abstract guidelines
advertisement

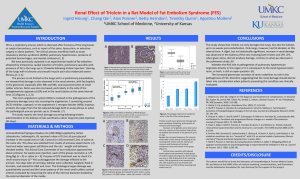
How to write an abstract A. Title B. Authors and Co-Authors The body of an abstract is usually organized into 4 main sections: C. Purpose/Goal/Hypothesis This section generally will include a very concise statement regarding the background for the study and then should state the goal of the proposed study. D. Methods E. Results F. Summary or conclusion C. Goal section This section should provide the reader with the importance of the subject area you will pursue, i.e., what is the clinical or scientific significance and what problems or questions remain to be answered. It is here that you state your hypothesis and concisely define your goal(s). Keep it brief and to the point. D. Methods section This section should state briefly the technical approach you will use, lab animals, human subjects, techniques to be used, facilities, etc. E. Results section This section will depend upon whether you have done any data. If so, briefly describe them. If not, you should briefly discuss the expected results or possibilities. F. Summary/conclusion section In this section, briefly discuss the important findings and how it does or does not support your original hypothesis. If not, state why your proposal is a worthwhile project. What benefit will be gained? What will your project lead to? Sample Abstract TITLE: Timed Fat Feeding in Rats Induce Diurnal Variation in Vascular Function Authors: Samantha Medical Student, Joe Advisor, Jill Advisor, Dept. of Research, KSOM Goal: Recent evidence in mice, demonstrates that fat feeding restricted to 8 hours during the night, prevents obesity and its associated abnormalities. In light of these findings, we undertook the current study to examine the effects of restricted timed fat feeding on vascular function. Methods: Male Wistar rats (n=10) with initial weights of 262± 6.2 g were fed control (C, n=3) or 60% high fat (HF, n=2) diets either during the day (D) from 7am-7pm, (lights on) or during the night (N) from 7pm-7am, (lights off) for a period of 3 weeks (w). Body weight (BW) and food intake were measured bi-weekly and daily, respectively. For assessment of vascular function, thoracic aortas were isolated and cut into 3 mm rings and suspended in tissue baths with an optimal passive tension of 3 g for measurement of isometric tension. Results: Total caloric intake over the 3 w was 11% less in HF-D rats compared to HF-N, 1313 vs. 1166 kilocalories (p<0.001). BW increased significantly in all groups, but did not differ among groups, average weight at time of sacrifice (361 ± 23.4g, p<.05 vs initial wt). Interestingly, 3 w of timed fat diet resulted in differential vascular responses to the vasoconstrictor phenylephrine, whereas the maximal contractile responses to cumulative doses of PE were significantly reduced in HF-D rats, reaching only 28% of baseline compared to Con (>80% for both D and N) and HF-N (50%) (p<.05 HF-D vs. Con) Conclusions: These data demonstrate evidence for development of vascular dysfunction prior to significant weight gain during fat loading. These data also show that fat feeding restricted to the day when rats are inactive, may have a more deleterious effect on vascular function.