Hospital Claims Data FAQ For Super-Utilizer Interventions
advertisement

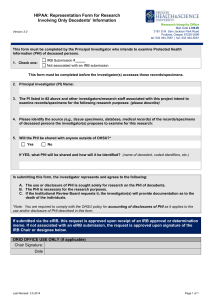
Hospital Claims Data FAQ For Super-Utilizer Interventions What is hospital claims data? Hospitals collect data related to the billable activities the hospital system performs for its patients. Hospital claims data includes total hospitalization costs (what is billed and what is reimbursed), date of admission, date of discharge, diagnosis codes related to the hospitalization, insurance, address, and date of birth for each patient and each hospitalization. Hospital claims data is historical data. It takes weeks for the hospital to enter and assemble claims data related to individual hospitalizations. How will having access to hospital claims data help a super-utilizer intervention? When you are just starting a super-utilizer intervention, hospital claims data will help you understand the hospital utilization background of the patients you are working with. If you can review 6-12 months of hospital claims data for each of the patients in the intervention, you can identify: total costs of care for each patient before your intervention and compare it with costs during/after your intervention the diagnoses and treatments each patient recently received how long your super-utilizer patient has stayed in the hospital before your intervention or how often the patient was readmitted These data points can help direct your intervention with each patient and begin to develop larger lessons for your work with super-utilizers. If you are able to collect 6-12 months of hospital claims data for an entire hospital or entire community, you can begin to understand community-level patterns, including: total costs of care for super-utilizing patients in your community common diagnoses for super-utilizing patients in your community how long super-utilizer patients have stayed in the hospital or how often super-utilizers have been readmitted. Community level data is important to developing the broad story about what is happening with super-utilization in your area, how it affects overall care and costs, and what kinds of providers/partners needs to collaborate to address the issue(s). Hospital claims data will not help you identify potential patients for your intervention. In order to identify patients for an intervention you need close to realtime data so that you can identify and intervene with patients who are in the hospital or very recently discharged. You can get real-time data either through a health information exchange (HIE) or through the ADT (admission/discharge/transfer) feeds from your partnering hospital(s). What is the process for obtaining hospital claims data? Hospital claims data can be requested through individual patient consent or through a comprehensive data sharing agreement with a hospital. When making a hospital claims data request be sure to ask for total hospitalization costs (what is billed and what is reimbursed), date of admission, date of discharge, diagnosis codes related to the hospitalization, insurance, address, and date of birth for each patient and each hospitalization. 1) Individual patient consent The easiest way to get hospital claims data is to have patients enrolled in your super-utilizer intervention collect their own claims data. Patients must contact the billing department at each hospital they have visited and provide whatever consent the hospital claims department requires. Patients can also provide consent for someone else, such as a member of the super-utilizer team, to access this information on their behalf. Often there is no official form for the patient to complete; rather, the hospital may ask for a written, signed letter that states the name of individual authorized to receive claims data, the specific information being requested and the period of claims sought. 2) Data sharing agreement with a hospital Hospitals may enter into agreements that will allow the hospital to share its claims data with a third party / outside organization that will coordinate care for its super-utilizers. These agreements allow individual patient data to be shared without an individual consent to be signed. Usually, a Memorandum Of Understanding (MOU) or a Collaborative Services Agreement (CSA) is used to describe and govern the super-utilizer care coordination activities that will be undertaken, and the role each party will play. If the hospital claims data, which includes protected health information (PHI), will be shared electronically, a Business Associates Agreement may also be necessary to ensure that the exchange of data will be fully compliant with federal law (HIPAA). Samples of these agreements are available on the Camden Coalition’s website.1 3) Institutional Review Board (IRB) Hospital claims data may also be made available through the hospital’s IRB 1 http://www.camdenhealth.org/about/resources-2/contracts/ 2 approval process. In addition to permitting the exchange of hospital claims information, an IRB agreement allows you to conduct research on your super-utilizer intervention. Talk to your hospital partner(s) about how to pursue IRB approval. Why is it important for a hospital to share hospital claims data with a superutilizer intervention? There are specific benefits to hospitals that can support a super-utilizer intervention by providing data to the program. Super-utilizing patients who regularly cycle in and out of the hospital are generally expensive for the hospital to treat, and they divert resources from others who need emergency department and inpatient care. A successful super-utilizer intervention will reduce these burdens on any participating hospital. A super-utilizer intervention may also lower the hospital’s 30-day