Description
advertisement

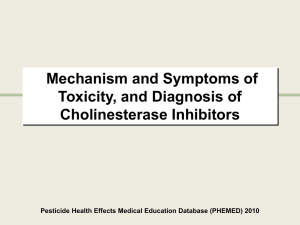
Pesticides Definition & Classification: Pesticides are chemicals that are used to kill pests, basic classes are: Insecticides target harmful or destructive insects: e.g. Organophosphates, organonitrogenous, pyrethroids and organochlorines. Herbicides target weeds: e.g. Chlorophenoxy compounds Fungicides target fungi: e.g. Hexachlorobenzene and Organomercurials. Rodenticides target rodents: Zinc Phosphide Circumstances of poisoning: Accidental poisoning: (a) Among children: can occur when insecticides or pesticides are stored improperly in the home or garage. (b) General population: through the consumption of foodstuffs treated incorrectly with pesticides or harvested prematurely before residues have declined to acceptable levels from contact with treated areas or from domestic use has been reported. (c) Among workers during spraying the trees or during manufacture of the compounds. Suicide attempts: by drinking it as it is easily obtained. Homicidal: by mixing it with foodstuffs. Organophosphate Insecticides (OP): The organophosphates (OP) are a large group of compounds, with the same basic mechanism of acute toxicity. They are esters, amides or thiol derivatives of phosphoric, phosphonic, thiophosphoric or thiophosphonic acids. OPs are used as insecticides in agricultural and domestic settings throughout the world. As nerve agents, they have also been used in warfare and terrorist attacks. Pharmacokinetics: Absorption: occurs via gastrointestinal, dermal, conjunctival and respiratory routes. Metabolism: occurs in the liver, detoxification occurs via cytochrome P450. Excretion of metabolites occurs in the urine. UNIT III CHAPTER 7 Route of entry into the body: For most OP, dermal exposure and subsequent absorption through intact skin represents the most important route of entry in the workplace. The oral route of entry is important in accidental ingestion and deliberate ingestion. Work-related accidental ingestion may occur as a result of poor work practices and lack of personal hygiene. If swallowed, OPs are rapidly absorbed from the stomach. The inhalation route is generally less important. Inhalation of OPs depends on the volatility of the compound, on the type of formulation and on the technique of application. OPs are also absorbed through mucous membranes and eyes, Mechanism of toxicity of organophosphates (OP): In human beings, there are two principal cholinesterases which are: 1- RBC or true cholinesterase (acetylcholinesterase) which is present in human red blood cells, nervous tissues and skeletal muscles. 2- Serum cholinesterase (pseudocholinesterase) which is present in human plasma and in the liver. Normally, the cholinesterases rapidly hydrolyze the neurotransmitter acetylcholine (Ach) into inactive fragments of choline and acetic acid after neurochemical transmission. OPs are irreversible anticholinesterase. The mechanism of action is through the inhibition of the enzyme acetylcholinesterase by phosphorylation, leading to the accumulation of acetylcholine at cholinergic synapses that results in prolonged effect of acetylcholine at a variety of neurotransmitter receptors, including autonomic nervous system (sympathetic and parasympathetic ganglionic nicotinic sites, postganglionic cholinergic sympathetic and parasympathetic muscarinic sites), skeletal muscle system (nicotinic sites), and central nervous system sites, producing first stimulatory and then inhibitory effects. The inactivation of cholinesterase enzymes by OPs occurs in several stages and becomes progressively irreversible after 24 to 36 hours and therefore it is the critical interval during which the antidote can reverse the process. Clinical Picture: (a) CNS manifestations: Stimulant effects: anxiety, restlessness, tremors, confusion, delirium, hallucination and rarely seizures. Depressed effects: coma, depression of respiratory and circulatory centers. (b) Muscarinic manifestations: 1- GIT: anorexia, nausea, vomiting, intestinal cramps, diarrhea. 2 UNIT III CHAPTER 7 2- Salivary, sweet and lacrimal glands: increased saliva, sweating and lacrimation. 