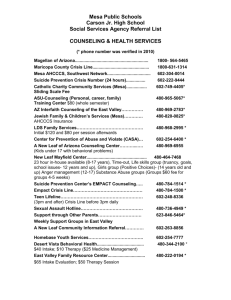
Univ Physicians Healthcare
advertisement

___________________________________________________________________________________________ UNIVERSITY PHYSICIANS HEALTHCARE dba THE UNIVERSITY OF ARIZONA HEALTH PLANS PROVIDER SERVICE AGREEMENT FOR Yavapai County Community Health Services Effective: TBD _________________________________________________________________________________________ UNIVERSITY PHYSICIANS HEALTHCARE dba THE UNIVERSITY OF ARIZONA HEALTH PLANS PROVIDER SERVICE AGREEMENT TABLE OF CONTENTS RECITALS .............................................................................................................................................................................. 3 AGREEMENT ......................................................................................................................................................................... 3 EXHIBIT SCHEDULE ........................................................................................................................................................... 24 EXHIBIT 1. ........................................................................................................................................................................... 25 EXHIBIT 2. COMPENSATION-ANCILLARY .............................................................. ERROR! BOOKMARK NOT DEFINED. EXHIBIT 2A. COMPENSATION CARVE-OUTS ........................................................ ERROR! BOOKMARK NOT DEFINED. EXHIBIT 3. COMPENSATION PROVIDER .......................................................................................................................... 27 EXHIBIT 4. COMPENSATION OBSTETRICAL.……………………………………………………………………………….…. 33 EXHIBIT 4A. RADIOLOGY PROCEDURES .. …………………………………………………………………………….……….. 39 EXHIBIT 5. PROVIDER DISCLOURES…... ……………………………………………………………………………………….. 40 EXHIBIT 6. ADDENDUM……………………………………………………………………………………………………………….41 UNIVERSITY PHYISICANS HEALTHCARE dba THE UNIVERSITY OF ARIZONA HEALTH PLANS PROVIDER SERVICE AGREEMENT This Services Agreement (the Agreement) is entered into effective _____TBD__________ (“Effective Date”), between University Physicians Healthcare dba The University of Arizona Health Plans, an Arizona non-profit corporation, including University Family Care, University Care Advantage and University Healthcare Group, (collectively “UAHP) and Yavapai County Community Health Services (Provider). The Addendum at Exhibit 6 (“Addendum”) is incorporated into this Agreement and is binding on the parties. In the event of inconsistent language between the Addendum and any other provision of this Agreement, the language in the Addendum shall control. RECITALS A. UAHP has entered into contracts with the Arizona Health Care Cost Containment System (AHCCCS) to offer various products such as KidsCare and other like products of the AHCCCS program. B. UAHP has entered into a contract with the Centers for Medicare and Medicaid Services (“CMS”) to provide services to Medicare beneficiaries who elect Membership in a health plan through the Member Medicare Advantage Program. C. UAHP has entered into contracts with Healthcare Group of Arizona (HCG) to offer affordable health insurance for the self-employed, Arizona companies with fewer than 50 employees, and political subdivisions. D. UAHP will provide services under the products of University Family Care (UFC) (an AHCCCS managed care plan), KidsCare (an AHCCCS managed care plan), University Care Advantage (UCA) (a Medicare Advantage Plan) and University Healthcare Group (UHCG) (administered under Healthcare Group of Arizona), and any other like products offered by The University of Arizona Health Plans, AHCCCS, Healthcare Group of Arizona and Medicare Advantage Program.. E. Provider is licensed and/or certified to provide health care items and/or services in Arizona. F. UAHP wishes to contract with Provider as a subcontractor to provide certain covered medical and related services to eligible UAHP Members. AGREEMENT The parties hereby agree as follows: 1. DEFINITIONS The following terms shall have the meanings set forth below unless the context otherwise requires. All non-defined terms shall have the meanings established by AHCCCS or CMS rules and regulations. Adverse Action/Decision Any action, such as a denial of Prior Authorization, for which a Member may file an Appeal and subsequently a request for hearing if necessary, or an action such as denial of claim or authorization from which a Provider may file a Grievance. Administration representatives. The Arizona Health Care Cost Containment System Administration and its official designees or Advance Directive A written document or instruction, such as a living will or health care proxy, made in advance of an incapacitating illness that states Member's treatment decisions, or identifies the person to make such treatment decisions if Member is unable to make it. AHCCCS The Arizona Health Care Cost Containment System, as authorized by A.R.S. § 36-2901 et seq., which is composed of the Health Administration, contractors, and other arrangement through which health care services are provided to a Member. Ancillary Care All health care services other than Physician and Hospital inpatient and Outpatient Services which are within the scope of services offered by UAHP and are ordered or approved by a Physician, including, but not limited to, xray, laboratory, ambulance, durable medical equipment, home health, vision services, Medically Necessary transportation, and pharmacy services. Appeal A disagreement by a Member with a UAHP Adverse Action/Decision such as denial of authorization. A Member may request a hearing if dissatisfied with the UAHP’s decision on the Appeal. Capitation Payment A predetermined periodic payment made to Provider by UAHP for providing Covered Services based on the number of assigned Members. Clean Claim A claim that can be processed without obtaining additional information from the Provider of the service or from a third party. It does not include a claim from a Provider who is under investigation for fraud or abuse, or a claim under review for medical necessity. In the context of billing for services provided to a beneficiary of a Medicare Advantage Plan, a Medicare Prescription Drug Plan and all types of Medicare Advantage Special Needs Plans, “Clean Claim” shall have the meaning applicable under Part C or Part D of Title XVIII of the Social Security Act. CMS The Center for Medicare and Medicaid Services. Coinsurance A percentage that the Member pays after the UAHP's Deductible has been exceeded. Complainant A Provider or Member exercises their rights to file a Grievance, Appeal, or Request for Hearing regarding a denial or Adverse Action/Decision issued by the UAHP. Co-payment An amount specified by the Director that a Member pays directly to a contractor or Provider at the time Covered Services are rendered. Covered Services The specific medical and surgical services in Provider’s area of specialty as designated in Exhibit 1 provided by Provider, and for which the Provider assumes responsibility and agrees to provide to or obtain for Members. Cultural Competency The integrated pattern of human behavior that includes thought, communication, actions, customs, beliefs, values and institutions of a racial, ethnic, religious or social group. Culture defines the preferred ways for meeting needs and may be influenced by factors such as geographic location, lifestyle and age. Deductible The portion of healthcare expense the Member must pay before the UAHP's benefits begin as applicable to each product line indicated in Recitals. EPSDT Early and Periodic Screening, Diagnosis, and Treatment services are for persons under 21 years of age. EPSDT services are synonymous with “well-check” services provided to patients as described in the Arizona Administrative Code R9-22, Article 2. Emergency Medical Services Services provided after the sudden onset of a medical condition manifesting itself by acute symptoms of sufficient severity (including severe pain) such that the absence of immediate medical attention could be expected to result in placing the patient’s health in serious jeopardy, serious impairment of bodily functions, or serious dysfunction of any bodily organ or part. In the context of billing for services provided to a beneficiary of a Medicare Advantage Program, a Medicare Prescription Drug Plan and all types of Medicare Advantage Special