outline31206

Management of the Corneal Graft
I.
Graft Basics a.
Terminology i.
Allograft ii.
Autograft iii.
Failure
1.
Primary/Iatrogenic
2.
Late iv.
rejection v.
Tissue v Organ transplant b.
Corneal Graft Basics i.
History of grafting
1.
PK
2.
EK a.
1970s group b.
Modern incarnation and differences
3.
DALK
4.
Role of OD in care of the corneal graft a.
Historically visual rehabilitation i.
50% require rgp b.
More of a shift as co-management develops to preservation of graft – ie prevention of graft failure ii.
Cornea review
1.
Function a.
Tectonic b.
Optical c.
How are these achieved
2.
Key physiologic concepts in K transplants a.
Immune privileged nature of cornea i.
Lack of vascularization b.
Endothelial Pump function c.
Neurotrophic nature of grafts d.
Risk of infection iii.
Indications of Corneal Grafting
1.
Tectonic a.
PK b.
EK in Keratoectasia pt example(john Ketterling)
2.
Optical a.
Corneal edema b.
Corneal irregularity c.
Scarring
iv.
Graft survival
1.
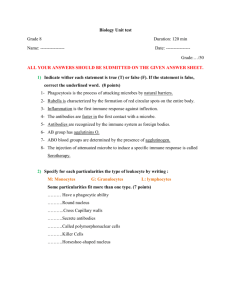
Graft Rejection a.
What is rejection i.
White blood cells attacking the graft ii.
What is the target of rejection – nucleated cells
1.
Epi Rejection
2.
Stromal Rejection
3.
Endothelial rejection b.
Requires evidence of immune function c.
Features which increase risk of rejection d.
How are the different graft types different when it comes to rejection risk e.
Treatment of rejection
2.
Endothelial Pump Failure a.
Primary Graft Failure i.
How to classify ii.
Graft that doesn’t clear or adhere within 6 weeks is the technical definition, of course with EKs this time frame is usually not observed prior to refloating b.
Late Graft Failure i.
Average percentage of Endo decomp upon transplant ii.
Average rate of endo decomp post transplant iii.
Expected life span iv.
Signs of late graft failure v.
Treatment of late graft failure c.
Endothelial Rejection d.
How are different graft types impacted by endothelial pump failure i.
DALKs risk of iatrogenic damage to host endo
3.
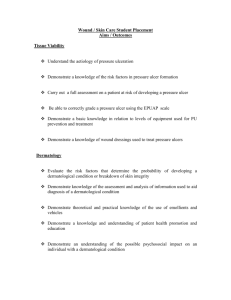
Neurotrophic features a.
Why are anterior grafts neurtophic? i.
Elimination of neural reflex between the cornea, lid and lacrimal apparatus ii.
Pre-existing neurotrophic states secondary to prior herpetic eye disease – a relatively common indication for anterior graft b.
Treatment of neurotrophic grafts i.
ATS
ii.
Restasis iii.
BSCL iv.
Tarrsorhaphy v.
Autologous serum vi.
Amniotic Membrane
4.
Infection a.
Why do anterior grafts have increased risk of infection i.
Use of corticosteroids ii.
Recurrence of virus in graft iii.
Use of contact lenses
5.
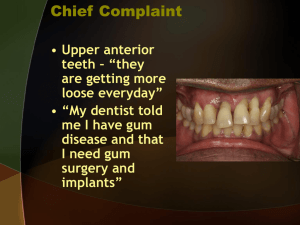
Case Reviews a.
Rejection i.
PK ii.
EK b.
Infection, new c.
Infection recurrent i.
HSV d.
Vascularization i.
Use of anti-VEGF medications e.
Neurtophic issues i.
Use of amniotic Membrane sutured ii.
Use of amniotic membrane with Prokerra f.
Wound dehiscence/rupture i.
PK ii.
DALK iii.
EK g.
Primary Graft Failure/EK h.
Endothelial pump failure i.
Pump failure in previous PK treated with rePK vs EK