3- Ocular signs: miosis and blurred vision, due to cholinergic effect on the papillary constrictors and ciliary body. 4- Cardiovascular system: hypotension and bradycardia. 5- Respiratory system: wheezes and pulmonary edema due to bronchospasm and increased bronchial secretion (bronchorrhea), dyspnea. Pulmonary edema can lead to hypoxia and tachycardia. N.B.1 The muscarinic signs can be remembered by use of the following mnemonic: • SLUDGE/BBB: Salivation, Lacrimation, Urination, Defecation, Gastric upset Emesis, Bronchorrhea, Bronchospasm, Bradycardia. (c) Nicotinic manifestations: 1- Somatic motor manifestations: Muscle fasciculation, cramps and muscle weakness, followed by paralysis and areflexia due to nicotinic stimulation at neuromuscular junction. 2- Sympathetic manifestations: tachycardia and hypertension. N.B.2 Stimulation of nicotinic receptors causes release of adrenaline and noradrenaline, producing symptoms best remembered with the mnemonic MATCH: 1- Muscle weakness and fasciculation. 2- Adrenal medulla activity increase. 3- Tachycardia. 4- Cramping of skeletal muscles. 5- Hypertension. Mechanism of death: Death occurs secondary to respiratory arrest caused by: 1- Respiratory muscular weakness and paralysis (nicotinic action). 2- CNS depression (CNS action). 3- Excessive bronchial secretion and bronchospasm (muscarinic action). Untreated patients usually die within 24 hours, and treated patients who die do so within 10 days. Late death, as long as 15 days after the acute ingestion, may be caused by ventricular arrhythmias. Diagnosis: i- History: patient may give history of working with agricultural chemicals in a closed space, exposing the skin to these chemicals, or ingesting a compound suspected or known to be insecticide. Epidemics occur with contaminated food products, terrorist activity. 3 UNIT III CHAPTER 7 ii- Clinical picture and proper physical examination: Findings depend on the degree of muscarinic, nicotinic or CNS stimulation or depression. Miosis and muscle fasciculations are frequent and reliable indicators of organophosphate toxicity. Also, garlic-like odor may be noted on breath. Typically, the patient presents anxious and diaphoretic, with tachycardia, miosis and excessive salivation. Copious vomiting and diarrhea often occur. Clinical picture was discussed before in details. N.B.3 Note that clinical presentation may vary, depending on the specific agent, exposure route, and amount. Symptoms are due to both muscarinic and nicotinic effects. Vital signs: Depressed respirations, bradycardia, and hypotension are possible symptoms. Alternatively, tachypnea, hypertension, and tachycardia are possible. iii- Diagnostic tests: 1- ECG: may reveal sinus tachycardia initially due to sympathetic stimulation. Then, parasympathetic tone predominates causing sinus bradycardia, arteriovenous block, complete heart block and asystole. 2- Chest radiograph: may show pulmonary edema in severe cases and hyperlucency consistent with bronchospasm and air trapping. 3- Chemistry: (a) Electrolytes: hypokalemia and hyperglycemia. (b) CBC: leukocytosis occur secondary to increased catecholamine release from adrenal medulla. (c) Urine analysis: proteinuria and glycosuria may occur. 4-Toxin-specific test (cholinesterase assays): are helpful for diagnosis and as a guide for treatment. Plasma and RBC cholinesterase levels are depressed in OPs poisoning. Depression of the RBC cholinesterase level is more specific and parallels the activity of cholinesterase. Plasma cholinesterase levels are less specific but are readily available in many hospitals. As a rough guide: 20% - 50% of the normal value is found with mild OPs poisoning. 10% - 20% of the normal value with moderate OPs poisoning. Less than 10% of the normal value in cases of severe OPs poisoning. 