67-Serotonergic_Neurotoxicity_and_Depression
advertisement
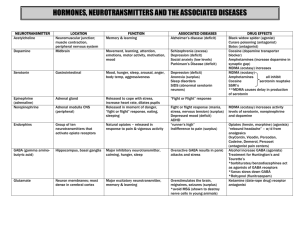
1 Serotonergic Neurotoxicity and Depression Following MDMA Administration Ann Frisse Barnard College 2 The toxicology of 3,4-methylenedioxymethamphetamine (MDMA), often referred to as ecstasy, was first evaluated by the U.S. military in the 1950s. In the late 1970s into the early 1980s, this drug was used in psychotherapy sessions to increase self-esteem and facilitate conversation. In 1985, the DEA classified MDMA as a Schedule 1 drug due to potential neurotoxic effects and addictive properties. MDMA use continued, albeit illegally, and became strongly associated with the rave scene of the 1990s. This drug is now used by a wider demographic and is rising in popularity among young adults (Green, Mechan, Elliott, O’Shea, & Colado, 2003). The appeal of this drug stems from the rapid release of serotonin (5-HT) and resulting euphoria experienced after administration. More specifically, MDMA binds to the 5HT transporter (SERT) with high affinity and blocks reuptake of 5-HT. It also enters neurons via this transporter. Once inside the neuron the drug stimulates 5-HT release from the synaptic vesicles into the cytoplasm. The SERTs then reverse direction, releasing 5-HT from the cytoplasm into the extracellular fluid. The acute and long-term deleterious effects of this process on serotonergic neurons are not well understood. The extensive history of the drug, its rising popularity, and inconsistent research findings on MDMA mediated neurotoxicity suggest a need to review the current literature pertaining to potential neurotoxic effects of MDMA. Deleterious Effects of MDMA on Serotonergic Neurons and Serotonin Levels Rats MDMA has acute toxic effects on serotonergic neurons in rats. Commins et al., found a dose-dependent reduction in 5-HT in the brain following MDMA delivery (1987). Male rats were administered doses of 10, 20, or 40 mg/kg MDMA or saline twice a day for four consecutive days. These rats were decapitated 2 weeks after the last injection. A separate group of rats was given a single injection of either saline or MDMA (20 or 40 mg/kg) and decapitated 3 at two or eight weeks after injection. Brain tissue samples were assayed for 5-HT by highperformance liquid chromatography with electrochemical detection. Results from the repeated injections found that all three doses resulted in significant depletions of 5-HT in the hippocampus, somatosensory cortex, and the rest of the cortex. Doses of 20, or 40 mg/kg caused depletions in the striatum whereas depletion in the hypothalamus was only seen at 40 mg/kg. There was a negative correlation between MDMA dose and 5-HT content. The single injection of 40mg/kg, but not 20 mg/kg, significantly depleted 5-HT levels at both two and eight weeks after MDMA administration in all brain regions examined excluding the hypothalamus suggesting that a single, large dose is sufficient to cause persistent neurotoxicity. This study also contained a neurohistological component in order to evaluate neuronal damage. Rats were administered 80 mg/kg of MDMA or saline twice a day for two days and were perfused 13 to 16 hours after the last injection. Sections of the striatum and the somatosensory cortex were silverstained and examined for the presence or absence of terminal degradation by an observer unaware of the rat’s treatment condition. Nerve terminal degradation was found in both brain regions. Dose dependent reductions in 5-HT following MDMA administration has been further supported by the work of Battaglia, Yeh, & De Souza (1988). Rats were subcutaneously injected with saline or 5, 10, or 20 mg/kg MDMA twice a day for four consecutive days, similar to the previous experiment. Animals were sacrificed 18 hours after the last injection. Portions of the frontal cerebral cortices were homogenized, centrifuged, and measured by electrochemical detection following reverse phase HPLC separation. Concentrations of 5-HT were then calculated. SERTs were labeled with 3H-paroxetine, a radioligand. Radioactivity was detected to observe changes in SERT density. Since the SERTs are located on axons terminals of 4 serotonergic neurons, it is considered to be a reliable marker of 5-HT neuronal damage. All doses showed significant decreases in the content of 5-HT as well as the density of SERTs in rat prefrontal cortex with higher doses producing greater reductions. Reductions in 5-HT concentration and uptake sites reached a maximum of 90% of control values after administration of 20 mg/kg MDMA. A separate subset of rats was administered injections of saline or 10 mg/kg MDMA every 12 hours one, two, four, or eight times to evaluate the effects of dose regimen on neurodegeration. One injection did not produce any significant reductions in 5-HT content or SERT density compared to controls. This agrees with the findings of Commins et al. who found that a single dose of 40-mg/ kg was necessary to produce neurotoxicity (1987). The 