Needs Plans, “Emergency Medical Services” shall have the meaning applicable under Part C or Part D of Title XVIII of the Social Security Act. Encounter A record of medical services submitted by a contractor, which is rendered by a Provider to a Member who is enrolled with the contractor on the date of service for which the contractor incurs any financial liability. Fee-For-Service Payment A method of retrospective payment to subcontractors by UAHP for certain Covered Services based on a fee-for-service schedule. Grievance For a Member is a complaint that initiates the UAHP administrative review on behalf of the Member. For a Provider is a complaint that initiates the UAHP administrative review on half of the Provider which a Provider may Appeal and request a hearing. Health Administration The Arizona Health Care Cost Containment System Administration. Healthcare Group of Arizona (HCG) The registered name of the Healthcare Group Program which is a prepaid medical coverage product marketed by the Healthcare Group Program to small uninsured businesses and political subdivisions within the State. Inpatient Services Covered Services provided to Members admitted to a Participating Hospital. KidsCare (including KidsCare II) A program implemented by AHCCCS under Title XXI--Children’s Health Insurance Program--to provide health care coverage statewide to eligible children under age 19 provided through existing AHCCCS health plans. Locum Tenens A credentialed Provider, not necessarily contracted with the UAHP, but who is approved to cover Members in the absence of the Member’s Provider. Medical Director A Physician licensed in Arizona appointed by UAHP to manage the Administration of Covered Services, Utilization Management and Quality Management and other matters relating to the provision of services to Members. Medically Necessary A Covered Service provided by the Physician or other licensed medical practitioner of the healing arts and within the scope of practice under state law to prevent disease, disability, and other adverse health conditions or their progression or prolong life. In the context of billing for services provided to a beneficiary of a Medicare Advantage Plan, a Medicare Prescription Drug Plan and all types of Medicare Advantage Special Needs Plans, “Medically Necessary” shall have the meaning applicable under Part C or Part D of Title XVIII of the Social Security Act. Medicare Advantage Program Social Security Act. Medicare Advantage Beneficiary Advantage contract. The Medicare managed care program authorized under Title XVIII, Part C, of the A person eligible for, and enrolled under, a Benefit plan pursuant to a Medicare Medicare Advantage Organization An organization that has entered into an agreement with CMS under the authority of Title XVIII, Part C, of the Social Security Act and that has delegated certain responsibilities under that contract to UAHP. Medicare Advantage Special Needs Plan A Medicare Advantage plan under which only Medicare Beneficiaries who are also eligible for Medical Assistance under Title XIX are eligible to enroll, as defined in Section 1859(b)(6)(A) of the Social Security Act. Member Eligible person enrolled with UAHP, and assigned to receive Covered Services from Providers pursuant to this Agreement. Nurse Practitioner Outpatient Services A Nurse Practitioner that is licensed under A.R.S. § 32-1601 et seq. A service provided in an outpatient setting that does not result in an admission. Participating Health Professional (PHP) A Physician, physician assistant, Nurse Practitioner, and other professional: (a) who is employed by, contracted with, associated with or otherwise represented by Provider and is identified in Exhibit 1 to this Agreement (b) who is authorized by Provider to provide Medically Necessary Covered Services pursuant to this Agreement (c) who has been offered and completed all UAHP application and credentialling requirements and has been approved by the UAHP for participation under this agreement; and (d) who agrees to comply with all requirements and provisions of this Agreement. Participating Hospital A health care institution (a) licensed by the Department of Health Services pursuant to A.R.S. Title 36, Chapter 4, Article 2 as a Hospital; (b) certified as a Provider under Title XVIII of the Social Security Act, as amended, or is currently determined by CMS to meet the requirements of such certification; (c) holding a current Certificate of Accreditation from the Joint Commission ("JCAHO"); and (d) holding a contract with UAHP, or otherwise approved by UAHP, to participate in the UAHP Provider network to provide Covered Services. If Provider is a Hospital, than it is a Participating Hospital pursuant to this Agreement. Participating Provider Any person/organization who contracts with UAHP for the provision of hospitalization and medical care to Members (i.e., specialty care Providers, hospitals, outpatient facilities, DME, etc.). Physician Any M.D. or D.O. licensed in the state of Arizona under A.R.S. § 32-1401 et seq. or A.R.S. § 32-1800 et seq. Plan(s) The product offered by UAHP and through which Provider provides Member’s with services under this Agreement. As referred to in this Agreement, Plan(s) includes only those identified in the Provider Participation Schedule at Exhibit 1. Primary Care Provider (PCP) A Physician who is a Family Practitioner, General Practitioner, Pediatrician, General Internist or Obstetrician or Gynecologist with an assigned panel of Members. Primary Care Provider may also include a Nurse Practitioner with an assigned panel of Members. Prior Authorization The process by which UAHP, according to its Utilization Management Policies and Procedures, authorizes, in advance, the delivery of Covered Services contingent on their medical necessity. Prior Authorization does not guarantee payment. Provider The person/organization contracting with the UAHP to provide healthcare services to UAHP Members in accordance with this Agreement. Provider includes all PHP’s. Provider Manual The manual that contains the policies and procedures, and operating guidelines instituted by UAHP for the use in providing services to UAHP Members. Quality Management The methodology and activity used by professional health personnel through a formal program involving multiple organizations components and committees to assess the degree of conformance to desired medical standards and practices and improve or maintain quality service and care. Referral The process by which a Member is directed by a Primary Care Provider or an attending Physician to another appropriate Provider or resource for diagnosis or treatment. Replacement PHP A credentialed Participating Health Professional (PHP), not necessarily contracted with the UAHP, but who is approved to cover Members in the absence of the Member’s Provider. Request for State Fair Hearing The review process through Administration that occurs upon written request by a Complainant dissatisfied with the UAHP’s decision/resolution to a filed Provider Grievance or Member Appeal. Retrospective Review Retrospective Review is the process of determining coverage for a clinical service by applying guidelines/criteria to support claims adjudication after the opportunity for precertification or concurrent review has passed. Specialty Care Obstetrician (SCO) A Physician, SCP, Nurse Practitioner, or certified nurse wife practicing in the field of obstetrics/gynecology who assumes primary responsibility for supervising, coordinating and providing Medically Necessary Covered Services relating to initial, antepartum, delivery and postpartum care to Members and for maintaining continuity of care with Member’s PCP. Specialty Care Physician (SCP) A qualified Physician who practices a specific medical or surgical specialty and who contracts with UAHP to accept Referrals from PCPs for the purpose of providing Medically Necessary Covered Services in that specialty to Members. Usual, Reasonable, and Customary The usual charge made by a Physician or supplier of services, medicine, or supplies. This fee will not exceed the general level of charge determined by others rendering or furnishing such services, medicines, or supplies within an area in which the charge is incurred for sickness or injuries comparable in severity and nature to the sickness or injury being treated. The term “area” as it would apply to any particular service, medicine, or supply means a county or such greater areas as is necessary to obtain a representative cross section of level of charges. Utilization Management A methodology used by professional health personnel that assesses the medical indications, appropriateness, and efficiency of care provided. 