CSRC-GBAR 11/15/2014: Santa Clara Valley Medical Center
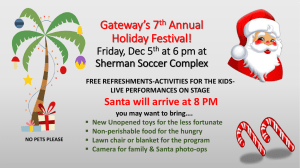
advertisement

CSRC-GBAR 11/15/2014: Santa Clara Valley Medical Center Meeting started 09:10 Introductions 9:10 – 9:18 AM Announcements Since our last meeting, another important piece of legislation was approved: SB 850. This allows for a pilot program in which community colleges can award a baccalaureate degree. There are 72 districts, and only 15 will more forward for the pilot. (Ray) Respiratory Therapy programs for Napa, Ohlone, Skyline, and Modesto have support from their Districts to participate in the Community College Baccalaureate Degree pilot program. Butte Glen chose Product Process Technology. Coast College chose Community Corrections. Grossmont is putting forth Environmental Health and Safety Management. Los Rios is still deciding. Crafton Hills has not decided but is considering Respiratory Therapy. State Center has decided on Dental Hygiene. Letters of intent submitted to the state were due November 12th. Pilot programs must start by 2017 or possibly earlier. We hope to have at least one Bay Area RT baccalaureate degree approved for participation in the pilot. The 30 CEU requirement for maintaining RCP licensure has been approved by the Respiratory Care Board; we are currently at 15 CEUs. Come January 2016, all RTs will have to complete 30 credits in two years to keep their licenses. Suggestion to add 1 CEU per GBAR meeting – will be considered as a means of making GBAR more attractive to current practitioners and for adding an education component to the regional meetings. Bob Bence will lead Government Affairs Committee: This committee is seeking members. Membership Committee is also seeking members Ebola: CPMC and UCSF are the Ebola Regional Centers but all local hospitals need to be prepared for Ebola to keep patients for a couple days. Contra Costa Regional Medical Center, Martinez, CA. To prepare for Ebola, they gather daily updates from CDC and daily monitoring of temperatures. CEO/Public Health Officer send out county wide updates – have changed donning/doffing procedures 2 or 3 times because they continued to improve the way they did donning and doffing. They are changing how ambulances bring patients in, where they are placed, etc. Some hospitals, per George, are sending patients directly to UCSF (Mount Zion) or UC Davis rather than training their employees to work with Ebola patients. He suggested that RTs watch 60 Minutes episode about Texas RNs taking care of Ebola patients. Most hospitals will not see these patients but, per George, not preparing front line people like RTs is not the CSRC-GBAR 11/15/2014: Santa Clara Valley Medical Center best decision. Paul Barraza is at a County facility – they have been preparing both Level I and Level II gear. Level I staff are in the ‘warm zone’; they will hand things off but not touch the patients. Initially, only RNs and MDs were trained then the decision was made to have RTs take care of patients on ventilators. When a patient is admitted, blood work is sent to LA (24 hour turnaround time). If test is positive, it’s sent on to CDC in Atlanta for 72 hour turnaround time. After a positive test, the infected patient could be sent to a designated center; however, if UCSF’s 2 beds are full , the patient will not be able to be sent there. Only a handful of beds are available at the state level; consequently, patients would need to stay at that hospital facility. The link to new Cal/Osha guidelines mentioned (Grey): http://www.dir.ca.gov/dosh/documents/Cal-OSHA-Guidance-on-Ebola-Virus-for-Hospitals.pdf REGIONAL REPORTS East Bay (Michelle): Kaiser RNs went on strike for 2 days this week due to feeling unprepared for Ebola (needed more training). Sutter is reducing from 6 supply chain regions to 2 regions in spring 2015. Covidien was acquired by Medtronic. CareFusion, known for EtCO2 modules which are becoming more and more common throughout hospital areas, was acquired by Becton Dickinson pharmaceutical company. Hep C is a growing concern with healthcare providers and the need for proper PPE via gloves/handwashing/N95 masks is very important. Kaiser Fremont is advertising for a Manager of Pulmonary Clinical Services. Monterey Coast (Tanya): Natividad went live as a trauma center. SVMH (Salinas Valley Medical Hospital) is looking for a supervisor position and St. Luis has not finalized the deal with Prime Health Care as of yet. Mechanical Ventilation Seminar on November 6 th had many Hartnell College attendees. North Bay (Jim/Kate): Sutter Santa Rosa moved into a new hospital – this is a huge, exciting thing and many grads from Napa work there so it’s great. There was an Open House for a simulation lab in Fairfield; the woman who developed it is a cardiologist/former trauma surgeon envisioning a full simulation hospital in Fairfield. She is a visionary and is working to make this happen in the future. Sonoma Valley Hospital was awarded one of the 15 