10-mg/kg dose was not large enough to produce visible damage. Increasing the number of injections beyond 1 dose resulted in progressively lower concentrations of 5-HT. Significant reduction in SERT density was only seen in rats receiving 8 injections. Results suggest that the reductions in 5-HT and SERTs are reversible. A third subset of rats was administered saline or 20 mg/kg MDMA twice a day for four consecutive days. Rats were sacrificed at 18 hours, 1, 2, 4, 8, 26, or 52 weeks following treatment. At all time points up to 6 months, the density of 5-HT uptake sites was significantly below those of controls. However, by 12 months, the density of 5-HT uptake sites in MDMA treated rats returned to control levels indicating that more than 6 months are required for complete recovery of 5-HT uptake sites. According to these results, the length of MDMA abstinence following repeated MDMA administration in the Commins et al. experiment, 14 days, was not sufficient to show significant recovery (1987). Primates 5 Several studies have been conducted to evaluate whether the MDMA mediated acute serotonergic neurotoxicity seen in rats is mirrored in nonhuman primates. The literature suggests that similar deleterious effects are seen in both categories of animal models. Results of nonhuman primate study done by Wilson, Ricaurte, and Molliver support results from rat studies as well as provide specificity to the damage of serotonergic neurons following MDMA administration (1989). In this study, adult macaque monkeys received 5 mg/kg MDMA twice a day for four days. Drug treated monkeys were sacrificed two weeks after drug administration. Untreated control macaque monkeys were also sacrificed to serve as controls. Immunohistochemical methods were used to evaluate the distribution and morphology of serotonergic axons. Results showed significant reductions in the density of 5-HT immunoreactive axons in the cerebral cortexes of MDMA treated monkeys. Although a quantitative comparison was not done, it was estimated that 60-90% of the 5-HT axons were lost due to MDMA exposure. Some axons were spared from MDMA damage. These were identified as beaded axons, one of two morphologic classes of serotonergic axon terminals. In contrast, fine axons were significantly reduced in density in the MDMA treated monkeys suggesting that MDMA selectively damages fine serotonergic axons and spares beaded axons. These findings support similar findings of fine axon degeneration in rats (O’Hearn, Battaglia, De Souza, Kuhar, & Molliver, 1988). In contrast to the long-term recovery of serotonergic axon terminals seen in rats, damage to serotonergic neurons appears to be more permanent in primates. Ricaurte, Martello, Katz, and Martello evaluated the long-term effects of MDMA on serotonergic neurons in squirrel monkeys (1992). Monkeys were administered 5 mg/kg MDMA twice daily for four consecutive days similar to the previous primate study. Concentration of 5-HT was measured by reverse phase 6 HPLC coupled to an electrochemical detector. Similar to the methods used by Battaglia et al., 3 H-paroxetine was used to label SERTs and radioactivity was used to measure the density of sites (1988). At two weeks post administration, a significant reduction in 5-HT was found in MDMA treated monkeys as well as a reduction in the number of 3H-paroxetine-labeled SERTs. At 10 weeks post administration, there appeared to be recovery of 5-HT and SERTs. However, by 18 months 5-HT deficits returned to low level observed 2 weeks after MDMA treatment in all regions except thalamus and hypothalamus. The thalamus saw partial recovery of 5-HT. Almost total recovery of 5-HT was seen in the hypothalamus by 8 months. By 18 months, 5-HT concentration was 140% of control concentrations. Despite the partial restoration of 5-HT seen in selected brain regions, the trend of recovery did not continue in all other brain regions examined, leading the authors to conclude that the neurotoxic effects of MDMA are more permanent in primates. Humans Findings from these animal studies should not be generalized to humans because there are many differences between typical human MDMA use and administration in animal models. These differences include dose, frequency of use, and route of administration. There may also be differences in drug metabolism between species. Despite the limitations of animal models, experiments involving humans have methodological issues. For example, cross sectional studies are frequently used which, although informative, does not assess the causality of neuronal damage. There are also many confounding variables when evaluating neurotoxic effects of drug use such as polydrug use, lifestyle, and education. Despite these limitations, there are similarities between findings of neurotoxicity in humans and those in animal models. 