Apparent Hepatitis B Seroconversion in an
advertisement
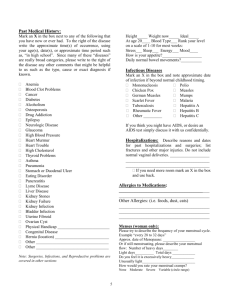
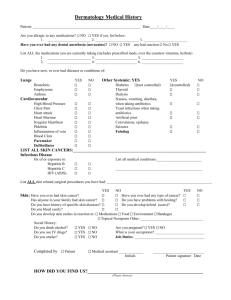
P155 APPARENT HEPATITIS B SEROCONVERSION IN AN IMMUNE HAEMODIALYSIS PATIENT - IMPORTANT LESSONS FOR CLINICAL PRACTICE Chandna, S, Awadel-Kariem, F, Samme, S, Farrington, K Lister Hospital, Stevenage Risk of transmission of blood-borne viruses (BBV) is a major issue in haemodialysis units., Hepatitis B seroconversion rates of 0.1 to 0.4 per 100 patient-years have been quoted in United States and UK. For Hepatitis C, the rates have been 0.2 to 2 per 100 patient-years. It is assumed that most patients with acute Hepatitis B infection recover completely and once they become Hepatitis B S Ag negative, they no longer pose infection risk to others. This is reflected in Renal Association (RA) guidelines which suggest that patients with antibodies to Hepatitis B need to be tested once a year. Hepatitis B Seroconversion is a major event in a haemodialysis unit with potentially serious consequences. We describe a case of apparent seroconversion in a 71 years old woman of Asian origin who was previously Hepatitis B S Ag negative with Anti-HB S level was 278. On routine testing she was found to be seroconverted to Hepatitis B S Ag positivity, with Anti HB S level falling to <10. She had 2.4 X 108/ml Hepatitis B DNA in her blood. After extensive testing, transmission from within dialysis unit or any other source of infection was ruled out. Detailed analysis of historical samples revealed that, eighteen months prior to her Hepatitis B seroconversion, she had low level (240 copies/ml) Hepatitis B DNA in her blood despite negative Hep B S Ag, equivocal Hep B Core Antibody and highly positive Hepatitis B S Antibody (277 miu/ml). It was therefore concluded that this was reactivation of previously acquired infection. Hepatitis B was of genotype D, which is common in Bangladesh where this patient was hospitalised two years previously. This patient was tested for Hepatitis B at 3 monthly intervals, however – in view of her Anti HB S level – RA guidelines recommend yearly testing for her which would have posed infection risk to other haemodialysis patients for much longer. Unlike US guidelines, British guidelines do not recommend testing for Hep B Anti Core Antibody which is an important marker of previous infection. We suggest Anti Core testing in all patients starting haemodialysis. Those found to be positive, should have Hepatitis B DNA checked and have monthly Hep B S Ag screening. Role of haemodialysis machines in BBV transmission has been debated. Until her Hepatitis B S Ag was found to be positive, our patient was dialysed in the main unit for at least a month in a highly infectious state. Haemodialysis machines were not disinfected between dialysis sessions, yet no other patient acquired infection from her, which argues against the need for machine isolation and routine disinfection between patients, and emphasises the importance of universal precaution.