Prototype 1.0
advertisement

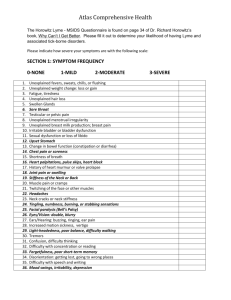
Prototype 1.0 Lyme disease: Inconsistencies with CDC Diagnosis & Treatment Protocols With What is Actually Occurring 1. Vision a. Collage b. I envision transparency and truth, where individuals move from protecting themselves and their careers at an ego level, to transcend the fear of consequences as they become eco-centric. I see funding for research; adequate testing methodologies (PCR, etc.); revised, individualized & affordable treatment plans. I see responsibility and action being a function of our collective and mutual consciousness. 2. Core Team a. Coaching Circle 113 b. Lyme Group c. Kimberly, Samantha, Lincoln Depelteau-Tracey d. Governor Maggie Hassan (friend) of New Hampshire, Al Gore, Hillary Clinton, George W. Bush, Dr. Richard Horowitz, dr. Paul Moran 3. 0.8 Iterate, iterate, iterate a. Prepare educational platform and ‘talking points’ to educate and enroll partnerships 4. Platforms and Space a. Coaching Circle 113 b. SubLyme Art 5. Listen to the Universe a. Daily Practices i. Course in Miracles ii. Journaling iii. Dialogue Walks 6. Integrating Head, Heart, and Hand a. Being an observer of self b. Presencing in the moment Prototype 1.0 Lyme disease: Inconsistencies with CDC Diagnosis & Treatment Protocols With What is Actually Occurring Lyme disease: Inconsistencies with CDC Diagnosis & Treatment Protocols With What is Actually Occurring Lyme disease is caused by the bacterium Borrelia burgdorferi and is transmitted to humans through the bite of infected blacklegged ticks. Typical symptoms include fever, headache, fatigue, and a characteristic skin rash called erythema migrans. If left untreated, infection can spread to joints, the heart, and the nervous system. Lyme disease is diagnosed based on symptoms, physical findings (e.g., rash), and the possibility of exposure to infected ticks; laboratory testing is helpful if used correctly and performed with validated methods. According to the CDC: most cases of Lyme disease can be treated successfully with a few weeks of antibiotics. The ticks that transmit Lyme disease can occasionally transmit other tick-borne diseases as well. Syphilis is a sexually transmitted, infectious disease caused by the spirochete Treponema pallidum. Length of treatment depends on how severe the syphilis is, and factors such as the patient's overall health. Follow-up blood tests must be done at 3, 6, 12, and 24 months to ensure that the infection is gone. Secondary syphilis can be cured if it is diagnosed early and treated effectively. Although it usually goes away within weeks, in some cases it may last for up to 1 year. Without treatment, up to one-third of patients will have late complications of syphilis. Late syphilis and late Lyme may be permanently disabling, and it may lead to death. In reading the CDC website about Lyme, a person, including MD’s can conclude that ‘this is it’ this is the word. However, there are other things to take into consideration. Basic Information about Lyme Disease By The International Lyme and Associated Diseases Society . 1 Lyme disease is transmitted by the bite of a tick, and the disease is prevalent across the United States and throughout the world. . 2 Lyme disease is a clinical diagnosis. 3 Fewer than 50% of patients with Lyme disease recall a tick bite. In some studies this number is as low as 15% in culture-proven infection with the Lyme spirochete. . 6 The Elisa screening test is unreliable. The test misses 35% of culture proven Lyme disease (only 65% sensitivity) and is unacceptable as the first step of a two-step screening protocol. By definition, a screening test should have at least 95% sensitivity. . 7 Of patients with acute culture-proven Lyme disease, 20–30% remain seronegative on serial western blot sampling. Antibody titers also appear to decline over Prototype 1.0 Lyme disease: Inconsistencies with CDC Diagnosis & Treatment Protocols With What is Actually Occurring . . . . . . . . time; thus while the western blot may remain positive for months, it may not always be sensitive enough to detect chronic infection with the Lyme spirochete. For “epidemiological purposes” the CDC eliminated from the western blot analysis the reading of bands 31 and 34. These bands are so specific to Borrelia Burgdorferi that they were chosen for vaccine development. Since a vaccine for Lyme disease is currently unavailable, however, a positive 31 or 34 band is highly indicative of Borrelia Burgdorferi exposure. Yet these bands are not reported in commercial Lyme tests. 