2. RIGHTS, RESPONSIBILITIES AND OBLIGATIONS OF PROVIDER 2.1. Services. Provider and its employees, agents and subcontractors (collectively “Provider”, except where noted) agree to participate in the Plans listed in Exhibit 1, and other Plans as UAHP may designate in writing from time to time. Provider shall provide, arrange for and coordinate all Medically Necessary Covered Services for Members of those Plans in accordance with the provisions of this Agreement, the Provider Manual and as directed by UAHP. All services shall be provided in accordance with nationally recognized clinical protocols and guidelines when available, and generally applicable standards for the provision of medical services. Provider shall ensure that all PHPs, employees, agents or subcontractors providing services under this Agreement comply with the terms, conditions and requirements of this Agreement and the terms, conditions and requirements of this Agreement shall be binding on Provider and its PHPs, employees, agents and subcontractors. Provider represents and warrants that it has the authority to bind all PHPs, employees, agents and subcontractors to comply with the terms of this Agreement. Provider shall deliver contracted services, as appropriate, to Members within 24-hours of discharge from an acute setting, or later if so prescribed. Provider understands that nothing in this Agreement prohibits or restricts Provider, or Provider’s PHPs, employees or contractors, acting within the scope of their practice, from communicating freely with Members regarding their health care, medical status, treatment options, the risks, benefits and consequences of treatment and non-treatment, the opportunity to refuse treatment and to express preferences about future treatment decisions, even if needed services are not Covered Services. 2.2. Capacity and Appointment Availability. Provider shall provide Medically Necessary Covered Services to Members through office visits during regular office hours, after hour office visits, skilled nursing facility visits, home visits or other appropriate non-office visits such as emergency and Inpatient Services. To ensure that Provider can provide continued high quality care and adequate access to Members, Provider agrees to maintain the capacity and appointment availability requirements applicable to Provider’s medical specialty/Provider-type set forth in the UAHP Provider Manual, by the Administration and/or CMS or such subsequent requirements adopted by UAHP. Provider must have the ability to provide Emergency Medical Services 24 hours a day, seven (7) days a week, including holidays. Should UAHP determine that Provider’s capacity and appointment availability are non-compliant with UAHP, AHCCCS or CMS requirements; Provider will immediately implement a corrective action plan to return to compliance. Failure to maintain adequate capacity and/or appointment availability is grounds for termination of this Agreement. 2.3. Equal Access to Services. Provider shall provide Medically Necessary Covered Services to Members with the same professional standards of care, skill and diligence customarily used by similar Providers in the community in which such services are rendered, and shall render Medically Necessary Covered Services to Members in the same manner, in accordance with the same standards and with the same availability as offered to other patients and to other Members regardless of eligibility category. Members are entitled to exercise their rights and shall not have their treatment adversely affected by Provider as a result. In addition, Provider shall provide Covered Services to Members without regard to payer source, race, color, creed, gender, religion, age, national origin (to include those with limited English proficiency), ancestry, marital status, sexual preference, genetic information, medical history, claims experience, medical condition, receipt of health care, evidence of insurability (including conditions arising out of acts of domestic violence) or physical or intellectual disability, except where medically indicated. Provider shall comply with Title VI of the Civil Rights Act of 1964, which prohibits the denial of benefits of or participation in Covered Services on the basis of race, color or national origin; the requirement of Section 504 of the Rehabilitation Act of 1973, as amended, which prohibits discrimination on the basis of handicap in delivering Covered Services; the Age Discrimination Act of 1975, which prohibits discrimination on the basis of age; and Title IX of the Education Amendments of 1972, which prohibits discrimination based on sex. 2.4. Provider. Provider shall list all persons providing Services under this Agreement on Exhibit 1, which list shall be subject to UAHP’s approval. Provider must request in writing to add to or delete from this list at least ninety (90) days prior to desired effective date, and all additions are subject to UAHP approval. In the event Provider arranges for back up or temporary replacement coverage by a Locum Tenens, or Replacement PHP, Provider shall obtain Prior Authorization from UAHP for such Replacement PHP or Locum Tenens. Replacement PHP and Locum Tenens shall provide the Covered Services subject to the terms of this Agreement, including but not limited to requirements for Prior Authorization. UAHP retains the right to approve, suspend or terminate any arrangement between Provider and a PHP or its subcontractors to provide services to AHCCCS enrollees or Medicare Advantage Beneficiaries. 2.4.1. Licensure and Credentialing. Provider shall comply with NCQA standards and procedures regarding the credentialing and approval of Provider and its PHPs, employees and subcontractors for participation under this Agreement. Provider shall comply with, and shall ensure that all PHP, employees and/or subcontractors maintain the applicable state license or certification necessary to provide Covered Services and comply with all Federal and State laws and regulations regarding licensure, Medicare and AHCCCS certification and Drug Enforcement Administration registration. Provider, and any PHP, subcontractor, employee or agent performing services under this Agreement must be, as applicable, an AHCCCS Provider in good standing and/or certified by CMS. In addition, Provider, any PHP, subcontractor, employee or agent may not be excluded or suspended from participation in any government program, including Medicare, Medicaid or CHIP. Provider shall screen its PHPs, employees and subcontractors by searching the HHS-OIG website to ensure compliance with this provision. Provider shall give immediate written notice to UAHP if its license or ability to participate in AHCCCS or Medicare is lost, suspended or limited in any way that affects Provider’s or a PHP’s, employee’s, subcontractor’s or agent’s ability to provide services under this Agreement. Provider shall furnish to UAHP such evidence of licensure, registration and certification upon request. If Provider is licensed, certified or accredited by an agency, such as the Occupational Safety and Health Administration (OSHA) or Clinical Laboratory Improvement Act (CLIA), Joint Commission (JC), National Committee on Quality Assurance (NCQA) or AAHC, Provider shall furnish such evidence of licensure, certification or accreditation to UAHP. Provider shall give immediate written notice to UAHP if such license, certificate or accreditation is lost, suspended or limited in any way. 2.4.2. Provider Representation and Warranties; Termination. Provider represents and warrants that it and each individual or entity providing services under this Agreement: (i) is appropriately licensed and/or certified to provide the Covered Services; (ii) is a registered AHCCCS Provider and certified by CMS and in good standing with both agencies; (ii) will provide the Covered Services within the scope of the Provider’s license or certification; (iii) maintains the applicable and appropriate facility and/or equipment licenses necessary to provide the Covered Services; and (iv) has never been: (1) excluded, debarred, or suspended from participation in any federal or state government health care program, including Medicare, Medicaid, or CHIP; or (2) convicted of or indicted on a felony or a crime relating to health care. Provider further represents and warrants that Provider has no director, officer, partner or owner of 5% or more of the Provider entity, any person, or affiliate of such a person, that is debarred, suspended or otherwise excluded from federal procurement activity. Provider agrees to notify UAHP in the event the foregoing representations and warranties are no longer true. Such notice shall contain information sufficient to allow UAHP to determine the nature of any sanction, indictment or conviction. If it is determined that the representations and warranties of this Section 2.4.2. are no longer true or if Provider breaches this Section 2.4.2., UAHP may, at its option, immediately terminate this Agreement. Provider shall exclude from providing services under this Agreement any individual who is excluded or suspended from participation in a state or federal health care program. 