes the causes, assessment and management of tuberculosis in children Key Words Fever, difficulty in breathing, shortness of breath, pleural effusion, weight loss, cough All children and young people Statement of the evidence base of the guideline – has the guideline been peer reviewed by colleagues? Evidence base: (1-5) 1a meta analysis of randomised controlled trials 1b at least one randomised controlled trial 2a at least one well-designed controlled study without randomisation 2b at least one other type of well-designed quasi-experimental study 3 well –designed non-experimental descriptive studies (ie comparative / correlation and case studies) 4 expert committee reports or opinions and / or clinical experiences of respected authorities 5 recommended best practise based on the clinical experience of the guideline developer Consultation Process Paediatric Clinical Staff Target audience All paediatric staff involved in treating malaria Clinical guidelines are guidelines only. The interpretation and application of clinical guidelines will remain the responsibility of the individual clinician. If in doubt contact a senior colleague or expert. Caution is advised when using guidelines after the review date. Gilhooley Page 1 of 10 March 2013 Jinja Regional Referral Hospital Nalufenya Road Jinja Uganda Management of Tuberculosis Summary This guideline reviews the burden of disease of Tuberculosis (TB) in Uganda and the need for clear diagnosis and management. It also reviews the common organisms causing TB and the different treatment options available. The guideline also aims to look at follow-up of patient to ensure compliance with medication and how to improve compliance. Finally there is a review of contract tracing and its importance in TB. Gilhooley Page 2 of 10 March 2013 Jinja Regional Referral Hospital Nalufenya Road Jinja Uganda Acute Treatment algorithm for Tuberculosis Yes History Cough > 2/52 +/- wheeze Not growing/weight loss Fever >2/52 Exposure to infectious TB Night Sweats No Examination Pleural effusion Enlarged tender LN, especially in neck. Signs of meningitis - Especially if developed over days Abdominal swelling Joint/bone/spine swelling or deformity Yes No Unlikely TB consider alternative diagnosis Treatment for pneumonia/worms/diarrhoea/bacterial meningitis failed. Reconsider diagnosis of TB Airway - ensure if safe. Breathing - Cyanosis – give oxygen - Respiratory distress (indrawing, RR) Circulation - Weak pulse/CRT>3 seconds – consider 10mls/kg fluid bolus - Ensure drinking/BF – if not consider NGT or IV fluids Disability – AVPU and glucose - If AVPU = V,P,U consider TB meningitis and need for LP - Monitor for raised ICP – pupils, eye deviation - If glucose <2.2 give bolus 10% glucose - LP if no contraindications. Exposure - Check skin, bones, joints, spine - HIV positive? Investigations - AFBs – gastric/CSF/pleural/ascetic - CXR - PPD skin test - HIV test Counselling of child and carers Treatment Smear -ve PTB/Non-severe EPTB 2HRZ + 4HR (+ 6 months pyridoxine) Smear +ve PTB/Severe EPTB/Severe concomitant HIV infection/smear –ve PTB +severe parenchymal disease 2RHZE + 4HR (+ 6 months pyridoxine) TB meningitis + TB arthritis 2RHZS + 4RH (+ 6 months pyridoxine) Prednisolone 1mg/kg OD for 1 month Previously treated smear +ve PTB 2HRZES/1HRZE + 5HRE Chronic and MDR TB Specialised regimes – discuss with expert. H = Isoniazid, R = Rifampicin, Z – Pyrazinamide E = Ethambutol S = Streptomycin. Doses on page 7. Gilhooley Page 3 of 10 If on ARVs consider interactions and adjust medications or doses appropriately. If unsure discuss with colleague. March 2013 Jinja Regional Referral Hospital Nalufenya Road Jinja Uganda Introduction Uganda ranks 16th on the list of 22 high-burden tuberculosis (TB) countries in the world. In 2007, the country had almost 102,000 new TB cases, with an estimated incidence rate of 330 cases per 100,000 population. i Causes of Tuberculosis Tuberculosis is common, and in many