8 When used as part of a diagnostic evaluation for Lyme disease, the western blot should be performed by a laboratory that reads and reports all of the bands related to Borrelia Burgdorferi. Laboratories that use FDA approved kits (for instance, the mardx marblot®) are restricted from reporting all of the bands, as they must abide by the rules of the manufacturer. These rules are set up in accordance with the CDC's surveillance criteria and increase the risk of falsenegative results. The commercial kits may be useful for surveillance purposes, but they offer too little information to be useful in patient management. 9 There are 5 subspecies of Borrelia Burgdorferi, over 100 strains in the US, and 300 strains worldwide. 10 Testing for Babesia, Anaplasma, Ehrlichia and Bartonella (other tick-transmitted organisms) should be performed. 1 A preponderance of evidence indicates that active ongoing spirochetal infection with or without other tick-borne coinfections is the cause of the persistent symptoms in chronic Lyme disease. 12 There has never been a study demonstrating that 30 days of antibiotic treatment cures chronic Lyme disease. However there is a plethora of documentation in the us and European medical literature demonstrating by histology and culture techniques that short courses of antibiotic treatment fail to eradicate the Lyme spirochete. Short treatment courses have resulted in upwards of a 40% relapse rate, especially if treatment is delayed. 13 Most cases of chronic Lyme disease require an extended course of antibiotic therapy to achieve symptomatic relief. 14 Many patients with chronic Lyme disease require prolonged treatment until the patient is symptom-free. 15 Like Syphilis in the 19th century, Lyme disease has been called the great imitator and should be considered in the differential diagnosis of rheumatologic and neurologic conditions, as well as Chronic Fatigue Syndrome, Fibromyalgia, Somatization Disorder and any difficult-to-diagnose multi-system illness. After many years of patients not getting well, fresh research shows that biofilm communities may be protecting Lyme disease and other co-infections from full spectrum antibiotic therapy effectiveness. University of New Haven suggests that Biofilm is protecting the Lyme disease spirochete from antibiotics and any therapy not containing a method to address biofilm may prove to be inferior. Lyme disease in its chronic form loves to hide and live within red blood cells and nervous tissue, including the brain. Prototype 1.0 Lyme disease: Inconsistencies with CDC Diagnosis & Treatment Protocols With What is Actually Occurring Antibiotics and other medications are not commonly designed to penetrate within the red blood cells or capable of breaking the blood brain barrier, and leave these organisms untouched to grow and spread. In the aftermath of WWII, over 1500 scientists, engineers, technicians from Nazi Germany and other countries were brought to the U.S. for employment. This project was known as Operation Paperclip; this project was to exploit German scientific knowledge and deny it to the Soviet Union. Erich Traubel was a German veterinarian and virologist who specialized in foot & mouth disease, Rinderpest (cattle plague) and Newcastle disease (bird disease that is transmissible to humans). He was a researcher in the Third Reich’s biological warfare program (cover name: Cancer Research Program) and did similar work in the U.S. One of the places he frequented was the Plum Island Bioweapon research facility off the coast of Long Island. In The Belarus Secret Loftus exposed records of the Nazi germ warfare scientists who experimented with poison ticks dropped from planes to spread rare diseases. In 1952, the Joint Chiefs of Staff called for a 'vigorous, well-planned, largescale [biological warfare] test to the secretary of defense later that year stated, 'Steps should be take to make certain of adequate facilities are available, including those at Fort Detrick, Dugway Proving Ground, Fort Terry (Plum Island) and an island field testing area.' "Traub might have monitored the tests. A source that worked on Plum Island in the 1950's recalls that animal handlers and a scientist released ticks outdoors on the island. 