7 The effect of MDMA on SERTs in humans was evaluated by Buchert et al. (2004). Positron emission tomography (PET) was performed using [11C](+)McN5652, a highly specific ligand for serotonin transporters. From these results, distribution volume ratios were calculated. PET results were obtained from current MDMA users, former MDMA users, drug-naïve controls, and users of drugs other than MDMA. Drug history was verified using hair samples. Former MDMA users were required to have abstained from MDMA use for at least 20 weeks. Participants abstained from use of all psychoactive drugs three days before PET scans to avoid acute drug effects. Results show lower distribution volume ratios in current MDMA users. This decrease in SERTs seen in recent MDMA users supports similar findings in studies involving rats and nonhuman primates (Battaglia et al., 1988; Ricaurte, 1992; Wilson et al., 1989; Commins et al., 1987). Reductions in transporters were more pronounced and widespread in female subjects compared to those in the males. A significant negative correlation between SERT availability and mean MDMA dose was found in current MDMA users. This suggests that neurotoxicity is dose dependent in humans as it is in rats (Commins et al., 1987; Battaglia et al., 1988). No significant difference was found between SERT availability in former MDMA users and those in drug-naïve and polydrug controls. This as well as results showing a positive correlation between SERT availability and length of MDMA abstention suggests that damage to SERTs is reversible in humans. These results agree with findings of reversible serotonergic neurotoxicity in rats (Battaglia et al., 1988). Surprisingly, results pertaining to long-term reversibility of neurotoxicity do not agree with findings from primate studies, which show neurotoxic damage to be more permanent (Ricaurte et al., 1992). Research by Reneman et al. also supports the reversibility of MDMA mediated neurotoxicity in humans (2001b). Iodine 123-labeled 2-carbomethoxy-3-(4-iodophenyl) 8 tropane ([123I]-CIT) was used to label SERT densities. These were detected using singlephoton emission computed tomography (SPECT). Transporter densities were evaluated for groups of recent MDMA users, ex-MDMA users, and control subjects who had not previously used MDMA. The recent MDMA user group contained participants who were current users ranging to participants who had abstained from use for 4.8 months. Participants in the exMDMA user group were required to have stopped using MDMA at least one year before the study. All users were required to abstain from psychoactive drug use for three weeks preceding the study. Results showed significantly lower mean cortical [123I]-CIT-labeled 5-HT transporter density in recent MDMA users compared to controls but not in ex-MDMA users. No significant difference was seen between cortical binding ratios of ex-MDMA users and control subjects. These findings suggest that neurodegenerative effects of MDMA on 5-HT axon terminals in human cortex may be reversible. Further study by Reneman et al. elucidates these findings (2001a). SPECT was used in conjunction with the same radioligand used in the earlier study. Participants consisted of moderate MDMA users, heavy MDMA users, ex-users of MDMA, and MDMA-naïve controls. Moderate users were required to have ingested a maximum of 50 tablets whereas heavy users were required to have ingested more than 50 tablets in their lifetime. The ex-MDMA users were required to have taken a minimum of 50 tablets in their lifetime but have abstained from MDMA use for at least one year prior to commencing the study. Participants abstained from psychoactive drug use for 3 weeks before the study. Results show a significantly lower [123I]CIT binding ratio in female, but not male, heavy MDMA users compared to those in controls. This agrees with Buchert et al.’s findings that females have higher susceptibility to MDMA mediated serotonergic neuronal damage (2004). In ex-users, [123I]-CIT binding ratios were 9 significantly higher in females compared to current, female MDMA users but were not higher than those in controls. This suggests that although females are more susceptible to the neurotoxic effects of MDMA, this damage is reversible. In moderate users, [123I]-CIT binding ratios were not significantly different from those of controls in males and females. This suggests that moderate MDMA exposure has no significant effect on 5-HT transporters. The minimal level of exposure to MDMA and dose of the drug that results in neurotoxic damage in humans is still being debated. The studies by Reneman et al. should be interpreted with caution because causality cannot be established in retrospective studies such as these. Caution should also be taken when interpreting these findings because the MDMA users consumed significantly more amphetamine and cocaine in the past year than control and ex-MDMA groups. Therefore, the lower mean cortical [123I]-CIT binding ratio seen in current MDMA users compared to controls may have been due to higher rates of cocaine and amphetamine use by members of this group. Despite the limitations of conducting human research studies, results