safest hospitals in the US by Consumer Reports. Doctor’s Hospital in San Pablo faces possible closure. South Bay (Karsten): Good Samaritan Hospital continues to look for a director. Kristen Merriman (former Good Sam Director) took a position as lead RCP at Stanford Health Care. Stanford is currently hiring for 7 PRN positions. Sutter (PAMF) Santa Cruz is advertising for a full time day position. Sequoia is advertising for a PRN pulmonary rehab tech. Lucile Packard is hiring for equipment tech and relief positions. Kindred Health Care in San Jose is hiring full time. Apria Health Care, Menlo Park, is hiring a branch coordinator. Stanford Health Care hosted a Respiratory Care Conference on October 23rd with 80 people in attendance. Many attendees CSRC-GBAR 11/15/2014: Santa Clara Valley Medical Center were students from Foothill, Skyline, Ohlone and Napa Valley Colleges. Twenty-five RCPs representing Santa Clara Valley Medical Center, Kaiser, Lucile Packard, and Stanford were also in attendance. Four CEUs were offered; Stanford looks forward to another conference to be held in 2015 with more speakers and a larger audience. West Bay (Theresa): Mission Bay UCSF is due to open Feb 1, 2015 and this is for L & D, cancer center, and neonatal/pediatrics. The General: Dec 5 2015 is open date for new hospital; they are doing Ebola/PPE training. Two years of adult care post-graduation is required to be an MGA registry member; the registry is currently seeking practitioners. ACCS credential worked on via many staff – Mark Siobal. He has retired after 35 years of excellence in his respiratory career. He is known as a man who wore many hats at the facility. Joseph Booze has been hired as his replacement for RCS Equipment Manager. Eula Lewis, the RCS Outpatient Coordinator, has been promoted to RT III Classification. CPMC: The new building at Cathedral Hill opens in 2019 as well as St. Luke’s. Ebola training has been completed and quarantines will be held at Marshall Hale, across the street from California Campus. Seton may be purchased by Prime Health Care with deadline in January; if not purchased by Prime Health Care, the new deadline is June for purchase. Kaiser Redwood City is moving across the street to a new facility. EDUCATION COMMITTEE: On October 23, 2015, UCSF is holding a conference on transitional research. This is a look at how basic science research is being translated into patient care. For instance, RTs learn about mucolytics in school. Acetylcysteine is being shown to be more effective than Dornase Alfa in breaking down mucus; this has been researched for a paper written by UCSF. There is exploration of giving mucomyst a saccharine base and pairing it with a beta adrenergic as a new approach in mucolytics. This conference will be mostly focused on adults; their research center has a rheometer, a ‘floating table’. GBAR/KETTERING ACCS conference was a success with 35 attendees with President Michael Madison and Abbie Rosenberg. They sent out surveys and results are pending on attendee satisfaction. This event made a profit, $400 or so. Next Kettering Seminar with CSRC will be paired with NPS. SOCIAL COMMITTEE: This cost for Lungapalooza was over $800 which covered the food; the date will be amended next year so all schools will have a better attendance record. This was the highest grossing prize for the Chili Cook Off, $375.00. The social committee has been planning the winter event; there is some interference with holidays. They are considering a January event as a scavenger hunt or a hike. The attendees at today’s meeting had some interest in doing a CSRC-GBAR 11/15/2014: Santa Clara Valley Medical Center volunteer event for the holidays, such as at a Food Bank or a soup kitchen. Skyline College is going to the SF Food Bank November 26th to prep food for Thanksgiving meals. All are welcome to join them for this event at the SF Food Bank. Michelle volunteers at Martin de Porres, a soup kitchen on Portrero Avenue: http://www.martindeporres.org/ Many facilities want you to be trained before coming in on a holiday; Michelle was able to help at Martin de Porres and continues to do so once/month, without prior training. Theresa suggested volunteering and promoting CSRC-GBAR by working in a kitchen or a wrapping party or any type of charitable events. To help people not just in the hospital but in the community is worthwhile; our career is based on helping other people – to extend this outwards would be valuable. This is a no cost type of event that would have innumerable, incalculable benefits. Second Harvest is another great place to volunteer for the holidays. Foothill College has the Medical Brigade; two of their RT students went to Honduras this year and hope to have more students involved in the future. (Janyth). November is COPD, Lung Cancer awareness month and also the Great American SmokeOut on November 20th. The RTs at Contra Costa Regional Medical Center and Health Centers will be providing the public quit