'They called him the Nazi scientist, when they came in, in 1951-they were inoculating these ticks,' and a picture he once saw 'shows the animal handler pointing to the area on Plum where they released the ticks.' It was suspected that Plum Island played a role in the evolution of Lyme disease, given the nature of its business and its proximity to Old Lyme, Connecticut. "Researchers trying to prove that Lyme disease existed before 1975 claim to have isolated Bb [the bacterium that causes the infection] in ticks collected on nearby Shelter Island and Long Island in the late 1940's. That timing coincides with both Erich Traub's arrival in the United States on Project PAPERCLIP and the Army's selection of Plum Island as its offshore biological warfare laboratory. There is a lot of denial, and some of these allegations are deemed a ‘conspiracy theory’. What I am up against is the denial, similar to CC denial. Stakeholders: CDC, USDA, Scientific American dismissed the possibility of a "Nazi scientist" link to Plum Island. In FTR#240-part of the long FTR series about "German Corporate Control over American Media"--it was noted that the Von Holtzbrinck firm controls that magazine. Like its larger competitor Bertelsmann, the Von Holtzbrinck firm is rooted firmly in the Third Reich. My understanding is that some CDC board members Prototype 1.0 Lyme disease: Inconsistencies with CDC Diagnosis & Treatment Protocols With What is Actually Occurring own a patent of the Borrelia burgdorferi. Thousands upon thousands of people suffering and dying; LLMDs Vision for future: I envision transparency and truth, where individuals move from protecting themselves and their careers at an ego level, to transcend the fear of consequences as they become eco-centric. I see adequate testing methodologies (PCR) and optimal treatment plans. Financial assistance is available to the infected. I see a place where there are no sides, no opposing thoughts, there is only oneness. All our hearts are beating in unison, everything is connected, all people, animal, vegetation, elements. What do I need to let go of: I notice that I am oftentimes on the under dog’s side of a controversy. Environmental, Chiropractic, Climate Change, now Lyme. I need to let go that I am always an under-dog. I need to let go of fear (criticism, death threats, loss of credibility). I need to let go of my inner dialogue: I don’t know where to start, I don’t know who to ask for help, how am I going to find the time, etc. I need to let go of my own fear of my body betraying me because of this disease. I need to learn: I still need to research the evidence on both sides. I need to learn that I cannot do this by myself and I need to learn to build team around this. Help: hold the vision with me. Lyme disease, transmitted by a bite from a tick infected by the Borrelia burgdorferi bacteria, had long been considered easy to treat, usually requiring a single doctor’s visit and a few weeks of antibiotics for most people. But new research from the Johns Hopkins Bloomberg School of Public Health suggests that a prolonged illness associated with the disease is more widespread and serious in some patients than previously understood. With an estimated 240,000 to 440,000 new cases of the tick-borne illness diagnosed every year, the researchers found that Lyme disease costs the U.S. healthcare system between $712 million and $1.3 billion a year — or nearly $3,000 per patient on average — in return doctor visits and testing, likely to investigate the cause of some patients’ lingering symptoms of fatigue, musculoskeletal pain and memory problems. These visits come after patients have finished their original course of antibiotics. Some doctors call those persistent symptoms post-treatment Lyme disease syndrome (PTLDS); others call it chronic Lyme disease. Still others attribute the complaints of fatigue, headaches and memory problems to the hum of daily life, the aches and pains that come with aging. At the core of the controversy is whether PTLDS can be a severe Prototype 1.0 Lyme disease: Inconsistencies with CDC Diagnosis & Treatment Protocols With What is Actually Occurring and chronic condition that requires more than reassurance and symptomatic therapy. While a blood test can confirm Lyme disease, there is no definitive test for PTLDS and there are no approved or proven treatments. It’s a controversial topic in medicine, the Hopkins researchers say. A report on the findings