of these studies have similar conclusions: MDMA is neurotoxic to serotonergic axons, but this damage may not be permanent in humans. Damage to serotonergic neurons and depletion of 5-HT may have behavioral consequences. Serotonin is known to play a central role in regulating mood. Decreases in this neurotransmitter have been linked to depression. Low SERT density has also been associated with depression in humans (Malison et al., 1998). This evidence has lead researchers to hypothesize that the MDMA mediated decrease in 5-HT levels and degeneration of serotonergic neurons are associated with depressive symptoms. Findings regarding long-term depressive symptoms after MDMA use are conflicting and difficult to interpret given the variability in patterns of use and length on MDMA abstinence. This necessitates a review the present literature and an evaluation of future research directions. 10 MDMA and Depression The short-term effects of MDMA on mood have been well documented. Mood seems to elevate after MDMA ingestion. Depressed mood occurs in the next several days following use. This was clearly demonstrated in a study by Curran & Travill (1997). This study used a parallel group design to compare participants who had consumed MDMA and participants who had only consumed alcohol on day 1 of the study. The Beck Depression Inventory (BDI), a self-report inventory measuring symptoms of depression, was administered at day 1, day 2, and day 5 (Beck, Steer, Ball, & Ranieri, 1996). Scores less than 9 on the BDI are considered normal levels of depression (Beck & Steer, 1993). Participants were instructed not to use any psychoactive drugs after day 1 until termination of the study at day 5. On day 1, MDMA users had significantly lower BDI scores than alcohol-only users. BDI scores were similar between the two groups on day 2 both showing elevation from day 1. By day 5, MDMA users’ scores were higher at a mean of 11.75, outside of the normal range of depressive symptoms, whereas alcohol users’ scores were similar to their scores on day 1. Some MDMA users’ scores reached the level of clinical depression by day 5. These BDI scores support the notion that MDMA causes euphoric mood post-administration and acute depressive symptoms. The authors suggest that this acute increase in depressive symptoms following MDMA administration may be related to neurotoxic damage of serotonergic neurons. This explanation is supported by results from previous studies (Buchert et al., 2004; Reneman et al., 2001a; Reneman et al., 2001b). Evidence Not in Support of MDMA Specific Increases in Depressive Symptoms Several studies suggest that after the initial rise in depressive symptoms in the week following MDMA ingestion, MDMA users have clinically normal levels of depressive symptoms. The Beck Depression Inventory (BDI) or the more recent version, the BDI-II, has 11 been used frequently to assess depressive symptoms in MDMA users. De Win et al. used the BDI in a prospective design to determine if depression predicts ecstasy use or is the product of use (2006). Ecstasy naïve volunteers with a high probability of future use were recruited, as were persistently ecstasy-naïve subjects. The BDI was administered at baseline and every three months during a follow-up period of 18 months. Results showed no significant predictive effect of the baseline BDI score on future ecstasy use. There was also no effect of ecstasy use on depression. The absence of an effect of MDMA use on depression may be due to the exclusion of heavy users from this study. Ecstasy-induced depression may only be apparent at higher cumulative dosages. This agrees with several studies on animal models that found very large or multiple doses were necessary to produce neurotoxicity (Commins et al., 1987; Battaglia et al., 1988). Falck, Wang, Carlson, and Siegal researched the depressive effects due to the degree of ecstasy use (2006). Individuals who had used ecstasy in the past 6 months were recruited for this study, and these individuals were administered the BDI-II. Similar to the results of the de Win et al. study, results found that ecstasy users do not have clinically significant BDI-II scores (2006). However, using MDMA on 50 or more occasions was found to be a marginally significant correlate of clinically high BDI-II scores suggesting that larger doses may be necessary to produce an increase in depressive symptoms as measured by the BDI-II. This corresponds well with the damage to serotonergic neurons seen only after multiple administrations of MDMA in rats (Battaglia et al., 1988). Results of this study should be interpreted with caution as this study has many limitations. This study lacked a drug-naïve control group and a control group consisting of polydrug, excluding MDMA, users making correlations between BDI-II scores and MDMA use difficult. The retrospective design also does not allow for causal inferences to be 12 made. In contrast, results from a study by Guillot & Greenway suggest that total