cases lethal, infectious disease caused by various strains of mycobacteria, usually Mycobacterium tuberculosis,ii a small, aerobic, nonmotile bacillus.iii The high lipid content of this pathogen accounts for many of its unique clinical characteristics.iv It divides every 16 to 20 hours, which is an extremely slow rate compared with other bacteria, which usually divide in less than an hour. v Mycobacteria have an outer membrane lipid bilayer.vi If a Gram stain is performed, MTB either stains very weakly "Gram-positive" or does not retain dye as a result of the high lipid and mycolic acid content of its cell wall.vii MTB can withstand weak disinfectants and survive in a dry state for weeks. In nature, the bacterium can grow only within the cells of a host organism, but M. tuberculosis can be cultured in the laboratory.viii Clinical presentation Most children with TB will present with symptoms such as prolonged cough lasting 2 weeks or more; fever >2 weeks, often associated with poor weight gain; and loss of weight, energy, activity or appetite. Although fever and weight loss are common in children with extrapulmonary TB, the conspicuous symptoms are usually associated with the site of disease.ix Pulmonary In about 90% of cases tuberculosis infection involves the lungs.x,xi Symptoms may include chest pain and a prolonged cough. Any child with a history of cough for more than 2 weeks should be reviewed and investigated for TB. Other common symptoms include night sweats and failure to gain weight or weight loss. About 25% of people may not have any symptoms (i.e. they remain "asymptomatic").ix Extrapulmonary In 15–20% of active cases, the infection spreads outside the respiratory organs, causing other kinds of TB.xii Extrapulmonary TB occurs more commonly in immunosuppressed persons and young children. In those with HIV, this occurs in more than 50% of cases.xiii Notable extrapulmonary infection sites include the pleura (in tuberculous pleurisy), the central nervous system (in tuberculous meningitis), the lymphatic system (in scrofula of the neck), the genitourinary system (in urogenital tuberculosis), and the bones and joints (in Pott's disease of the spine), among others. When it spreads to the bones, it is also known as "osseous tuberculosis". xiv a form of osteomyelitis.ii Sometimes, bursting of a tubercular abscess through skin results in a tuberculous ulcer.xv An ulcer originating from nearby infected lymph nodes is painless, slowly enlarging and has an appearance of "wash leather".xvi A potentially more serious, widespread form of TB is called miliary tuberculosis.xvii and makes up about 10% of extrapulmonary cases.xviii A high index of suspicion is the key to diagnosis of TB in childrenix Suspect TB disease in a child under the following conditions: • History of contact with PTB sputum-smear positive in a child who is 5 years or younger. • Cough of 2 weeks or more • Unexplained prolonged fever greater than 38 degrees Celsius after exclusion or failure of treatment for usual diseases such as malaria or pneumonia • Unexplained loss of weight • Failure to gain weight • HIV infection • Past history of TB treatment Gilhooley Page 4 of 10 March 2013 Jinja Regional Referral Hospital Nalufenya Road Jinja Uganda • Non-response to nutritional rehabilitation after at least 2 weeks of proper nutritional care • Haemoptysis Signs to look for in a physical examination • Severe wasting • Enlarged cervical lymph nodes that may be painful • Swelling (angulation), also known as gibbus, in the middle of the back • Pleural effusion • Progressive deformity of bones or joints First line investigations and interpretation The procedure(s) for diagnosing tuberculosis are usually carried out on patients who have symptoms and have reported to the health facility on their own. After the patient’s history has been taken and a physical exam has been performed, investigations are carried out. In most cases, sputum specimens (1 spot and 1 early morning) are examined for AFB. If facilities are available, patients can also be investigated by culture for Mycobacterium tuberculosis, chest Xray and tissue histology. The investigations and tests useful in the diagnosis of TB are described below: 1. Ziehl-Neelsen stain: Used to examine sputum specimen or gastric aspiration fluid. This is reported as +++, ++, +, scanty or negative. 