2.4.3. Disclosure on Ownership Information and Control. (42 CFR 455.104). Provider has fully and accurately disclosed on Exhibit 6 all of the information required under 42 C.F.R. § 455.104 for any individual or corporation with an ownership or controlling interest in Provider. Provider shall promptly notify UAHP of any deletions, additions or amendments to the information on Exhibit 6, but in no event no later than 35 days after any change. 2.5. Compliance with Laws, Rules; Policies and Procedures. 2.5.1. Laws, Rules and Regulations. Provider shall comply with, and require that each individual or entity with whom it contracts to provide services under this Agreement comply with, all Federal, State and local laws, regulations, standards, local coverage determinations, and executive orders governing performance of duties under this Agreement, including, but not limited to, all provisions relating to Provider participation in Medicare and AHCCCS. The Provider shall comply with all Federal, State and local immigration laws and regulations relating to the immigration status of their employees during the term of the contract. Further, the Provider shall flow down this requirement to all PHPs and subcontractors. The State shall retain the right to perform random audits of UAHP and Provider records or to inspect papers of any employee thereof to ensure compliance. Provider shall comply with Federal regulations of the Occupational Safety and Health Administration including, without limitation, the regulations concerning Bloodborne Pathogens Standards at 29 C.F.R. Part 1910.1030, as amended. Provider shall ensure that all handicapped persons have access to Provider facilities as required by applicable Federal, state and local law. Provider will appropriately report all incidents of suspected child and vulnerable adult abuse to proper authorities in accordance with A.R.S. § 13-3620 and A.R.S. § 46-454 and to UAHP. Provider will comply with all of the AHCCCS Standard Subcontract Terms and Conditions as defined by AHCCCS set forth in the UAHP Provider Manual. Provider also agrees to comply with all Federal, State and local laws and regulations designed to ameliorate fraud, waste and abuse, including applicable provisions of federal criminal law and federal and state laws governing kickbacks and the Physician Self-Referral Law, 42 U.S.C. § 1395nn and provisions for Physician incentive arrangements pursuant to 42 U.S.C. § 1395mm(i) and related regulations. Provider must train its staff on the following aspects of the Federal False Claims Act (31 USC § 3729 et seq.): (a) (b) (c) The administrative remedies for false claims and Statements; Any State laws relating to civil or criminal penalties for false claims and Statements; The whistleblower protections under such laws. Provider will notify UAHP of any Member activity that causes suspicion of fraud against any Plan. In the event AHCCCS, CMS or any other agency with authority over UAHP or any Plan imposes sanctions or penalties upon UAHP or any Plan due to Provider’s non-compliance with UAHP, AHCCCS, CMS or other applicable statutes, regulations, instructions, guidance, performance standards, polices, or procedures, Provider shall either reimburse UAHP or UAHP shall deduct the amount of the penalty or sanction from future payments to Provider, at the sole discretion of UAHP. 2.5.2. Non-Discrimination in Employment. Provider shall comply with Title VII of the Civil Rights Act of 1964, as amended, the Age Discrimination In Employment Act, State Executive Order 75-5 and Federal Executive Order 11246 which mandates that all persons, regardless of race, color, religion, sex, age, national origin or political affiliation, shall have equal access to employment opportunities. If applicable, Provider shall comply with Section 503 of the Rehabilitation Act of 1973, as amended which prohibits discrimination in the employment or advancement of the employment of qualified persons because of physical or mental disability. 2.5.3. UAHP Policies and Procedures. In providing services under this Agreement, Provider must comply with all applicable UAHP policies and procedures and all guidance issued by UAHP, including the Provider Manual. UAHP policies and the UAHP Provider Manual are available on UAHP’s website (http://ufcaz.com/ProviderResourcePage.aspx) and may be updated from time to time. Provider is responsible for keeping current with UAHP’s policies and maintaining compliance. 2.5.4. Noncompliance. Should AHCCCS, CMS or UAHP determine that the Provider and/or any PHP is noncompliant with this Agreement, AHCCCS, CMS or UAHP may pursue all remedies allowed by law, including, but not limited to, suspension of work, termination of the contract for default and suspension and/or debarment of the Provider. 2.6. Facilities. 2.6.1. Provider Facility Locations. Provider shall provide Medically Necessary Covered Services at locations approved by UAHP. The current approved locations are listed on Exhibit 1. Provider shall not eliminate or change a location without sixty (60) days advance written notice to UAHP and any affected Member. 2.6.2. Management and Services Responsibilities. The operation and maintenance of the offices, facilities and equipment of Provider and the provision of all Covered Services, shall be solely and exclusively under the professional control and supervision of Provider. Except as set forth in Section 2.4, UAHP shall have no right of control over the selection of support staff, the supervision of personnel, or the financial operation of Provider’s practice. Nothing contained in this Agreement shall be construed as giving UAHP any right to manage or conduct the practice of Provider as manager, proprietor, lesser or otherwise. The Provider is required to meet all AHCCCS, CMS and UAHP requirements for facilities and Member services. 2.6.3. Facility Inspection. Provider shall allow UAHP or its agents to inspect Provider premises and operations upon reasonable notice and during regular office hours to ensure that such premises and operations are adequate to meet Member's needs. The facility will be inspected prior to the Provider beginning to see patients. 2.7. Referrals and Authorization for Services. 2.7.1. Prior Authorization. Except for Emergency Medical Services, Provider shall obtain Prior Authorization from the applicable Plan for any Fee-For-Service Medically Necessary Covered Service to the Member in accordance with Plan policies. Failure to follow the Prior Authorization/Notification process may result in denial of payment. Prior Authorization is not a guarantee of payment. 2.7.2. Referrals. Provider shall obtain Prior Authorization for specified procedures and shall complete Referral forms for Covered Services to be referred to a Physician other than Members’ assigned PCP. Except for Emergency Medical Services, or as otherwise authorized by the Medical Director (or designee) or required by AHCCCS or CMS, all Referrals shall be to Participating Providers. Provider shall refer to and comply with UAHP’s Referral policies and procedures as set forth in the Provider Manual. A SCP shall not begin a course of treatment for a medical condition other than that for which the Member was referred, unless approved by the Member’s PCP. 2.7.3. Direct Access to Services. Provider agrees that, notwithstanding the terms of the Agreement, Members shall have direct access to women’s health specialists within the network for women’s routine and preventive health care services that are Covered Services. In addition, Medicare Advantage Beneficiaries shall have direct access to screening mammography and influenza vaccines that are Covered Services and are furnished by a Participating Provider. Direct access to specialists must also be available for Members with special health care needs determined through an assessment by appropriate health care professionals (42 C.F.R. § 438.208(c)(2)) to need a course of treatment or regular monitoring. 