lifetime consumption is not even marginally related to depressive symptomology (2006). The aim of this study was to evaluate the relationship between recreational ecstasy use and depression as measured by the BDI-II. BDI-II scores of current ecstasy users and ecstasy-naïve college students were compared. Ecstasy users were required to abstain from the drug for one week before the study to control for acute effects. Results found that BDI-II scores did not differ significantly between the ecstasy user and control groups. Also, no significant correlations were found between BDI-II scores and conditions of ecstasy use such as total lifetime consumption of ecstasy, period of abstinence from ecstasy, and more ecstasy consumed in 12 hours. Results seem to indicate that ecstasy use is not related to depression. Clinically significant depressive symptoms may not have been seen due to the inclusion of many moderate users in this study. This would agree with findings from Reneman et al. demonstrating no neurotoxic effects in moderate users (2001a). A study by Falck, Wang, and Carlson expanded on these findings by using a longitudinal study to assess depressive symptomology in MDMA users over a two-year period (2008). Individuals who had used ecstasy in the past 6 months were recruited for this study. MDMA use in this sample was highly variable ranging from 1 to 1000 instances with the mean number of uses being 36.2. The BDI-II was administered at baseline and every six months for the next two years. During this time, most participants continued to use MDMA. Participants who had used MDMA on at least 50 occasions before baseline measurements had higher BDI-II scores than those who used less often. The association between cumulative ecstasy use and BDI-II score agrees with previous findings by Falck et al. but disagree with those of Guillot and Greenway 13 (2006; 2006). Mean BDI-II scores decreased over time from 9.8 at baseline to 7.7 at 24 months. BDI-II scores greater than 13 are considered to suggest significant depressive symptoms (Beck, Steer, & Brown, 1996). Both of these scores are not indicative of clinically significant depressive symptoms suggesting that for most people MDMA use does not result in depressive symptomology. Results suggest that the level of neurotoxicity resulting from MDMA use is not extensive enough to cause clinically significant depressive symptoms. The decrease in the low levels of depressive symptomology is consistent with the notion that MDMA mediated neurotoxicity is reversible although this would only apply to former MDMA users who had been abstinent for a period of time necessary to see a reversal of damage (Reneman et al., 2001a; Reneman et al., 2001b; Buchert et al., 2004). As for the majority of individuals in this study who continued to use MDMA, increased and stable levels of depression were expected due to the decrease in SERTs that has been documented in current MDMA users (Buchert et al., 2004; Reneman et al., 2001b). This, however, was not seen. Also of interest is the finding that men had lower levels of depressive symptomology compared to women. Given the findings Burchert et al. and Reneman et al. indicating higher susceptibility to MDMA mediated serotonergic neuronal damage in women, the higher level of depressive symptoms seen in females in this study may be due to greater damage of serotonergic neurons compared to that of men (2004; 2001a). One study has been conducted to evaluate long-term effects of MDMA use on depressive symptoms after a period of abstinence, a pattern of MDMA use closer to that in animal studies. Thomasius et al. investigated whether elevated psychopathology could be found in individuals using MDMA and whether any of these changes persisted after abstaining from the substance (2003). Data from current MDMA users, ex-MDMA users, polydrug users who did not use 14 MDMA, and drug-naïve controls were compared. All drug users abstained from all psychotropic substances for six days prior to testing. Participants were administered the Symptom Check List (SCL-90-R) to assess subjective perception of psychopathological symptoms. The SCL-90-R includes a depression subscale. All three groups of drug users had increased symptoms of psychopathology compared to controls as measured by the Global Severity Index (GSI) on the SCL-90-R. A similar pattern of increases was also seen in the depression subscale. These results suggest that there is no significant effect of MDMA use on psychopathology or depression beyond the use of other illicit drugs. The self reported number of ecstasy tablets taken on a typical occasion was however a predictor of the SLC-90-R subscale for depression. This is in line with the PET findings using [11C](+)McN5652. Multiple regression analyses found that the self reported number of ecstasy tablets taken on a typical occasion predicted reduction of SERT distribution volume ratios. In combination, these results suggests that MDMA serotonergic neuronal damage may predict