2. Fluorescence microscopy stain: Another method of identifying the bacilli in the specimen examined. 3. Chest X-ray: Features of chest X-ray consistent with TB disease include miliary picture, pleural effusion and mediastinal lymph gland enlargement with lung infiltration. Although the findings of radiology are nonspecific, abnormalities like any heterogeneous opacities and cavitations, if located in the upper parts of the lung, are more likely to be caused by TB. 4. Culture for Mycobacterium tuberculosis: Although this is the definitive diagnostic test, it is expensive and difficult to carry in the general health service. It will be available only for special situations, such as research and drug-resistant TB. 5. Aspirated serous fluid: Examines pleura peritoneum and pericardium for total protein, cells (total and differential). This test classifies the fluid into exudate and transudate. Exudative fluid is caused most frequently by TB in countries with high prevalence of TB and HIV. 6. Tissue aspirate: Ziehl-Neelsen or fluorescence staining of the aspirate, e.g., lymph node aspirate. 7. Tissue biopsy: Histology examination to see if morphologically the inflammation is diagnostic of TB. In a child it is even more difficult to obtain a reliable sample for culture or histology. When seeing a child with suspected TB it is important to consider the location of the infection and consider investigations appropriate to that location. Possible locations and investigations are outlined below. Gilhooley Page 5 of 10 March 2013 Jinja Regional Referral Hospital Nalufenya Road Jinja Uganda Table 1; sites of possible TB and appropriate investigationix Gilhooley Page 6 of 10 March 2013 Jinja Regional Referral Hospital Nalufenya Road Jinja Uganda Initial management Emergency management Airway - ensure if safe. Breathing - Cyanosis – give oxygen - Respiratory distress (indrawing, RR) Circulation - Weak pulse/CRT>3 seconds – consider 10mls/kg fluid bolus - Ensure drinking/BF – if not consider NGT or IV fluids Disability – AVPU and glucose - If AVPU = V,P,U consider TB meningitis and need for LP - Monitor for raised ICP – pupils, eye deviation - If glucose <2.2 give bolus 10% glucose - LP if no contraindications. Exposure - Check skin, bones, joints, spine - HIV positive? Medications used to treat TB Below is a table showing the different medications used in the treatment of TB and their respective doses in children. Table 2; Anti-TB medications and doses Gilhooley Page 7 of 10 March 2013 Jinja Regional Referral Hospital Nalufenya Road Jinja Uganda Treatment of Tuberculosis Treatment of TB depends of the category of TB. There are 4 categories and each requires different. The 4 categories are outlined below. Table 4: Categorising TBix Table 3: Anti-TB regimes for each categoryix Gilhooley Page 8 of 10 March 2013 Jinja Regional Referral Hospital Nalufenya Road Jinja Uganda Monitoring Health workers providing TB treatment to children should assess progress: at 2 weeks after start of treatment at the end of the initial phase of treatment and monthly thereafter until treatment completion The child should be assessed for symptoms, treatment adherence, adverse events and weight change. Medication dosage should be adjusted for any weight gain. For sputum smear-positive children, sputum should be examined at these points: end of 2 months 5 months during the last month of treatment Chest X-rays are not routinely required for treatment follow-up in children as many children have slow radiological response to treatment, especially those with hilar and