What Do Practitioners want from a Diagnostic Taxonomy?
advertisement
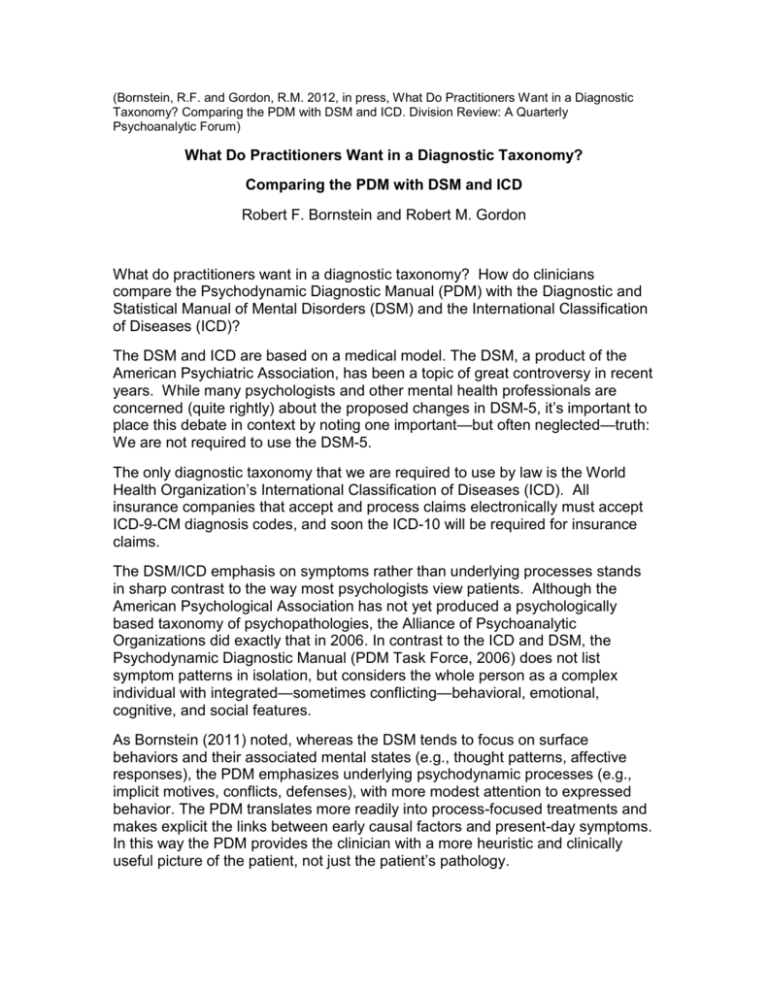
(Bornstein, R.F. and Gordon, R.M. 2012, in press, What Do Practitioners Want in a Diagnostic Taxonomy? Comparing the PDM with DSM and ICD. Division Review: A Quarterly Psychoanalytic Forum) What Do Practitioners Want in a Diagnostic Taxonomy? Comparing the PDM with DSM and ICD Robert F. Bornstein and Robert M. Gordon What do practitioners want in a diagnostic taxonomy? How do clinicians compare the Psychodynamic Diagnostic Manual (PDM) with the Diagnostic and Statistical Manual of Mental Disorders (DSM) and the International Classification of Diseases (ICD)? The DSM and ICD are based on a medical model. The DSM, a product of the American Psychiatric Association, has been a topic of great controversy in recent years. While many psychologists and other mental health professionals are concerned (quite rightly) about the proposed changes in DSM-5, it’s important to place this debate in context by noting one important—but often neglected—truth: We are not required to use the DSM-5. The only diagnostic taxonomy that we are required to use by law is the World Health Organization’s International Classification of Diseases (ICD). All insurance companies that accept and process claims electronically must accept ICD-9-CM diagnosis codes, and soon the ICD-10 will be required for insurance claims. The DSM/ICD emphasis on symptoms rather than underlying processes stands in sharp contrast to the way most psychologists view patients. Although the American Psychological Association has not yet produced a psychologically based taxonomy of psychopathologies, the Alliance of Psychoanalytic Organizations did exactly that in 2006. In contrast to the ICD and DSM, the Psychodynamic Diagnostic Manual (PDM Task Force, 2006) does not list symptom patterns in isolation, but considers the whole person as a complex individual with integrated—sometimes conflicting—behavioral, emotional, cognitive, and social features. As Bornstein (2011) noted, whereas the DSM tends to focus on surface behaviors and their associated mental states (e.g., thought patterns, affective responses), the PDM emphasizes underlying psychodynamic processes (e.g., implicit motives, conflicts, defenses), with more modest attention to expressed behavior. The PDM translates more readily into process-focused treatments and makes explicit the links between early causal factors and present-day symptoms. In this way the PDM provides the clinician with a more heuristic and clinically useful picture of the patient, not just the patient’s pathology. We believe that DSM and ICD diagnoses should be integrated with PDM process-focused data to enhance case conceptualization and treatment planning. To facilitate this sort of integration we developed a clinician-friendly coding form—the Psychodiagnostic Chart (PDC)—that allows the practitioner to combine DSM and ICD