smoking tips, device usage and disease education. She has 3 clinics that she wants to pair with students. This will be from 0800 – 1500 Monday – Friday next week. Please contact her if you’re interested in volunteering in Honor of the Great American SmokeOut. Janyth Bolden (email: janyth.bolden@hsd.cccounty.us) or call Odessa Lefrancois (925) 813-8020. Break from 10:25 – 11:00 AM Tahoe Committee: This event is March 4 – 6th 2015. With nine talks, two small-group intensives, two gourmet buffet dinners, two phenomenal buffet breakfasts, drink tickets, raffles, a plethora of vendors and so many CEUs to be had, this is not an event to be missed. Everyone needs to mark his or her calendar and plan to attend. Student registration is under $150! With so many CEUs, new products, networking opportunities and after-hour parties, plan to attend theTahoe Conference 2015: Summit at the Summit. Sputum Bowl Committee: Students who are participating will have to compile and create 30 – 60 questions per school. These will be brought to the table so there is some mixing up of the topics. They will switch up the seeding; there may be changes to the seeding with a random drawing. This will change the tournament format and have single elimination. It has taken 2.5 days for the Sputum Bowl to be completed at state and this is being paired down to 1 day only for Sputum Bowl in a Round Robin format. There is an effort to make more parity in the question setup and only 6 regions. State competition is June 1 – 3 so the regional competition will be held before that (April or May at the latest). There is some interest in a practitioner competition available, as well. Student Reports CSRC-GBAR 11/15/2014: Santa Clara Valley Medical Center Foothill: They hired able a Director of Clinical Education who starts December 1st; it’s a huge help. Josh Forsling has teaching and clinical experience. Students have 27 first years and 26 second years; they had Respiratory Care Week with Spirometry and wheel with prizes as well as table for Great American Smokeout. Students got NRP certified and start NICU orientations shortly. Hartnell: They have 9 second year students and 12 first year students. They just started clinical rotation in San Luis Obispo at Sierra Vista. They are excited to get going for Sputum Bowl and are not likely to go to Las Vegas National Conference. Napa Valley: They have 26 first years and 23 second years. They participated in the Great American Shakeout for events regarding the earthquake. They made kits and taught how to do hands-only CPR and were also involved with Respiratory Care Week – over 100 were trained in CPR. Last week, they were at the American Lung Association Walk with a great showing. Not many are going to Vegas because this event is held the week before final exams. They have a distance education partnership with Santa Rosa JC; the distant education program is going through some transitions. They’re applying for Bachelor’s proposal and are hopeful that either Napa College, Ohlone or Skyline will get that… in January, they will find out who will get it. Asthma Institute will have annual conference (held in March 12 – 13, 2014) in Oakland for people who want to do a 2-day course to take the Asthma Certification Test; CEUs are available through CSRC for this course. Ohlone: Second-year class includes 17 students who are finishing Neonatal/pediatric rotations. Last semester is ICU rotation/critical care. Sputum Bowl is practicing with Tom Wagner as the coach. Respiratory Care Week featured displays/tables in the central foyer which included PFT and intubation mannequin, free pizza, with good participation between first and second year students. For first years, they have 20 people in their class; they’re finishing up first semester and are finishing first clinical rotation of once/week 5 hours per shift. There will be an event in March with Lung Association, likely another walk. Skyline: There are 27 first year students and 20 second year students. During Lungapalooza, they won the Chili Cookoff. They also won the balloon carrying game and the tug of war. All of the second year student class minus one person is going to the AARC Conference. They’re fundraising through different organization and have accumulated several thousand dollars for the conference. They strive to be academic and to have fun, as well. November 26th they go to San Francisco Food Bank and will organize food for needy families in the City. There are a few spots available for volunteering if anyone wants to join their group. November 20th is their Health Fair event date. CSRC-GBAR 11/15/2014: Santa Clara Valley Medical Center Day on Capitol Hill: February 9, 2015 – This is an important opportunity to be involved with moving legislation forward on Capitol Hill in Sacramento. Attendees will first meet with Aaron Read & Associates, our legislative advocate. Following this, Assemblyman Brian Jones, who sponsored AB 1972 (RRT minimum for licensure