mediastinal adenopathy. A child not responding to anti-TB treatment in the first 2 months should be referred for further assessment and management. These children may have drug-resistant TB, unusual complications of pulmonary TB, other causes of lung disease or problems of treatment adherence. Education Parents and children should be made aware of the diagnosis. The background of how the infection was acquired and the need for prolonged medication should be carefully explained. The need for strict adherence to medications should be discussed with the parent/carer and the child. Until effective education and counselling has been achieved anti-TB medications should not be started. Contact Tracing Whenever a child is diagnosed as having TB contact tracing should also be performed in order to ensure all exposed people receive prophylaxis or treatment if necessary. Children who are at risk of exposure should be evaluated for the possibility of having TB. If on review it is felt they have TB they should undergo counselling prior to starting the required anti-TB regime in the treatment section. If after evaluation they are not felt to have TB then they are deemed to be at risk. Children under 5 years or who are HIV positive are deemed to be at risk and should be given 6 months of Isoniazid prophylaxis (see page 7 for doses). Children over 5 years of age do not require prophylaxis. Gilhooley Page 9 of 10 March 2013 Jinja Regional Referral Hospital Nalufenya Road Jinja Uganda Bibliography i USAID 2009. Tuberculosis Profile Uganda. http://www1.usaid.gov/our_work/global_health/id/tuberculosis/countries/africa/uganda.pdf ii Kumar V, Abbas AK, Fausto N, Mitchell RN (2007). Robbins Basic Pathology (8th ed.). Saunders Elsevier. pp. 516–522. Dolin, [edited by] Gerald L. Mandell, John E. Bennett, Raphael (2010).Mandell, Douglas, and Bennett's principles and practice of infectious diseases (7th ed.). Philadelphia, PA: Churchill Livingstone/Elsevier. pp. Chapter 250 iv Southwick F (10 December 2007). "Chapter 4: Pulmonary Infections". Infectious Diseases: A Clinical Short Course, 2nd ed.. McGraw-Hill Medical Publishing Division. v indal, editor-in-chief SK. Textbook of pulmonary and critical care medicine. New Delhi: Jaypee Brothers Medical Publishers. pp. 525. vi Niederweis M, Danilchanka O, Huff J, Hoffmann C, Engelhardt H (March 2010)."Mycobacterial outer membranes: in search of proteins". Trends in Microbiology 18(3): 109–16. vii Madison B (2001). "Application of stains in clinical microbiology". Biotechnic & Histochemistry 76 (3): 119–25. viii Parish T, Stoker N (1999). "Mycobacteria: bugs and bugbears (two steps forward and one step back)". Molecular Biotechnology 13 (3): 191–200 ix Uganda Ministry of Health. MINISTRY OF HEALTH MANUAL OF THE NATIONAL TUBERCULOSIS ANDLEPROSY PROGRAMME. 2nd EDITION 2010. x Lawn, SD; Zumla, AI (2 July 2011). "Tuberculosis".Lancet 378 (9785): 57–72. xi Behera, D. (2010). Textbook of pulmonary medicine (2nd ed. ed.). New Delhi: Jaypee Brothers Medical Pub.. pp. 457 xii Jindal, editor-in-chief SK. Textbook of pulmonary and critical care medicine. New Delhi: Jaypee Brothers Medical Publishers. pp. 549 xiii Golden MP, Vikram HR (2005). "Extrapulmonary tuberculosis: an overview".American Family Physician 72 (9): 1761–8 xiv Kabra, [edited by] Vimlesh Seth, S.K. (2006). Essentials of tuberculosis in children(3rd ed. ed.). New Delhi: Jaypee Bros. Medical Publishers. pp. 249. xv Manual of Surgery. Kaplan Publishing. 2008. pp. 75 xvi Burkitt, H. George (2007). Essential Surgery: Problems, Diagnosis & Management 4th ed. pp. 34. xvii Dolin, [edited by] Gerald L. Mandell, John E. Bennett, Raphael (2010).Mandell, Douglas, and Bennett's principles and practice of infectious diseases (7th ed.). Philadelphia, PA: Churchill Livingstone/Elsevier. pp. Chapter 250 xviii Ghosh, editors-in-chief, Thomas M. Habermann, Amit K. (2008). Mayo Clinic internal medicine : concise textbook iii Gilhooley Page 10 of 10 March 2013