Supplemental Digital Content CPT and ICD
advertisement

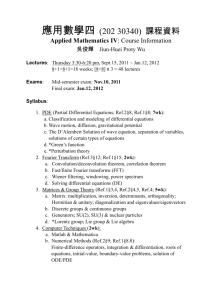
Supplemental Digital Content 1. CPT and ICD-9 codes used in study 2. Hierarchical model development and calculation of reliability 3. Table of fixed effect odds ratios and between-hospital variance for each model 1 Supplemental Digital Content 1 - CPT and ICD-9 codes used in study Colorectal procedures were identified using the following CPT codes: 44140, 44141, 44143, 44144, 44145, 44146, 44147, 44150, 44151, 44155, 44156, 44157, 44158, 44160, 44204, 44205, 44206, 44207, 44208, 44210, 44211, 44212, 45110, 45111, 45112, 45113, 45114, 45116, 45119, 45120, 45121, 45123, 45126, 45130, 45135, 45160, 45395, 45397, 45402, 45550 Postoperative diagnosis groups included the following ICD-9 codes: Diagnosis group ICD-9 codes Diverticulitis 562.11, 562.13, 562.01, 562.03 Diverticulosis 562.10, 562.12, 562.1, 562, 562.00, 562.02 Fistula 596.1, 569.81, 619.1, 998.6, 565.1, 537.4, 619, 599.1, 619.8 Hemorrhage 578.9, 578.1, 569.85, 569.3, 578, 532.40, 534.40, 569.86 Infectious enteritis/colitis/peritonitis 003.0, 008.4, 008.45, 009.0, 009.1, 569.5, 540.1, 567.22, 540.0, 540.9, 567.9, 567.21, 567.29, 540, 542, 567.89, 541, 567, 567.31, 569.61 Inflammatory bowel disease (Ulcerative colitis and 555, 555.0, 555.1, 555.2, 555.9, 556, 556.0, 556.1, Crohn’s disease) 556.2, 556.3, 556.4, 556.5, 556.6, 556.8, 556.9, 558, 558.1, 558.2, 558.3, 558.9, 567.82 Benign neoplasm 211.3, 235.2, 211.4, 230.3, 239.0, 569.0, 230.4, 238.1, 211.2, 239, 209.57, 215.5, 235.5, 229.8, 230.5, 209.52, 209.60, 211.1, 211.8, 227.0, 228.1, 229.9, 235.3, 238.79, 238.8, 239.7, 239.8, 209.50, 209.53, 209.69, 211.5, 211.7, 211.9, 214.2, 215.6, 217, 230, 235.4, 236.3, 238.9, 214.3, 209.51, 209.43, V12.72, 214.8 Malignant neoplasm 154.1, 153.6, 153.3, 153.4, 153.9, 154.0, 153.1, 153.0, 153.2, 153, 153.7, 153.8, 154, 154.8, 197.5, 153.5, 197.6, 209.03, 154.3, 154.2, 152.2, 197.4, 209.11, 158.0, 202.83, 198.89, 183.0, 202.80, 209.12, 152.9, 171.5, 151.8, 157.2, 197.7, 199.0, 199.1, 209.13, 259.2, 158.8, 196.2, 209.16, 151.9, 157.0, 158.9, 195.3, 198.6, 209.17, 152.8, 156.0, 157, 159.0, 171.9, 174.9, 182.0, 195.2, 200.70, 209.00, 209.15, 150.9, 151.2, 151.3, 151.4, 152.0, 156.1, 157.1, 158, 159.9, 170.6, 171.6, 179, 184.4, 185, 188.9, 189.0, 194.0, 197.8, 198.5, 200.10, 202.03, 203.80, 209, 209.10, 209.29, 209.72, 150.2, 151, 151.6, 152, 152.1, 155, 155.0, 157.9, 161.1, 162.3, 162.9, 172.5, 173.9, 174, 182, 188, 188.8, 193, 195.8, 196.5, 198.82, 200.03, 200.2, 200.23, 200.33, 200.43, 200.7, 202.13, 202.8, 202.87, 202.93, 209.0, 209.01, 209.14, 209.27, 209.3, 209.30, 209.79 Obstruction/perforation 560.0, 560.8, 560.81, 560.89, 560.9, 569.83, 560.2, 552.21, 560, 550.10, 552.8, 552.1, 552.2, 550.0, 551.21, 552.29, 532.50, 537.3, 550.00, 550.11, 551.2, 552.00, 552.20, 532.10, 551.1, 551.8, 552.3, 552.9, 532.11 Rectal prolapse 569.1 Vascular insufficiency 557.0, 557.1, 557.9, 557 2 Supplemental Digital Content 2 – Hierarchical model development and calculation of reliability John L. Adams, Ph.D. We developed hierarchical multivariate logistic models for superficial SSI, deep/organ-space SSI, and “any SSI,” with hospital entered as a normally distributed random intercept: pij 0i 1 X ij ln 1 p ij pij is the probability that person j in hospital i will have an infection. X ij is a vector of person level covariates. 