2.7.4. Obstetrical Care. If Provider is not contracted to provide obstetrical care, Provider shall refer pregnant Members to a participating SCO who is able to provide initial prenatal care consistent with the appointment standards set forth in this Agreement and the Provider Manual. 2.7.5. Referrals to RHBA, CRS and IHS. Provider must comply with all applicable statutes, rules, policies and procedures governing the required referral and linkage systems for behavioral health to the responsible Regional Behavioral Health Authority (RHBA), Arizona Children’s Rehabilitation Services (CRS), and Indian Health Services. If a Member’s medical condition is eligible for coverage by CRS, Provider agrees to submit referrals for those Members to CRS and seek payment from CRS prior to seeking payment from UAHP. 2.7.6. Formulary. Provider shall prescribe generic medications and medications listed in UAHP’s formulary in accordance with UAHP policies. If not available or listed in the formulary, Provider shall obtain approval before prescribing medications in accordance with UAHP’s Prior Authorization policies. Provider understands not all medications are covered by all Plans. 2.8. Staff Membership at Participating Hospitals. Provider shall maintain staff Membership and admission privileges in good standing with at least one of the Plan’s Participating Hospitals; or have a hospitalists agreement with at least one of the Plan’s Participating Hospitals, or as otherwise permitted by Plan. Provider shall admit Members only to Participating Hospitals except (a) as otherwise approved by Plan; (b) if Emergency Medical Services are required; (c) as otherwise described in the Provider Reference Manual; or (d) as otherwise required by law or AHCCCS regulation. 2.9. Orientation. Provider or designee shall attend a UAHP orientation within a reasonable time after the Effective Date. In addition the Provider or designee is required to attend one (1) Provider update meeting per year with the UAHP Medical Director. If the Provider chooses to send a designee, the Provider is responsible for all information disseminated, written or oral, at the orientation and Provider update meetings. 2.10. Utilization Management. Provider shall comply with and cooperate in UAHP's Utilization Management review activities as set forth in Section 4.7. UAHP may conduct medical and utilization review of claims submitted by Provider to ascertain Medical Necessity and appropriateness of costs. Provider shall designate appropriate personnel to facilitate UAHP's Utilization Management reviews (including Prior Authorization, concurrent and Retrospective Review) and Quality Management. Provider shall provide UAHP with timely access to Member's medical records to facilitate Utilization Management review and Quality Management. Provider shall compile and provide utilization and quality review information to UAHP, subject to applicable laws, in a manner intended to assess and enhance performance with regard to quality of care, quality of service and cost effectiveness as required by UAHP and AHCCCS or CMS. Compensation to individuals or entities that conduct utilization management and concurrent review activities is not structured to provide incentives for the individual or entity to deny, limit, or discontinue Medically Necessary services to any enrollee (42 CFR 438.210(e)). 2.11. Quality Management Compliance. Provider shall comply and cooperate with the UAHP Quality Management program and other programs as may be adopted by UAHP, and the National Committee for Quality Assurance (NCQA), or required by regulatory agencies such as AHCCCS or CMS. Provider shall allow UAHP or its agents to conduct periodic audits and site surveys upon reasonable notice and during regular office hours for the purpose of evaluating compliance with Quality Management standard. The Quality Management program and Utilization Management program shall not be construed to interfere with or in any way affect Provider's obligation to exercise independent medical judgment in rendering Covered Services to Members. 2.12. Provider Preventable Condition. Provider must identify and report to UAHP any Providerpreventable condition as required by Section 2702 of the Affordable Care Act. Reports shall be timely made and in accordance with federal and state requirements. Provider acknowledges that federal law prohibits payment for those Provider-preventable conditions identified by AHCCCS or Medicare. 2.13. Advance Directives. All Providers shall comply with all Federal and State law relating to Advance Directives. Provider shall: (a) Maintain written policies that address the rights of adult Members to make decisions about medical care, including the right to accept or reject medical care, and the right to execute an Advance Directive. If the Provider has a conscientious objection to carrying out an Advance Directive, it must be explained in the policies. (b) Provide written information to adult Members regarding an individual’s right under state law to make decisions about medical care, and the Provider’s written policies concerning Advance Directives (including any conscientious objections). (c) Document in the Member’s medical record whether or not the adult Member has been provided the information and whether an Advance Directive has been executed. (d) Not discriminate against a Member because of his or her decision to execute or not to execute an Advance Directive, and not make it a condition for the provision of care. (e) Provide education to staff on issues concerning Advance Directives including notification of direct care Providers of services, such as home health care and personal care, of any Advance Directives executed by Members to whom they are assigned to provide services. 2.14. Complaint, Inquiry, Investigation or Review. Provider shall notify UAHP immediately of the initiation of any lawsuit, complaint, inquiry, investigation, review or action by any licensing or regulatory authority, organization or body which directly or indirectly evaluates or focuses on the quality of care provided by Provider or any PHP either in any specific instance or in general, or which may, if sustained, materially impede Provider’s ability to meet its duties and obligations under this Agreement. 2.15. Member Information. All information about and concerning Members, including their names and addresses (Information) are considered confidential and proprietary to UAHP. Except as otherwise required by Section 5, as is Medically Necessary or as required by the Physician-patient relationship, Provider shall not use any Information or contact Members without the advance written consent of UAHP. Changes in practice (location, PHP termination with Provider, etc.) must all be communicated to the Member by UAHP. The provisions of this section shall survive the termination of this Agreement. Nothing in this Section shall be construed to limit communications between Provider and Members necessary for the provision of Covered Services 2.16. Data Exchange Requirement. Provider shall meet any AHCCCS, CMS or UAHP required technical and procedural requirements for data exchange interfaces between or among AHCCCS, UAHP and Provider. Provider shall comply with any technical requirements as mandated by AHCCCS, CMS or UAHP from time to time. Provider shall implement any applicable ANSI electronic data interchange (EDI) standards required by AHCCCS, CMS or UAHP. 2.17. Member Rights. Provider recognizes the right of Members to be treated with respect and with due consideration for the Member’s dignity and privacy, to receive information on available options and alternatives, presented in manner appropriate to the Member’s condition and ability to understand and to participate in decisions regarding the Member’s health care, including the right to refuse treatment. All Providers must offer high quality services in a culturally competent manner. In providing this care, the Provider must be aware of and sensitive to the patient’s cultural needs. Factors that influence culture include but are not limited to: race, ethnicity, where one was raised, language, reading skills, age, gender, socioeconomic status, religion, values and beliefs, family structure, sexual orientation, homelessness, physical and mental ability. Members have the right to be free from any form of restraint or seclusion used as a means of coercion, discipline, convenience or retaliation, as specified in federal and state law on the use of restraints and seclusion. Provider must comply with UAHP’s policies and procedures concerning Member rights as set forth in the Provider Manual. Provider shall participate in and comply with the performance standards, policies, procedures, and programs established from time to time by UAHP, AHCCCS or CMS with respect to cultural and linguistic services, including without limitation, attending training programs, and collecting and furnishing cultural and linguistic data to UAHP, AHCCCS and CMS. 2.18. Interpretation Services. The UAHP, in conjunction with the Provider, shall provide interpretive services to those Members needing such services. If the Provider is aware that a Member is in need of interpretive services, the Provider shall assist the Member in contacting the UAHP to arrange for these services. 