Joe`s HIV Outline
advertisement

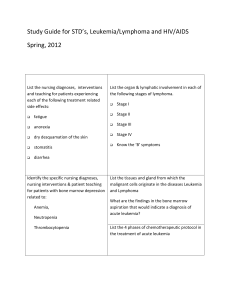
The information below is the text that was under the graphs on the PP> For adults and adolescents living with HIV/AIDS, prevalence rates per 100,000 population are shown for 34 states and 5 U.S. dependent areas with confidential name-based HIV infection surveillance. Areas with the highest prevalence rates in 2007 were New York, the U.S. Virgin Islands, Florida, New Jersey, and Louisiana. The following 34 states and 5 U.S. dependent areas have had laws or regulations requiring confidential namebased HIV infection surveillance since at least 2003: Alabama, Alaska, Arizona, Arkansas, Colorado, Florida, Georgia, Idaho, Indiana, Iowa, Kansas, Louisiana, Michigan, Minnesota, Mississippi, Missouri, Nebraska, Nevada, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, West Virginia, Wisconsin, Wyoming, American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, and the U.S. Virgin Islands. The data have been adjusted for reporting delays From 2004 through 2007 there were increases in the number of adults and adolescents living with HIV/AIDS in the 34 states with confidential name-based HIV infection surveillance. The increase is due primarily to the widespread use of highly active antiretroviral therapy, introduced in 1996, which has delayed the progression of AIDS to death. At the end of 2007, an estimated 549,195 adults and adolescents were living with HIV/AIDS; of these, 73% were males and 27% were females. The following 34 states have had laws or regulations requiring confidential name-based HIV infection surveillance since at least 2003: Alabama, Alaska, Arizona, Arkansas, Colorado, Florida, Georgia, Idaho, Indiana, Iowa, Kansas, Louisiana, Michigan, Minnesota, Mississippi, Missouri, Nebraska, Nevada, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, West Virginia, Wisconsin, and Wyoming. Data exclude persons who have died and were reported to the HIV/AIDS Reporting System as of December 2007. The data have been adjusted for reporting delays. In 2007, of HIV/AIDS cases diagnosed among male adults and adolescents in 34 states with confidential namebased HIV infection surveillance, 71% were attributed to male-to-male sexual contact and 10% were attributed to injection drug use. Approximately 14% of cases were attributed to high-risk heterosexual contact and 4% attributed to male-to-male sexual contact and injection drug use. Most (83%) of the HIV/AIDS cases diagnosed among female adults and adolescents were attributed to high-risk heterosexual contact, and 16% were attributed to injection drug use. The following 34 states have had laws or regulations requiring confidential name-based HIV infection surveillance since at least 2003: Alabama, Alaska, Arizona, Arkansas, Colorado, Florida, Georgia, Idaho, Indiana, Iowa, Kansas, Louisiana, Michigan, Minnesota, Mississippi, Missouri, Nebraska, Nevada, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, West Virginia, Wisconsin, and Wyoming. The data Blacks/African Americans accounted for over half (51%) of the estimated number of HIV/AIDS diagnoses made during 2007, followed by whites (29%) and Hispanic/Latinos (18%). These numbers do not account for individuals of unknown race/ethnicity or those who choose not to identify with any particular race/ethnicity [have been adjusted for reporting delays and missing risk-factor information. Life Expectancy • 1990s = 10 years • Present = 35 years • As of 2009 from BJM the Lancet Patho of HIV Virus • Infection with retrovirus (HIV) • Retrovirus binds to a CD4+ cell • CD4 make up 2/3 of WBC found all throughout the body and tissues • DNA of CD4 T Helper cell which is essential to the immune system • RNA is inserted into the CD4+ cell • RNA is converted to DNA and becomes part of the infected cell’s genetic material! Latency vs. Proliferation • Cells may remain relatively inactive and latent for years. (Provirus) • Activated cells proliferate and produce large amounts of viral particles. How HIV is NOT Transmitted • Shaking hands • Hugging • Casual kissing • Toilet seats • Drinking fountains • Doorknobs • Food • Pets • Mosquitoes How HIV is Transmitted • HIV is very fragile • Having sex with infected partner • Anal, vaginal, oral • Sharing needles/syringes with HIV infected individual • Exposure during birth or through breast feeding • Less chance of exposure in C-Section birth Blood Transfusions • Since 1985 all donated blood in the United States has been tested for HIV. Risk Factors for HIV • IV Drug Use (Illicit drugs, Steroids) • Unprotected Sex • Diagnosis of hepatitis, tuberculosis, or STD • Received blood transfusion from 1978-1985 Prevention of Transmission (NO CURE) • Abstinence • Condoms • Testing for HIV • Monitor and treat other STDs • Don’t inject drugs ABCs of Protection (from CDC) • A = Abstinence • B = Be Faithful • C = Condoms HIV Screening EDUCATION!! • All clients must be educated on the screening process. CONFIDENTIALITY!! • Must sign a consent for testing SUPPORT!! • Will need ongoing counseling. HIV Antibody Tests – EIA (enzyme immunoassay) test- most common • Identifies antibodies against HIV (Antibodies that are trying to attack HIV) • 2-13wks after exp osure – Western Blot assay • Measures individual antibody classes. Confirms disease. • Viral Load tests- the amount of virus in the body – Monitor response to treatment – Good predictor of progression. Low the viral load = the longer it takes to get full blown AIDs. • CD4/CD8 ratio- overall indicator of immune function – The more present = the stronger the immune system is – HIV pt doing well will have a High vol load and a low CD4 Stages of HIV • Based on clinical condition – S/S- Candidiasis, Thrush, Fever, Neuropathies, Pneumonia • CD4+ T-Cell counts – 500-1500 cells per microliter • See table 52-1 pg 1823 A B C Asymptomatic or Acute HIV Symptomatic Not A or C AIDS – Indicator Conditions (1) > 500/µL AI BI CI (2) 200-499/µL A2 B2 C2 (3) < 200/µL A3 B3 C3 CD4+ T-cell Category Primary Infection (Acute HIV) • Period from infection to development of antibodies • Widespread dissemination of HIV • Window Period – 30 days to 3 months- where indiv will have HIV, but test negative • Viral Set Point- the balance between HIV levels and immune response – Higher the set point the worse the prognosis Clinical Manifestations: – None – Flu-like or Mono-like symptoms • Fever • Enlarged lymph nodes • Rash • Muscle aches • Headaches HIV Asymptomatic (Category A) – More than 500 CD4+ T-cells/µL – Enough cells to preserve immunity – Viral Set Point achieved – Few if any symptoms – Average time period = 8-10 years HIV Symptomatic (Category B) – 200-499 CD4+ T-cells/µL – Weakened enough that s/s start to show – Opportunistic conditions such as: – Thrush - Long term diarrhea – Leukoplakia - Shingles (Herpes zoster) – Pelvic Inflam. Disease - Cervical Carcinoma – Fever - Peripheral Neuropathy AIDS (Category C) – Fewer than 200 CD4+ T-cells/µL – You have Aids! Once reached “C”, there’s no going back. – Clinical Manifestations: – Anemia -Candidiasis of bronchi, trachea, esophagus – Cytomegalovirus -HIV encephalopathy – Kaposi’s Sarcoma -Chronic herpes ulcerations – Lymphomas -Mycobacterium tuberculosis – Recurrent Pneumonia -Pneumocystis pneumonia (PCP) – Toxoplasmosis of Brain -Wasting Syndrome Treatment of HIV Infection • The goal of HIV treatment is to slow progression and improve quality of life. • Treatment given to pts w/ < 350 cell count. • Treatment decisions will be based on CD4+ counts, viral load, symptoms of HIV/AIDS, and willingness of the patient to adhere to treatment. Highly Active Antiretroviral Therapy (HAART) • Will slow growth and reproduction of HIV • Often have multi-drug combinations • Monitor viral load o Want it to be low • Things to Consider… o Major side effects o Potential viral resistance o Concerns about adherence to regimen • Side effects: o Lipodystrophy syndrome/ hypercholesterolemia The meds will cause fat collections, fat distribution, and growths o Fat redistribution syndrome/pseudo-Cushing’s o Facial wasting