diagnostic data with PDM-derived information regarding level of personality organization, overall mental functioning, and other salient psychological variables. (You can obtain copies of the PDC from either of us; email rmgordonphd@rcn.com, or bornstein@adelphi.edu.) The impetus for the PDC came from Gordon’s (2009) survey data, which suggested that practicing clinicians of various theoretical orientations find the PDM useful in conceptualizing patients. To address questions of what practitioners want in a diagnostic taxonomy, and how practitioners compare the PDM with the DSM and ICD, we conducted a follow-up study, recruiting expert practitioners from various state psychology listservs, the Division 39 website, and other psychology websites. We asked them to: 1) use the PDC with at least one patient, and then 2) complete an online survey evaluating key features of the PDM, DSM, and ICD. Fifty practitioners have taken the survey to date, with 80% of respondents having doctorates and 20% masters degrees; 54% were women. Half of the respondents identified themselves as Psychodynamic (50%); the rest were Eclectic (22%), Cognitive-Behavioral (12%), Humanistic/Existential (10%), Systems (4%), and Other (2%). Practitioners rated on 7-point scales how useful various PDM-derived diagnostic dimensions were in understanding one’s patients, and we contrasted these ratings with practitioners’ ratings of information derived from DSM and ICD (1 = Not at All Helpful; 7 = Very Helpful). Some preliminary findings: 68% rated PDM Personality Structure as “helpful-very helpful.” 58% rated PDM Mental Functioning as “helpful-very helpful.” 44% rated PDM Dominant Personality Patterns or Disorders as “helpfulvery helpful.” In contrast: 18% rated DSM GAF scores as “helpful-very helpful.” 14% rated ICD or DSM symptoms as “helpful-very helpful.” Additional analyses suggested that the utility of the PDM is not limited to analytic therapists: Practitioners with other theoretical orientations rated PDM derived constructs as positively as did psychodynamic practitioners. Thus, the PDM may be useful to clinicians from an array of theoretical perspectives. Moving forward, the PDC may help facilitate use of the PDM in clinical and research settings, and allow clinicians to integrate DSM/ICD and PDM data more easily. As work begins on the PDM-2, such assessment tools promise to play a central role in enhancing psychodynamic assessment, diagnosis, and treatment. References Bornstein, R. F. (2011). From symptom to process: How the PDM alters goals and strategies in psychological assessment. Journal of Personality Assessment, 93, 142-150. Gordon, R. M. (2009). Reactions to the Psychodynamic Diagnostic Manual (PDM) by psychodynamic, CBT, and other non-psychodynamic psychologists. Issues in Psychoanalytic Psychology, 31, 55-62. PDM Task Force. (2006). Psychodynamic Diagnostic Manual. Silver Spring, MD: Alliance of Psychoanalytic Organizations.