2.19. EPSDT. Providers serving EPSDT-aged Members must utilize the AHCCCS-approved EPSDT tracking forms and standardized developmental screening tools. Provider also agrees to fill out EPSDT tracking forms for pregnant Members under 21 years of age as they qualify for EPSDT services and return to UAHP. UAHP uses the information to track and trend service needs of this population. 2.20. Vaccines for Children (VFC) Program. The vaccine portion of childhood immunizations shall be reimbursed through the State of Arizona’s VFC Program. It is the responsibility of Provider to submit billings to the VFC Program for reimbursement. UAHP will not reimburse Provider for the Administration of the vaccines in excess of the maximum allowable cost set by CMS. 2.21. Information About the Plan. Provider may provide a Member with factual information regarding the Plans, but is prohibited from recommending or persuading a Member’s selection of any Plan. 3. DELEGATION 3.1. Services. Provider acknowledges that UAHP has delegated to Provider certain responsibility under its Medicare Advantage and AHCCCS contracts to provide those Medicare and Medicaid Covered Services within the scope of Provider’s and PHPs’ licensure or certification and expertise to Medicare Advantage Beneficiaries and AHCCCS Members, including, to the extent applicable, certain limited Medicare Part D items or services. Provider agrees that UAHP may only delegate such responsibilities in a manner consistent with the applicable standards set forth under 42 CFR §422.504 (i), 42 CFR §423.505(i), and 42 CFR §438.230(b). Provider further agrees that UAHP may revoke this delegation and thereby terminate this Agreement if Provider does not perform satisfactorily and if any of Provider’s reporting and disclosure obligations is not fully met in a timely manner. Provider agrees to implement corrective action upon request if UAHP identifies deficiencies or areas for improvement. 3.2. Monitoring. Provider acknowledges that UAHP shall oversee and monitor Provider’s performance on an ongoing basis. Provider further acknowledges that UAHP is accountable to CMS for the functions and responsibilities described in the Medicare Advantage contract and regulatory standards and to AHCCCS for the functions and responsibility described in the Medicaid agreements and regulatory standards. 3.3. Compliance with Laws. Provider agrees to comply, and to require any and all of its subcontractors and employees to comply, with all applicable Medicare and Medicaid laws, regulations, and CMS or AHCCCS instructions. Further, Provider agrees that any services provided by Provider, it’s PHPs, employees or its subcontractors to UAHP, any Medicare Advantage Beneficiary or AHCCCS Member will be consistent with, and will comply with, as applicable, UAHP’s contractual obligations to CMS and AHCCCS. 3.3.1. Responsibility for Credentialing. Provider shall credential any and all of its subcontractors on behalf of UAHP. Provider agrees to comply with all aspects of UAHP’s credentialing and re-credentialing policies and procedures. Provider agrees that the credentialing process will be reviewed and approved by UAHP and that UAHP will audit the credentialing process on an ongoing basis. 4. RIGHTS, RESPONSIBILITIES AND OBLIGATIONS OF UAHP 4.1. Administration. UAHP agrees to administer the provisions of this Agreement according to AHCCCS and CMS requirements. This includes Prior Authorization, Utilization Management, Quality Management, Member Services, Provider Services, fiscal services, claims processing and information reporting. 4.2. Member Eligibility Verification. UAHP shall maintain a 24-hour per day, seven day a week telephone or on-line service to assist Provider in verifying the eligibility of a Member. 4.3. Orientation, Education and Communication. UAHP will assign a Provider representative to provide initial orientation, ongoing education and operational assistance to Provider regarding participation with UAHP. 4.4. Policies and Procedures. UAHP shall develop and maintain policies and procedures and shall make copies of these policies, procedures and the Provider Manual available to Provider. During the term of this Agreement, UAHP shall notify Provider of any modifications to the policies and procedures. 4.5. Compensation for Provider. UAHP shall compensate Provider for Medically Necessary Covered Services delivered under this Agreement as set forth in Section 5. Provider shall accept the compensation set forth in Section 5 of this Agreement, including the coordination of benefits provisions, less applicable Coinsurance, Copayments, and/or Deductibles, as payment in full for all Covered Services provided by Provider to Members pursuant to this Agreement. UAHP shall have no obligation or responsibility to make any compensation directly to any PHP. 4.6. Utilization Information. UAHP will compile and provide utilization review information to Provider in a manner intended to assess and enhance performance with regard to quality of care, quality of service and cost effectiveness. 4.7. Utilization Management. UAHP or its designee shall perform Utilization Management services, including but not limited to Selective Prospective Review, Inpatient or Outpatient Case Management, or Retrospective Review. 4.8. Selective Prospective Review. Through its Prior Authorization process, UAHP shall confirm Member’s eligibility and that proposed services are Medically Necessary Covered Services and are provided at the most appropriate level of care and site. 4.9. Inpatient Case Management. UAHP’s reviewers for Inpatient Services shall provide on-site or telephonic nurse reviewers for Utilization Management and discharge planning. 4.10. Outpatient Case Management. UAHP’s case reviewers for Outpatient Services shall assess, UAHP, coordinate, monitor and evaluate options and care relating to Outpatient Services to meet a Member’s health needs. 4.11. Prescription Drug Prices. UAHP will regularly update its prescription drug pricing standard consistent with the time frames set forth in 42 C.F.R. § 423.505(b)(21). These prices apply to Part D program Beneficiaries. 4.12. Participation. The participation procedures set forth in 42 C.F.R. § 422.202(a) applies to Provider’s Physicians. 5. ELIGIBILITY, CLAIMS SUBMISSION, BILLING, COMPENSATION, AND COORDINATION OF BENEFITS 5.1. Member Eligibility. 5.1.1. Member Eligibility Verification. It is Provider’s responsibility to verify the enrollment and assignment of all Members with UAHP on the date of service. As applicable, AHCCCS, HCG and CMS are responsible for enrollment, re-enrollment, and dis-enrollment of Members, respectively. Pursuant to the procedures set forth in UAHP policy, and based on eligibility lists supplied to Provider by UAHP and the eligibility verification procedure set forth in Section 4.2, Provider shall determine whether Members are eligible for Covered Services. It is Provider’s responsibility to verify the enrollment and assignment of all Members with UAHP on the date of service, and failure to do so may result in a claim being denied. Receipt of an approved referral does not verify Member’s eligibility at the time of service with the Provider. 