o Hepatotoxicity Clinical Manifestations of HIV/AIDS • Fatigue • Opportunistic Infections Clinical Manifestations of HIV/AIDS: Respiratory • Pneumocystis Pneumonia (PCP)- ***Most common infection in pts w/ Aids o Early onset: Cough, fever chills, SOB, dyspnea o Left untreated: Significant impairment & respiratory failure Cyanosis and altered mental status • Diagnosis = cultures of secretions and tissue biopsy • Treatment = Bactrim or Septra (TMP-SMZ) o Given prophylactically, when CD count drops below 200. Clinical Manifestations of HIV/AIDS: Respiratory These diseases will manifest more clearly in pts w/ HIV • Mycobacterium Avium Complex (MAC) • Tuberculosis Clinical Manifestations of HIV/AIDS: Gastrointestinal • Loss of appetite • Nausea/vomiting • Oral and esophageal candidiasis • Chronic diarrhea • ***Wasting syndrome- involuntary wt loss exceeding 10% in body weight. Loss of lean muscle mass. Clinical Manifestations of HIV/AIDS: Oncologic • ***Kaposi’s Sarcoma o Most common CA in a pt w/ Aids o Cutaneous lesions o Multiple organ involvement o Disfigurement o Pain o Impaired skin integrity Clinical Manifestations of HIV/AIDS: Oncologic Kaposi’s Sarcoma • Treatment – reduce discomfort – Decrease size of lesions • Surgical excision • Radiation • Injection of liquid nitrogen Clinical Manifestations of HIV/AIDS: Oncologic • B-Cell Lymphomas – Usually arise in a younger population than others with lymphoma – Brain, bone marrow, GI tract most common sites – Aggressive growth – Most treatment ineffective, cause pt is so immunocompromised. • Try chemo and radiation Clinical Manifestations of HIV/AIDS: Neurologic • HIV Encephalopathy – aka Aids Dementia Complex • Early stages: – Memory deficits, headache, confusion, ataxia • Late stages: – Delayed verbal responses, vacant stare, spastic Para-paresis, psychosis, hallucinations, seizures, death Clinical Manifestations of HIV/AIDS: Neurologic • Prone to… – Cryptococcus Meningitis – Peripheral Neuropathy Clinical Manifestations of HIV/AIDS: Depressive • Pain • Isolation • Guilt and shame • Loss of self-esteem • Helplessness, worthlessness Treatment: Antidepressants, counseling, psychostimulants, electroconvulsive therapy Clinical Manifestations of HIV/AIDS: Gynecologic • Recurrent yeast infections • HPV • Cervical cancer – Pts w/ HIV are x10 more likely to develop Clinical Manifestations of HIV/AIDS: Retinitis • Retinitis – Caused by Cytomegalovirus – Leading cause of blindness with HIV Use prophylactic antibiotics (ganciclovir) Nutrition Therapy • Calorie Counts • Appetite stimulants – Megace – Marinol- marijuana • ***Diet – High calorie -Easily digestible proteins – Inexpensive -Tolerated w/o diarrhea Nursing Diagnoses??? • Diarrhea • ***Risk for Infection- most likely to kill pt • Ineffective airway clearance • Imbalanced nutrition • Deficient knowledge • Social Isolation • Impaired skin integrity Emotional and Ethical Issues • Gerontologic Considerations – Due to sexual activity w/o protection. Don’t think about HIV. New relationships. Veterans & Drugs. Blood transfusions prior to 1985. • Needle exchange programs Emotional and Ethical Issues • Transmission to Health Care Providers – More hepatitis than HIV • Follow standard precautions • Standard Precautions – blood and semen are more common vectors • Post-exposure prophylaxis – Wash w/ soap and water immediately. Milk cuts. Alert Supvr. Identify pt, if known positive then no testing. But unknown than test HIV and Hepatitis. Consent not needed for Hepatitis test, but is req’d for HIV. • Meds are and option for those poss. Exposed, but meds are highly renal/hepato toxic. – Chart 52-5 pg 1821 Emotional and Ethical Concerns • How do you feel about caring for HIV/AIDS patient? – Option is available to deny assignment of HIV pt. HIV/AIDS Basics • Don’t have unprotected sex • Don’t share needles/syringes • Monitor and treat STDs • Standard Precautions


![Africa on the rise - Health[e]Foundation](http://s2.studylib.net/store/data/005761249_1-4e2609b64b2c374f99ff6e9dbe45edb8-300x300.png)