1 is a vector of fixed regression coefficients corresponding to the person level covariates in X ij (e.g. demographics). 0 i is a hospital level random intercept: Where 0i ~ Norma l(0 , l2ogodds) Where 0 is the mean of the distribution of hospital intercepts and lo2 go d d sis the hospital-to-hospital random effect in the log odds scale. 2 log odds is a quantity of fundamental interest in reliability calculations The hospital-to-hospital random effect is in the log odds scale. There is a choice to be made whether to calculate the reliability in the log odds or the probability scale. Both approaches have advantages. The log odds scale is the natural scale for logistic regression. The probability scale is the scale where the hospital profiles will most likely be reported. In the delta calculation reported below you can see that the reliability will be roughly the same if isn’t so large that it spans substantial non-linearity in the logistic transform. We pursue reliability in the probability scale here since it is a better fit to the hospital profiling policy problem. 2 The basic definition of reliability is: Reliability= 2 2 i2 i2 is the hospital specific sampling error variance for the infection rate. The binomial distribution ˆ i (1 pˆ i )ni where p̂i is used to represent the number of infections has a mean of p̂i ni and a variance of p Where the proportion of cases at hospital i that have an infection. The rate rather than the total number of infections is the quantity of interest here so we will use the variance of the rate estimate, the squared standard error of the rate estimate: ˆi2 pˆi (1 pˆi ) / ni s Since our estimate is in the log odds scale we need to apply a delta method calculation to transform 2 log odds to the probability scale. The expit function ( p ex ) transforms from the log odds scale to 1 ex the probability scale. We need the derivative of this function which is p*(1-p). Since this is the multiplier to transform log odds we must square it to apply to 2 2 log odds so our estimate of p * (1 p) 2 2 2 squared will be: 2 l ogodds Where p is the probability where the transformation occurs. For p we use the infection rate for the whole dataset. Note that the inverse of this transformation could be applied to the hospital specific sampling variances to develop a reliability estimate in the log odds scale. 3 Supplemental Digital Content 3: Table of fixed effect odds ratios and between-hospital variance for each model Deep/Organ-space SSI Superficial SSI Model “Any SSI” Model Model Odds Odds Ratio p-value p-value Odds Ratio p-value Ratio Intercept 0.041 <0.001 0.037 <0.001 0.083 <0.001 Procedure: (vs. Open colectomy) Ref Ref ref Laparoscopic colectomy 0.582 <0.001 0.613 <0.001 0.589 <0.001 Open proctectomy 1.207 0.059 1.290 0.014 1.265 0.002 Laparoscopic proctectomy 0.639 0.096 0.962 0.868 0.766 0.153 Diagnosis: (vs. Benign Neoplasm) Ref Ref ref Malignant neoplasm 1.295 0.007 1.321 0.022 1.321 <0.001 Diverticulitis 1.686 <0.001 1.137 0.344 1.467 <0.001 Diverticulosis 