readmission rate, which will keep the hospital from losing Medicare funding. Lastly, super-utilizers often visit more than one hospital in a community. Identifying and intervening with super-utilizers is not something an individual hospital. By sharing data with community-wide super-utilizer intervention, a hospital can gain efficiencies and effective care that would be outside of its individual capacity. How does HIPAA impact the collection of hospital claims data? HIPAA permits hospitals to use and disclose their patients’ protected health information (PHI), including hospital claims data, for the purposes of treatment, payment and healthcare operations without obtaining individual patient consent. Most super-utilizer interventions are a form of “treatment” because they include the “provision, coordination, or management of health care and related services among health care providers or by a health care provider with a third party.” 2 If a hospital identifies your program as a third party that will coordinate care for its super-utilizers, that hospital may share information, including hospital claims data, about its patients who may be eligible for the intervention without obtaining prior patient consent. Does HIPAA require the protection of hospital claims data? Your program should be careful to comply with HIPAA by safeguarding all patient information. HIPAA protects all individually identifiable health information, known as protected health information (PHI), which includes name, address, birth date, Social Security number, information that relates to the individual’s physical or For information about uses and disclosures for treatment, payment, and health care operations, see: http://www.hhs.gov/ocr/privacy/hipaa/understanding/coveredentities/usesanddisclosuresfortpo. html. 2 3 mental health condition, and the provision of or payment for health care to the individual. To make sure that PHI is not disclosed improperly, only save PHI on an encrypted hard drive, and send any electronic communications containing PHI through a secure email server. Furthermore, any disclosure of PHI should be limited to information that is necessary to carrying out the care coordination intervention. The hospitals you work with are a terrific source of information about HIPAA. Generally, a hospital will have a Director of Compliance who can explain their policies regarding PHI. 4 Hospital Claims Data FAQ For Super-Utilizer Interventions Four Roles of Data in a Healthcare High Utilization Intervention Quantify the high utilizer problem Can hospital claims data help? Yes. Claims data includes records for each visit to the emergency room or inpatient stay. The data can be reorganized in a way that summarizes the yearly utilization (# ED and # IP visits), charges and receipts for each patient. Analysis of this data can be used to quantify the number and cost of high utilizers to the local healthcare system. What specific claims data variables are essential to have for this component? Unique patient id is needed in order to take individual claims records and turn them into an aggregate utilization history. What are the specific software needs? Data analysis and visualization software If data is being merged from multiple hospital systems, master patient index software is needed in order merge patient utilization from multiple hospitals. Develop interventions to target the high utilizer problem Yes. Further analysis of the claims data can be used to facilitate a discussion on what interventions are needed and how many patients a program will need to serve in order to significantly reduce costs. Identify and engage patients needed a high utilizer intervention No. In order to identify patients for an intervention you need close to realtime data. For example, the best time to begin an intervention with an inpatient high utilizer is when they are currently in the hospital. Claims data is historical data and cannot identify current inpatients with a history of high utilization.* Patient address is necessary in order to explore geographic hotspots. NA Data analysis and visualization software ArcGIS mapping software NA *Real time data for identifying patients for an intervention can be gathered in one of two ways: Evaluate the impact of the intervention on the problem Yes. Identifying historic claims data for patients receiving an intervention can be used to evaluate program impact. For example, calculating a patients total costs 6 months prior to program enrollment and 6 months post enrollment can quantify the impact on that particular patients. Aggregating this information for all program participants will quantify the total program impact. Patient name and date of birth from the claims data is needed in order to link the claims data to patients participating in the intervention Data analysis and visualization software 1) If your community has a Health Information Exchange (HIE), the HIE data can be used to create a daily report of current hospital inpatients classified as high utilizers. HIE’s provide a more accurate identification of high utilizers because the system aggregates data across hospitals and thus can identify a patient classified as high utilizers when aggregating utilization across hospitals. 2) If you do not have an HIE you can work with individual hospitals to generate a list of patients currently admitted to that hospital that have been admitted to that particular hospital 2 or more time in the last 6 months. This option would miss cross-hospital system high utilizers, but should provide an ample number of patients for potential enrollment. They key component of this option is developing a partnership with the hospital to run this list daily and provide access to the list.