in CA), will be given an award with a photo-op on the stairs of Capitol Hill for all those in attendance. We will then break up into smaller groups and go to legislator’s offices to talk with representatives. Due to term limits, there will be many new faces beginning January 1st….and we need to educate them about our profession. There will be more details coming out on how to become more involved with the profession and its movement forward on a state level. Depending on the number of interested individuals, The CSRC may rent buses to go to Sacramento. Please contact Ednalee Warnecke at ewarnecke@csrc.org to reserve your spot now! Paul Barraza, Clinical Educator at Valley Medical Center: Adjunct faculty at Foothill College and he was impressed with how large the GBAR meeting was at VMC. He has been an employee for 20+ years – VMC is the County hospital for Santa Clara and started in the 1860s, one of the oldest facilities in the Bay Area. They are licensed as a 750 bed hospital, regional burn center, Level 1 Trauma, Level 3 NICU as well as 7 different ICUs. They are a primary stroke center and teaching facility affiliated with Stanford and some Kaiser Residents. Construction of the new facility begins 2016 and RTs will be in the basement, once again. They are the hospital with the graveyard so in the late 1800s/1900s, they buried them out back behind the hospital. They unearthed 600+ graves when parking lot construction began; this slowed down construction for more than one year. RT Department – 90 RTs with 11 – 14 therapists per shift, quite busy. US News World Report considered this to be one of the top two hospitals in the Bay Area. The RT department was awarded one of the top 10 in the country. They have an incredible amount of equipment, doing anything and everything that is out there. Also, they have one of the most active high frequency programs in the state. In February, went to Newport Beach ALA did the COPD Educator’s program. Eight RTs will be going to the Oakland conference, as well. COPD Program: It’s an exciting yet frustrating program. With new Medicare Program and the penalties from excessive readmits in COPD October 1, 2014 this year, the number of times people are readmitted to the hospital will be tracked. The VMC program focuses on home care and training within the hospital to cut down admissions and readmissions. The multidisciplinary team includes: RN, MD, RT, social workers, PT, dietary, language services, case management, out-patient PFT, smoking cessation. Sandi Wong used COPD GOLD standard among several national standards as well as VMC’s Assess and Treat Protocols to help create the program. A future goal includes adding corticosteroids to the bronchodilator protocol. A COPD Educator goes through a patient’s smoking history, inhalation/particulate, personal history, etc. It’s a long process, often 45 minutes or longer than an hour to do a patient assessment. Currently, they use peak flows for all COPD patients but want to move to CSRC-GBAR 11/15/2014: Santa Clara Valley Medical Center spirometry. A major goal includes teaching patients to take care of themselves and to monitor themselves. Educators don’t want patients to wait for the ER visit; it has been a real learning curve to get patients to move away from an ER-based approach rather than monitoring selfcare. A second goal includes getting the patient to have spirometry testing so they have a baseline number before discharge from the hospital. Smoking cessation part is another component of the COPD program. Even if patients are not willing to stop smoking, educators try to get COPD patients to wear a nicotine patch. By getting patients a patch, they are more able to listen and to consider alternatives. COPD educators use the End Check Dial which uses low range inspiratory flows as the metric. The End-Check Dial gives a solid number to know whether patient is receiving the inhaled medication or not. The Better Breathers Club meets once/month (affiliated with ALA). It’s a small group of patients and their families who come to VMC; Gail and her team enjoy seeing them at the meetings. Another component of the program includes making phone calls to patient’s homes within 2 weeks of discharge as a follow-up. One problem to overcome was the home follow-up care. Medical and Medicare are complex entities; the patient must have the proper medication but every level of insurance has medicines that approved and/or not approved. If a patient’s insurance doesn’t cover a particular medication, the pharmacy could not make substitutions. Now, VMC has instituted a transitional care approach; the pharmacy can come to bedside and make appropriate pulmonary medicine substitutions. The ultimate goals are to formulate and maintain a multidisciplinary program dedicated to a commitment to excellence in providing COPD / Asthma Chronic Care services in a comprehensive manner and to reduce the readmission rate of COPD / Asthma patients (primary diagnosis).