1.634 0.003 1.153 0.518 1.462 0.007 Ulcerative colitis/Crohns 1.323 0.042 1.986 <0.001 1.631 <0.001 Obstruction/perforation 1.649 <0.001 1.549 0.003 1.654 <0.001 Vascular insufficiency 0.968 0.887 1.101 0.672 1.037 0.827 Fistula 1.518 0.016 2.018 <0.001 1.756 <0.001 Rectal prolapse 0.157 <0.001 0.599 0.081 0.320 <0.001 Infectious colitis/peritonitis 1.184 0.418 1.338 0.163 1.254 0.141 Hemorrhage 3.000 <0.001 2.059 0.027 2.875 <0.001 Other 1.125 0.380 1.751 <0.001 1.413 0.001 Age: (vs. <55 years) Ref Ref Ref 1.087 0.224 0.759 <0.001 0.933 0.196 55-64 65-74 1.052 0.495 0.639 <0.001 0.834 0.002 75-84 0.916 0.318 0.582 <0.001 0.736 <0.001 0.795 0.075 0.480 <0.001 0.622 <0.001 >84 Male 0.982 0.715 1.201 0.001 1.079 0.051 Race: (vs. White) Ref Ref Ref Black 0.933 0.439 0.921 0.399 0.924 0.256 Other 1.052 0.570 1.375 <0.001 1.213 0.004 Hispanic (vs. Non-Hispanic) 1.134 0.285 0.928 0.583 1.055 0.568 Admission source (vs. Home) Ref Ref Ref Acute care hospital 0.783 0.124 0.969 0.829 0.858 0.179 Chronic care facility 1.062 0.751 0.800 0.288 0.942 0.682 Other 1.417 0.245 0.944 0.878 1.286 0.304 BMI (vs. Normal 18.5-24.9) Ref Ref Ref Underweight (<18.5) 0.883 0.452 1.057 0.699 0.975 0.823 Overweight (25-29.9) 1.429 <0.001 1.017 0.807 1.234 <0.001 Class I obesity (30-34.9) 1.741 <0.001 1.197 0.026 1.509 <0.001 Class II obesity (35-39.9) 2.205 <0.001 1.307 0.013 1.851 <0.001 2.484 <0.001 1.527 <0.001 2.114 <0.001 Class III obesity (40) Functional status (vs. Independent) Ref Ref Ref Partially dependent 1.088 0.402 1.370 0.002 1.253 0.003 Totally dependent 0.898 0.555 0.959 0.812 0.947 0.679 Smoker 1.069 0.292 1.143 0.047 1.109 0.035 Alcohol use 1.253 0.061 1.338 0.021 1.313 0.004 Renal Failure 0.687 0.067 1.200 0.278 0.951 0.711 Diabetes (vs. None) Ref Ref Ref Oral medication 1.081 0.314 0.865 0.134 0.987 0.832 Insulin 1.061 0.581 0.846 0.186 0.945 0.514 Dyspnea (vs. None) Ref Ref Ref 4 Moderate exertion At rest COPD Pneumonia Steroid Use Bleeding disorder Congestive heart failure Hypertension Myocardial infarction Disseminated cancer Weight loss Chemotherapy Radiotherapy Preop blood transfusion Preop Sepsis (vs. None/SIRS) Sepsis Septic shock ASA class (vs. I and II) Class III Class IV and V Wound class (vs. II) Class III Class IV Emergency procedure Between-hospital variance (probability scale) Between-hospital variance (log odds scale) 1.165 1.142 1.163 0.707 0.926 1.008 0.954 1.003 0.791 0.953 0.850 0.733 0.898 0.877 Ref 0.687 0.546 Ref 1.254 1.080 Ref 1.204 1.060 0.818 0.061 0.466 0.129 0.287 0.459 0.939 0.834 0.957 0.403 0.694 0.161 0.140 0.425 0.637 0.003 0.008 <0.001 0.502 0.015 0.521 0.024 1.598 x 10- 1.032 0.974 1.102 0.747 1.198 0.998 0.586 1.086 1.683 1.510 0.986 0.993 1.434 1.354 Ref 1.351 1.201 Ref 1.339 1.115 Ref 1.306 1.420 0.819 0.747 0.884 0.390 0.279 0.062 0.988 0.062 0.195 0.022 <0.001 0.901 0.969 0.005 0.252 0.008 0.336 <0.001 0.374 0.001 <0.001 0.032 1.132 1.024 1.146 0.742 1.075 0.993 0.771 1.033 1.158 1.219 0.914 0.884 1.101 1.097 Ref 1.000 0.852 Ref 1.311 1.084 Ref 1.268 1.221 0.793 3.997 x 10-4 1.943 x 10- 3 0.312 0.128 0.145 5 3 0.060 0.861 0.085 0.165 0.337 0.936 0.156 0.460 0.437 0.025 0.288 0.380 0.332 0.650 0.998 0.294 <0.001 0.364 <0.001 0.004 0.001