levels of depression but that these levels of depression are not significantly greater than those seen by polydrug users or ex-MDMA users. A limitation to studies evaluating depression as an outcome of a specific environmental factor, like the studies discussed above, is the presence of confounding variables. A study by Scott, Hides, Allen, Burke, & Lubeman attempted to control for known environmental and genetic risk factors for depression to clarify the relationship between ecstasy use and depressive symptomology (2010). Participants consisted of individuals who had taken ecstasy at least once in the past 12 months. Mood symptoms were assessed using the Mood and Anxiety Symptom Questionnaire—Short Form (MASQ; Watson & Clark, 1991). This self-report inventory contains a scale of depressive symptomology. DNA was extracted and analyzed for serotonin transporter gene (5-HTTLPR). Traumatic life events were measured using the Composite 15 International Diagnostic Interview—Trauma List (World Health Organization, 1997). Participants were also asked if they had experienced any major stressful life events in the preceding month. Events were categorized using the subject areas from the Psychiatric Epidemiological Research Interview—Life Events Scale (Dohrenwend, Krasnoff, Askenasy, & Dohrenwend, 1978). Results show that neither lifetime nor recent ecstasy use was associated with current mood symptoms. This was found before and after controlling for genetic and environmental risk factors for depression. Mean lifetime use was 172.4 pills with a standard deviation of 507.4 suggesting that the lack of depressive symptoms are not due to moderate ecstasy use. As would be expected, lifetime history of trauma and stressful life events were significant predictors of severe depressive symptoms. This indicated that depressive symptoms in this sample were related to environmental risk factors and not 5-HTTLPR genotype or ecstasy use. These variables may play more significant roles in depression than damage to serotonergic neurons. Evidence of Clinically Significant Levels of Depression in MDMA Users In contrast to results discussed above, several studies show a relationship between MDMA use and depression. McCardle, Luebbers, Carter, Croft, & Stough evaluated differences in depressive symptoms between MDMA users and MDMA-naïve controls (2004). In the MDMA group, total lifetime consumption ranged from use on two occasions to more than 30. The average time since last use ranged from one week to 4.5 months. Participants were administered a drug history questionnaire and the BDI-II. The MDMA group had significantly higher BDI-II scores (M = 12.35, SD = 9.41) than controls (M = 5.53, SD = 4.64). Scores in the MDMA group approached clinical significance. MDMA users were abstinent from the drug for an average of 130 days, suggesting that depressive symptoms may not be the result of a 16 temporary decline in 5-HT concentration but may instead by a result of 5-HT neurotoxicity. The average time of MDMA abstinence agrees with several neuroimaging studies of 5-HT neurotoxicity in humans (Reneman et al., 2001a; Reneman et al., 2001b). These neuroimaging studies saw a decrease in SERT density in users who has abstained up to about 5 months compared to controls. However no significant decrease in SERT availability was seen in users who had been abstinent for over a year when compared to controls. Users in this study had not been abstinent for longer than 4.5 months suggesting that they still have significant 5-HT neurotoxic damage. Results of this study should be interpreted with caution, as there were significant differences between the two groups in use of cannabis, hallucinogens, amphetamines, alcohol, other opiates, tranquillizers, barbiturates, and tobacco. Therefore the elevated BDI-II scores in MDMA users may have resulted from the higher use of drugs other than MDMA. Despite these limitations, results from MacInnes, Handley, & Harding also show longterm depressive symptoms resulting from MDMA use (2001). Participants consisted of former chronic ecstasy users who must have abstained from ecstasy for the past 14 days or longer and drug-naïve controls. Participants were administered the BDI. This experiment also controlled for potential confounding variable such as life stress. The frequency of life stress was assessed using the Social Readjustment Rating scale (SRRS) and the Daily Hassles scale. Former chronic users had significantly higher BDI scores than the matched drug-naïve controls. The BDI scores were positively correlated with ‘maximum tablets consumed in 12 h’ but not with the total number of tablets consumed. Multiple regressions revealed that the Daily Hassles scale and the ‘number of ecstasy tablets consumed in 12 h’ were significant predictors of BDI score. Higher doses in a short amount of time may have caused an extensive amount of damage that was irreversible, resulting in higher BDI scores even after ecstasy abstinence. The reversibility of 17 