4 UNIT III CHAPTER 7 The levels usually decrease to less than 50% before symptoms are seen. Treatment: 1- Emergency stabilization of the ABCs: Airway management with frequent suction of secretion and respiratory support. Intubation may be required to facilitate control of secretion. The patient is placed on 100% oxygen for 1 to 2 hours, then 70% oxygen and a cardiac monitor. An intravenous line is established, and baseline blood sampling and determination of cholinesterase levels should be done. 2-Decontamination: It is carried out according to the route of exposure GIT decontamination: (a) Ipecac shouldn't be used (due to prior repeated vomiting). (b) Gastric lavage with a large bore orogastric tube may be performed with care taken to prevent aspiration as many OPs compounds are in petroleum distillate vehicles which, if aspirated, may precipitate pneumonitis. (c) Activated charcoal is administered unless contraindicated. Dermal decontamination: (a) Removal of clothes by hospital personnel wearing protective gloves and masks. (b) Wash the skin with soap and water. (c) Contaminated clothes should be destroyed. Remove the patients from the polluted atmosphere if exposure is by inhalation. 3-Antidotal therapy: concomitant atropine and oximes. (a) Atropine: A competitive antagonist of acetylcholine at muscarinic sites, it is a tertiary amine that crosses the blood-brain barrier. Thus, atropine treats the muscarinic effects and possibly the CNS toxicity of OPs. Dose for adults: 2 to 4 mg, intravenously. Dose for children: 0.05 mg/kg If no effect is noted, this dose is doubled every 5 to 10 minutes until dryness of trachea-bronchial secretions. Pupillary dilatation is not a therapeutic end point. (b) Oximes (Pralidoxime = Protopam = “2-PAM” and Obidoxime = toxogonin): Pralidoxime “2-PAM” is a quaternary amine oxime, which can regenerates acetylcholinesterase. It works by attacking the phosphate moiety of the OPscholinesterase complex, forming an oxime-phosphate, which lifts off the enzyme, freeing it for normal activity and also detoxifies the remaining OPs. Thus, 2-PAM reverses nicotinic, muscarinic and CNS effects of OPs effects and 5 UNIT III CHAPTER 7 OPs- related muscle paralysis. It should be given within 24 to 36 of acute exposure before" aging" of enzyme Dose for adults: 1 g (Pralidoxime, 2-PAM). Dose for children: 20 to 40 mg/kg (Pralidoxime, 2-PAM). Oximes are given by intravenous infusion in normal saline over 30 minutes every 6 hours for 24 to 48 hours, or until signs and symptoms resolve. Response usually occurs within 10 to 40 minutes of administration of concomitant antidotal therapy. 4- Symptomatic treatment: Seizures: can be controlled by diazepam. Hypotension: normal saline. Pulmonary edema and bronchospasm: Oxygen, intubation, positive pressure ventilation. 5-Disposition and follow up: Mild toxicity requires only decontamination and observation for 6 to 8 hours but all significant toxicity requires admission to the intensive care unit. Patients, who ingest OPs intentionally, should undergo psychiatric evaluation and counseling. Workers shouldn't be re-exposed to OPs until acetylcholinesterase levels are more than 75%. Organonitrogenous insecticides (Carbamates) Carbamates Carbamate insecticides are derivatives of carbamic acid. They are widely used in homes, gardens and agriculture. e.g. Aldicarb (temik), carbaryl (sevin), propoxur (baygon) and methomyl (Lannate) Mechanism of action: Like organophosphate pesticides, but carbamates reversibly inhibit acetylcholinesterase and plasma pseudocholinesterase. They hydrolyze spontaneously from the enzymatic site within 48 hours. They cause increased activity of acetylcholine at the nicotinic and muscarinic receptors. Carbamates poorly pass BBB & thus have less CNS effects. The clinical presentation Carbamates toxicity is typically as muscarinic and nicotinic manifestations of OPs (cholinergic crisis of OPs) but with less CNS toxicity without seizures and a short duration of action. 