5.1.2. Ineligible Covered Persons: Negative Retroactivity. In the event UAHP determines at any time that a Member is ineligible or terminated from coverage by AHCCCS, CMS or any Plan, Provider shall return to UAHP any fee for service payments paid by UAHP for that Member on or after the effective date of Member’s termination or eligibility. Provider may seek payment for Medically Necessary Covered Services provided to an ineligible or terminated Member after loss of eligibility or the termination date from either a new third party payer or from the individual. 5.2. Claims and Encounter Data. 5.2.1. Provider’s Submission of Claims/Encounter Data. Provider shall submit a claim for all Covered Services, whether capitated or not, per AHCCCS and CMS guidelines, as applicable, and as required by UAHP, including the Vaccine For Children Program immunizations for all Members for whom Provider receives payments. Clean Claims shall be submitted on a CMS 1500 form within ninety (90) days after the Covered Services are rendered. Claims data elements shall include, but not be limited to, the elements included in the Required Claim Information provisions of the applicable Exhibit(s) governing compensation to ensure UAHP is in compliance with all AHCCCS and CMS reporting requirements related to claims data. Claims initially received more than 90 days from the date of service will be denied. In addition, failure to submit any of the information or data required by UAHP or failure to comply with Prior Authorization/Notification requirements of this Agreement within the required time period may result in delay or denial of payment. Claims should be mailed to the Plan Claims Department at the following addresses: University Family Care PO Box 37169 Phoenix, AZ 85069-7169 University Healthcare Group PO Box 37279 Phoenix, AZ 85069-7279 University Care Advantage PO Box 38549 Phoenix, AZ 85069-8549 Provider may resubmit claims that have been denied or adjudicated by UAHP but must be received by UAHP within one hundred and twenty (120) days from the date of the initial UAHP Explanation Of Benefits (EOB). UAHP will re-adjudicate claims resubmitted by Provider only if an initial claim has been filed within the described submission deadline. Claim submissions shall be designated as such and shall consist of the following: (a). (b). (c). (d). Copy of claim; Copy of UAHP remits; Supporting documentation; and; Written explanation as to reasons for resubmission. Resubmitted claims are to be addressed and mailed to the addresses set forth in this Section. A tracer claim may be submitted in follow-up to claims that have been determined to be “not received” or “not in the system” by UAHP. Tracer claims must be received within ninety (90) days from the date of service and must be marked as “tracer” or “second submission”. Tracer claims should not be submitted less than twenty one (21) days from the first submission, allowing processing of the original claim. UAHP’s date of receipt of claims is the date the claim was received by UAHP as indicated by the date stamp on the claim and the claim reference number. Claims will be considered paid on the date indicated on disbursement checks. Denied claims will be considered adjudicated on the date of their denial. Claims that are denied and are resubmitted will receive new date stamps. Claims that are pending for additional supporting documentation from Provider will receive new date stamps upon receipt of the additional documentation except as provided under this Section 5. If the Provider does not bill UAHP (e.g., Provider is capitated), the Provider’s Encounter data that is required to be submitted to UAHP is defined for these purposes as a “claim for payment.” The Provider’s provision of any service results in a “claim for payment” regardless of whether there is any intention of payment. All said claims shall be subject to review under any and all fraud and abuse statutes, rules and regulations, including but not limited to Arizona Revised Statute (A.R.S.) §36-2918. 5.2.2. Certifications. Provider agrees to provide all information necessary for UAHP and any Plan to meet its reporting obligations under 42 C.F.R §§ 422.310 and 422.516, including, but not limited to, providing data necessary to characterize the context and purpose of each service furnished to a Medicare Advantage Beneficiary. Provider acknowledges that by submitting data to UAHP or any Plan under this Agreement, including all claims and Encounter data, the submitted data is accurate, complete, and truthful, based on the Provider’s best knowledge, information and belief. 5.2.3. Review of Claims/Encounter Data. Through Retrospective Review, UAHP will ensure that services rendered were Medically Necessary Covered Services, provided in compliance with general medical standards of care, applicable statutes, regulations, instructions, guidance, and the Provider Manual, and substantiated with documentation supporting the level of services billed. UAHP shall deny any claim not satisfying these criteria. UAHP shall conduct Retrospective Review on both a pre-payment and post-payment basis. UAHP may deduct the amount of erroneous payments from future payments to Provider or demand repayment from Provider. UAHP reserves the right to audit Provider’s billing procedures, claims and Encounter data at any time, and Provider agrees to fully cooperate and provide necessary records for such audit. Provider agrees to have procedures in place that will insure proper coding, billing, and documentation of claims and Encounter data. 5.2.4. Provider Payments. Provider shall pay on a timely basis all PHPs, employees, contractors, and agents for which Provider is financially responsible under this Agreement, included any Locum Tenens or Replacement PHP who, upon the request of Provider, provides Medically Necessary Covered Services. Payment for services provided by PHPs, employees, contractors, agents, Locum Tenens or Replacement PHPs shall be decided between Provider and individual or entity providing the service. UAHP has no obligation or responsibility to make any compensation directly to any Provider PHP, employee, contractor, agent, Locum Tenens or Replacement PHP. 5.3. Payment for Services. UAHP will reimburse Provider for the delivery of Medically Necessary AHCCCS and Medicare Part C Covered Services to Members during the term of this Agreement within forty-five (45) days receipt of a Clean Claim. Services will be compensated on a fee for service basis, if such services are Medically Necessary and Prior Authorized according to UAHP policy. Payment will be based upon the lesser of the rates set forth in the attached Exhibits, or billed charges minus any applicable Co-payments, Coinsurance, and/or Deductible. To receive payment, Provider must have a current IRS W-9 form on file with the State of Arizona and annually submit a Form IRS W-9 to UAHP. UAHP will pay Medicare Part D services in accordance with the prompt pay provisions of 42 C.F.R. § 423.520. 5.4. Risk Pool Sharing. Provider has chosen not to participate in risk pool arrangements. 5.5. Supplemental Payment Program. program. Provider has chosen not to participate in the supplemental payment 5.6. Prohibitions on Member Billing. Provider agrees that in no event, including, but not limited to, nonpayment by UAHP, UAHP’s insolvency or breach of this Agreement, shall Provider bill, charge, collect a deposit from, seek compensation, remuneration or reimbursement from, or have any recourse against a Member or persons other than UAHP acting on a Member’s behalf for Covered Services provided pursuant to this Agreement or for any fees that are the legal obligation of UAHP. This provision shall not prohibit the billing and collection of any Co-payment, Coinsurance and/or Deductible amount or any other amount in accordance with the terms of Arizona Administrative Code R9-22-702, 42 C.F.R. § 422.216, 42 CFR § 438.108 or other applicable law, as amended from time to time. However, Provider shall not hold liable Members who are beneficiaries of a Medicare Advantage Special Needs Plan for dual eligible individuals for any Medicare Part A and Part B cost sharing; Provider agrees in such cases to either accept UAHP payment as payment in full or bill AHCCCS, as applicable. Provider shall not refuse to provide Covered Services to Members who are unable to pay a Co-payment, Coinsurance, and/or Deductibles unless otherwise allowed by law. Provider further agrees that (a) this provision shall survive the termination of this Agreement regardless of the cause giving