damage may play a role in long-term use, as seen in total number of tablets consumed, because damage may have decreased over time before the next tablet was consumed. These results are difficult to interpret given previous findings on MDMA mediated neurotoxicity in humans. Former chronic users were abstinent from ecstasy for 14 days or longer with the mean length of ecstasy abstinence being 26 weeks. According to Buchert et al., SERT availability in MDMA users who had been abstinent for 20 weeks or more was similar to controls (2004). According to this data, damage to serotonergic neurons should have reversed by the mean time of abstinence in this study, 26 weeks. The persistent depressive symptomology is not consistent with the time frame of reversibility. However, the variability in length of ecstasy abstinence in this study was very large making it is hard to compare mood outcomes to 5-HT neurotoxicity. Conclusions and Future Directions At present, several conclusions can be made regarding MDMA mediated neurotoxicity. Both rats and nonhuman primates appear to show significant decrease sin 5-HT and SERTs following MDMA administration (Commins et al., 1987; Battaglia et al., 1988; Wilson et al., 1989; Ricaurte et al., 1992). In rats, this damage is completely reversible by 1 year postadministration (Battaglia et al., 1988). In primates, this damage appears to be more permanent in the long-term (Ricaurte et al., 1992). Significant decreases in SERTs are also seen in current, human MDMA users. This damage is not apparent in ex-users suggesting that MDMA mediated neurotoxicity is reversible in humans (Buchert et al., 2004; Reneman et al., 2001b). Results pertaining to correlations between MDMA use and symptoms of depression in humans are contradictory. Several studies suggest that MDMA does not have any specific effects on elevated symptoms of depression (de Win et al., 2006; Falck et al., 2006; Guillot & Greenway, 2006; Falck et al., 2008; Thomasius et al., 2003; Scott et al., 2010). Conversely, 18 results from several studies show that current MDMA users and ex-MDMA users show clinically elevated levels of depression (McCardle et al., 2004; MacInnes et al., 2001). There are many difficulties in comparing results between studies on depressive symptoms in current or ex-MDMA users. Studies differ in extent and patterns of use as well as in length of abstinence from MDMA. These factors are likely to play significant roles in the degree of neurotoxicity and presence of depressive symptoms. It is also difficult to compare studies evaluating depressive symptomology in humans with studies on MDMA mediated neurotoxicity in animal models. The patterns of MDMA within human studies differ form those used in animal studies making it difficult to relate these findings to those of 5-HT neuronal damage. For example, in animal studies MDMA is administered to animals on a set schedule for a set amount of time. The brains of these animals are either assessed soon after administration of after a given period of abstinence. This clearly differs from the use patterns of humans. Studies involving continued use of MDMA are particularly hard to compare to studies involving animals models because the cumulative exposure to MDMA from continued use is likely to have a different effect on the brain than discontinuation of use. Further study should be done to help clarify these findings and to help link findings of 5HT axonal damage with depressive symptomology. Studies should be conducted to compare SERT presence in MDMA users who have abstained for differing, predetermined amounts of time with those of drug-naïve controls. PET using [11C](+)McN5652 or SPECT using [123I]CIT could be used to evaluate the presence of SERTs. The BDI-II should be administered on the day of scanning. This is similar to the design used by Thomasius et al. however there should be a higher degree of control over participant characteristics (2003). For example, ex-MDMA users included in the study should have similar patterns of MDMA use, similar cumulative lifetime use 19 of MDMA, and limited use of other psychoactive substances. Although this design is idealistic in terms of inclusion criteria, future studies should strive to meet these standards. At this juncture, there is not enough available evidence to reach any significant conclusions regarding depressive symptomology resulting from MDMA mediated damage to serotonergic neurons. 20 References Battaglia, G., Yeh, S. Y., & De Souza, E. B. (1988). MDMA-Induced neurotoxicity: parameters of degeneration and recovery of brain serotonin neurons. Pharmacology Biochemistry & Behavior, 29, 269-274. Beck, A. T., & Steer, R. A. (1993). Beck depression inventory manual. San Antonio, TX: Psychological Corporation. Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck depression inventory manual (2nd ed.). San Antonio, TX: The Psychological Corporation. Beck, A., Steer, R., Ball, R., Ranieri, W. (1996). Comparison of Beck Depression Inventories-IA and –II in psychiatric outpatients. Journal of Personality Assessment, 67, 588-597. Buchert, R., Thomasius, R., Wilke, F., Petersen, K., Nebeling, B., Obrocki, J., Schulze, O., Schmidt, U., & Clausen, M. (2004). A voxel-based PET investigation of the long-term effects of “ecstasy” consumption on brain serotonin transporters. American Journal of Psychiatry, 161, 1181-1189. Commins, D. L., Vosmer, G., Virus, R. M., Woolverton, W. L., Schuster, C. R., & Seiden, L. S. (1987). Biochemical and histological evidence that methylenedioxymethylamphetamine (MDMA) is toxic to neurons in the rat brain. The Journal of Pharmacology and Experimental Therapeutics, 241(1), 338-345. Curran, H. V., & Travill, R. A. (1997). Mood and cognitive effects of ±3,4methylenedioxymethamphetamine (MDMA, ‘ecstasy’): week-end ‘high’ followed by mid-week low. Addiction, 92(7), 821-831. 21 de Win, M. L., Schilt, T., Reneman, L., Vervaeke, H., Jager, G., Dijkink, S., Booij, J., & van den Brink, W. (2006). Ecstasy use and self-reported depression, impulsivity, and sensation seeking: a prospective cohort study. Journal of Psychopharmacology, 20(2), 226-235. Dohrenwend, B. S., Krasnoff, L., Askenasy, A. R., & Dohrenwend, B. P. (1978). Exemplifications of a method for scaling life events: the PERI Life Events Scale. Journal of Health and Social Behavior, 19, 205-229. Falck, R. S., Wang, J., & Carlson, R. G. (2008). Depressive symptomatology in youth adults with a history of MDMA use: a longitudinal analysis. Journal of Psychopharmacology, 22(1), 47-54. Falck, R. S., Wang, J., Carlson, R. G., & Siegal, H. A. (2006). Prevalence and correlates of current depressive symptomology among a community sample of MDMA users in Ohio. Addictive Behaviors, 31, 90-101. Green, A. R., Mechan, A. O., Elliott, J. M., O’Shea, E., & Colado, M. I. (2003). The pharmacology and clinical pharmacology of 3,4-methylenedioxymethampheramine (MDMA, “ecstasy”). Pharmacological Reviews, 55(3). 463-508. Guillot, C., & Greenway, D. (2006). Recreational ecstasy use and depression. Journal of Psychopharmacology, 20(3), 411-416. MacInnes, N., Handley, S. L., & Harding, G. F. A. (2001). Former chronic methylenedioxymethamphetamine (MDMA or ecstasy) users report mild depressive symptoms. Journal of Psychopharmacology, 15(3), 181-186. Malison, R. T., Price, L. H., Berman, R., van Dyck, C. H., Pelton, G. H., Carpenter, L., Sanacora, G., Owens, M. J., Nemeroff, C. B., Rajeevan, N., Baldwin, R. M., Seibyl, J. P., Innis, R. B., & Charney, D. S. (1998). Reduced brain serotonin transporter availability in major 22 depression as measured by [123I]-2-carbomethoxy-3-(4-iodophenyl)tropane and single photon emission computed tomography. Biological Psychiatry, 44, 1090-1098. McCardle, K., Luebbers, S., Carter, J. D., Croft, R. J. & Stough, C. (2004). Chronic MDMA (ecstasy) use, cognition and mood. Psychopharmacology, 173, 434-439. O’Hearn, E., Battaglia, G., De Souza, E. B., Kuhar, M. J., & Molliver, M. E. (1988). Methylenedioxyamphetamine (MDA) and methylenedioxymethamphetamine (MDMA) cause ablation of serotonergic axon terminals in forebrain: immunocytochemical evidence. Journal of Neuroscience, 8, 2788-2803. Reneman, L., Booji, J., de Bruin, K., Reitsma, J. B., de Wolff, F. A., Gunning, W. B., den Heeten, G. J., &van den Brink, W. (2001a). Effects of dose, sex, and long-term abstention from use on toxic effects of MDMA (ecstasy) on brain serotonin neurons. The Lancet, 358, 1864-1869. Reneman, L., Lavalaye, J., Schmand, B., de Wolff, F. A., ven den Brink, W., den Heeten, G. J., & Booij, J. (2001b). Cortical serotonin transporter density and verbal memory in individuals who stopped using 3,4-methylenedioxymethamphetamine (MDMA or “ecstasy”). Archives of General Psychiatry, 58, 901-906. Ricaurte, G. A., Martello, A. L., Katz, J. L., & Martello, M. B. (1992). Lasting effects of (±)-3,4methylenedioxymethamphetamine (MDMA) on central serotonergic neurons in nonhuman primates: neurochemical observations. The Journal of Pharmacology and Experimental Therapeutics, 261(2), 6161-622. Scott, R. M., Hides, L., Allen, J. S., Burke, R., & Lubman, D. I. (2010). Depressive and anxiety symptomatology in ecstasy users: the relative contribution of genes, trauma, life stress and drug use. Psychopharmacology, 209, 25-36. 23 Thomasius, R., Peterson, K., Buchert, R., Andersen, B., Zapletalova, P., Wartberg, L., Nebeling, B., & Schmoldt, A. (2003). Mood, cognition and serotonin transporter availability in current and former ecstasy (MDMA) users. Psychopharmacology, 167, 85-96. Watson, D., & Clark, L. A. (1991). The mood and anxiety symptom questionnaire. Iowa City: University of Iowa. Wilson, M. A., Ricaurte, G. A., & Molliver, M. E. (1989). Distinct morphologic classes of serotonergic axons in primates exhibit differential vulnerability to the psychotropic drug 3,4-methylenedioxymethamphetamine. Neuroscience, 28(1), 121-137. World Heath Organization. (1997). Composite international diagnostic interview (version 2.1). Geneva: World Health Organization.