6 UNIT III CHAPTER 7 Treatment: (a) Emergency stabilization and decontamination measures are the same as OPs. (b) Antidotal therapy: Atropine is the antidote of choice. N.B.4 Oximes in carbamate poisoning is generally not recommended. However, as early differentiation between OPs and carbamate toxicity is difficult, it is recommended that oximes be started in any syndrome consistent with these toxins unless OPs exposure is ruled out. Pyrethrins Sources and forms of toxins: Pyrethrum is a natural compound extracted from the chrysanthemum flower. Pyrethrum contains six active compounds called pyrethrins. Pyrethroids are synthetic derivatives of the pyretherins. Many of these compounds are mixed in petroleum distillates which can produce a hydrocarbon chemical pneumonitis. These agents are used commonly as aerosols in automated insect spray in public places; therefore, inhalation is the most common source of exposure Mechanism of toxicity: In human, these compounds produce cutaneous and inhalational allergic reactions. Clinical presentation: History: patient may give a history of insecticide exposure. Physical examination: 1-skin: erythema, vesiculation and mild paresthesias. 2- Pulmonary: upper airway irritation (rhinitis, throat irritation, oral and laryngeal edema) and lower airway reactions (cough, wheezing and chest pain). 3- GIT: nausea, vomiting, diarrhea and abdominal cramping can occur with both oral and inhalational exposure. 4- Neurological: CNS excitation, tremors, incoordination and paralysis. Seizures may occur with massive ingestion. Laboratory tests: no specific laboratory tests are indicated. Management: 1- Removal from exposure. 2- The patient usually not needs hospitalization. 3- Supportive therapy: should be administered based on the symptoms and signs. Vitamin E oil applied dermally to relieve paresthesia. 7 UNIT III CHAPTER 7 4- GIT decontamination: is not indicated unless the patient ingested more than 1 g/kg of the poison. If GI emptying is indicated, either emesis or lavage, the placement of a cuffed endotracheal tube is necessary. 5- No specific antidotal therapy. Rodenticides Rodenticides are defined as any substance that is used to kill rats, mice, and other rodent pests. It may be classified in several ways but the most medically useful of classifying them is by toxicity: 1- Highly toxic rodenticides include: thallium, sodium monofluoroacetate, strychnine, zinc phosphide, yellow phosphorus and arsenic. 2- Moderately toxic rodenticides includes: α-naphthyl-thiourea and cholecalciferol (vitamin D3). 3- Low toxic rodenticides includes: red squill and warfarine-type anticoagulants. Anticoagulant rodenticides The toxicity of anticoagulant rodenticides depends entirely on repeated exposure to relatively small doses. This is true for both rodents and humans. All the anticoagulant rodenticides act by interfering with the synthesis of vitamin K which is essential for normal blood coagulation. Hemorrhage is the most frequent encountered complication from anticoagulant poisoning. Warfarin poisoning can cause spontaneous bleeding, usually from the nose, gums as well as the gastrointestinal and urinary tracts. Hemorrhage into the skin and brain can also occur, but this is less common. Treatment consists of activated charcoal and vitamin K1 orally at a dose of 5 mg in children and 20 mg in adults two or four times daily. Zinc Phosphide Mechanism of toxicity: Zinc phosphide is an inorganic compound, with typically a dark grey crystalline appearance. The toxicity of zinc phosphide results from the liberation of phosphine gas when it ingested following a hydrolytic reaction with water in the stomach; phosphine (which is a cytochrome C oxidase inhibitor) acts rapidly to cause widespread cellular toxicity with necrosis of the gastrointestinal tract and injury to liver and kidney if ingested and to the lungs if inhaled. Clinical picture: C.N.S.: Headache, fatigue, ataxia, coma and seizures. 8 UNIT III CHAPTER 7 G.I.T.: Nausea, vomiting (black vomitus), epigastric pain with a fishy breath. The symptoms are due to GI irritation or ulceration. Hepatic: Centrilobular necrosis (hepatic), jaundice. Neuromuscular & skeletal: Paresthesias, intention tremor. Ocular: Diplopia. Respiratory: Non-cardiogenic pulmonary edema, cough, dyspnea. Myocardial toxicity: Shock and dysrhythmia. Endocrine & metabolic: Metabolic acidosis, hypocalcemia and tetany. Treatment: The management of zinc phosphide poisoning is mostly supportive and symptomatic. 9 UNIT III CHAPTER 8 86