was published online Feb. 4 in the journal PLOS ONE. “Our study looks at the actual costs of treating patients in the year following their Lyme diagnosis,” says study author Emily Adrion, MSc, a PhD candidate in the Department of Health Policy and Management at the Johns Hopkins Bloomberg School of Public Health. “Regardless of what you call it, our data show that many people who have been diagnosed with Lyme disease are in fact going back to the doctor complaining of persistent symptoms, getting multiple tests and being retreated. They cost the healthcare system about $1 billion a year and it is clear that we need effective, cost-effective and compassionate management of these patients to improve their outcomes even if we don’t know what to call the disease.” Adrion and her colleagues looked at medical claims data from approximately 47 million people enrolled in a wide range of commercial health insurance plans in the United States between 2006 and 2010. The researchers ended up analyzing 52,795 cases of Lyme disease patients under the age of 65 who had been treated with antibiotics within 30 days of a Lyme disease test order and/or Lyme disease diagnosis. The data were compared to nearly 264,000 other similar people with no evidence of Lyme disease exposure. The researchers found that, on average, people with Lyme disease cost the system $2,968 more than matched controls. They had 87 percent more visits to the doctor and 71 percent more visits to the emergency room within the year following diagnosis. Those with Lyme disease were nearly five times more likely to have any PTLDS-related diagnosis — fatigue, nerve pain, joint pain, cognitive troubles — within that year and were 5.5 times more likely to have a diagnosis of debility and excessive fatigue. Among those with Lyme disease, having one or more PTLDS-related diagnosis was associated with $3,798 more in healthcare costs as compared to those with no posttreatment symptoms. Lyme disease is named after the town in Connecticut where it was first recognized in 1975. It now hits its peak in June and July and is found from Maine to Virginia along the East Coast of the United States. The tick causes a skin reaction that resembles a bulls-eye or spider bite. If left untreated, Lyme disease may lead to neurologic and rheumatic symptoms weeks or months later. Treatment with the antibiotic doxycycline is associated with a more rapid resolution of early signs of infection and prevention of the majority of later symptoms, the researchers say. Still, some patients report symptoms lasting for weeks, months or years beyond completion of the original antibiotic regimen. There is no approved therapy for these Prototype 1.0 Lyme disease: Inconsistencies with CDC Diagnosis & Treatment Protocols With What is Actually Occurring patients and the magnitude of the problem in the U.S. population has never been systematically studied. The Centers for Disease Control and Prevention (CDC) estimates 10 percent to 20 percent of those treated for Lyme disease with the recommended two-tofour week course of antibiotics continue to have symptoms. But, in the new study, the researchers found that more than 63 percent of those treated for Lyme disease had at least one PTLDS-related diagnosis — a rate 36-percentage points higher than those who did not have Lyme disease. The study’s lead author John Aucott, MD, an assistant professor of rheumatology at the Johns Hopkins University School of Medicine, says it does no good to keep debating the existence of long-term problems related to Lyme disease while people are suffering a debilitating illness. And he says that increasing awareness of potential complications is crucial to avoid misdiagnosis and unnecessary medical testing. “These patients are lost,” he says. “No one really knows what to do with them. It’s a challenge, but the first thing we need to do is recognize this is a problem. There’s not a magic pill. These patients already got the magic pill and it didn’t work.” “Healthcare costs, utilization and patterns of care following Lyme disease” was written by Emily Adrion, MSc; John Aucott, MD; Klaus Lemke, PhD; and Jonathan P. Weiner, DrPH. This research was funded by a grant from the Lyme Disease Research Foundation. Source: Johns Hopkins Bloomberg School of Public Health http://www.infectioncontroltoday.com/news/2015/02/lyme-disease-costs-up-to13%20billion-annually-to-treat-study-finds.aspx