rise to termination and shall be construed to be for the benefit of the Member, and (b) this provision supersedes any oral or written contrary agreement now existing or hereafter entered into between Provider and Member or persons acting on their behalf. Non-Covered Services may be billed to an AHCCCS Member only if a waiver has been signed by the Member and all costs associated with the services have been disclosed in advance to the Member. The Member must understand that the service will not be covered by the UAHP. 5.7. Excluded Services. The Provider is not responsible for providing and UAHP is not responsible for paying costs for the Member Services set forth below: 5.7.1. No Legal Obligation. Medical Services for which neither the recipient nor any other person or organization incurs a legal obligation to pay. Such non-Covered Services may include, but are not limited to: (a) Free chest x-ray provided by voluntary health organization (b) Free samples of items received at no cost 5.7.2. Non-Covered Services. Services which are not covered by UAHP or Services AHCCCS and/or CMS, as applicable, do not cover, including but not limited to: (a) Services mandated for purposes of meeting non-medical requirements, such as employment physicals and Physician visits required for a license, certificate, or for obtaining third party liability or disability payments. (b) Services provided by or under the direction of naturopaths. (c) Personal comfort items or services. (d) Cosmetic surgery intended solely to improve the physical appearance of a recipient and which does not restore bodily function or correct a deformity. (e) Reconstructive surgical procedures intended to improve function and appearance of any body, which has been altered by disease, trauma, congenital or developmental anomalies or previous surgical processes unless the services are Covered Services that are Medically Necessary and Prior Authorized. Clear and precise documentation substantiating Medical Necessity for reconstructive surgery is required for a Covered Service determination. (f) Therapeutic legally induced abortions and abortion counseling unless the pregnancy termination is the result of rape or incest, or in circumstances where the Member suffers from a physical disorder, physical injury, or physical illness, including a life endangering physical condition caused by or arising from the pregnancy itself, that would, if certified by a Physician, place the Member in danger of death unless the pregnancy is terminated and is prior approved by the Plan. (g) Post mastectomy breast reconstruction. An initial prosthesis, including a surgical brassiere, is covered if Medically Necessary. (h) Penile implants for recipients over 21 years of age. (i) Infertility services, reversal of surgical sterilization, sex change operations. (j) Hysterectomies unless Medically Necessary. (k) Hearing aids, except as allowed under EPSDT program for recipients under 21. (l) Eye examination and eyeglasses, except as allowed under EPSDT program for recipients under 21. Glasses and contact lenses are not excluded if they are the sole prosthetic devise after cataract extraction. (m) Routine dental care, except as allowed under EPSDT program for recipients under 21. (n) Orthognathic surgery for recipients over 21 years of age. (o) Outpatient Occupational or Speech therapy except as allowed under Home Health, EPSDT, ALTCS, and KidsCare. (p) Service for items requiring Prior Authorization for which Prior Authorization has not been obtained or has been denied. (q) Services determined to be experimental or provided primarily for the purpose of research. (r) Artificial or mechanical hearts or xenografts. (s) Heart transplantation and allogeneic and autologous bone marrow transplantation, unless the recipient is categorically eligible. (t) Liver transplantation, unless the recipient is categorically eligible and under age 21. (u) Behavioral health services for non-categorically eligible acute care recipients, except for limited emergency/crisis stabilization services. (v) Behavioral health services for ALTCS recipients ages 21 through 64, except for limited emergency/crisis stabilization services. (w) Services to prison inmates or residents of a tuberculosis or Behavioral Health Treatment institution (x) Treatment for drug abuse unless authorized in rules. (y) Non-emergency transportation for KidsCare Enrollees. 5.8. Coordination of Benefits. UAHP is the payer of last resort and Provider shall identify and first bill other thirdparty carriers or insurers. If Member has third-party coverage, including, but not limited to Medicare Part A or Part B, Provider shall identify and seek such payment before submitting claims to UAHP in accordance with the following: Provider shall include a completed copy of the third-party carrier’s explanation of benefits (EOB) or remittance advice (RA) when submitting a claim for any Fee-For-Service claim balance due under non-duplication of benefits. A claim, plus a completed copy of the of the third-party carrier’s EOB or RA for any balance due, must be initially received by UAHP within sixty (60) days from the third-party carrier’s EOB or RA date. For Members with Medicare, only the difference between the Medicare allowable charges, as shown on the Explanation of Medicare Benefits (EOMB), and the Medicare reimbursement received, will be eligible for payment by UAHP. UAHP’s payment of Coinsurance plus any applicable Deductibles will constitute payment in full to Provider. For UAHP’s non-Medicare Members, the allowed amount will be based upon the UAHP Fee Schedule, less the paid amount of the other third-party carrier(s); any balance of which will be paid by UAHP as non-duplication of benefits. In the event Provider identifies any third party source of payment or liability, Provider shall immediately notify UAHP of such source. 6. RECORDS MAINTENANCE, AVAILABILITY, INSPECTION, AUDIT AND CONFIDENTIALITY 6.1 Records. Provider agrees to maintain medical, financial and administrative records related to Covered Services rendered by Provider and as required by law, AHCCCS and CMS guidance, including the AMPM, this Agreement, and the Provider Manual. Such records must be maintained in an accurate and timely manner and in accordance with general standards applicable to such records. Medical records shall be maintained in a detailed and comprehensive manner that conforms to good professional medical practice, must be accurate, legible, signed and dated, and permits effective professional medical practice, effective professional medical review and medical audit processes, and facilitates an adequate system for follow-up treatment. Provider agrees to maintain such records, documents and any other information relating to this Agreement for ten (10) years or such longer period as required by law. A description of Provider’s patient, medical, dental and cost record keeping system(s) is included in Provider’s policies and procedures. 6.2 Audit and Inspection: 6.2.1 Provider acknowledges that UAHP, AHCCCS, CMS and/or the United States Department of Health and Human Services (HHS) may evaluate: the quality, appropriateness and timeliness of services furnished to Members; Provider’s and UAHP’s facilities; and any enrollment and termination enrollment records. Provider further acknowledges that UAHP, AHCCCS, CMS, HHS, the Comptroller General, or their designees, have the right to inspect any books, contracts, computer or other electronic systems, including medical records and documentation of Provider, or its subcontractors or transferees and other downstream entities related to UAHP’s Medicare Advantage contract, AHCCCS contract, the ability of UAHP or its subcontractors to bear the risk of potential financial losses, services performed, cost information or determination of amounts payable, through ten (10) years from the final date of the contract period or from the date of the completion of any audit, or for such longer period provided for in 42 CFR §422.504. If any such audit or inspection is requested by UAHP, AHCCCS, CMS, HHS, the Comptroller General, or their designees’ requested records shall be provided directly to HHS, the Comptroller General, or their designees. 6.2.2 Provider further agrees to cooperate with UAHP to facilitate the record and information exchanges necessary for the Utilization Information, Utilization Management, Quality Management, peer review, billing compliance or other programs required for UAHP, AHCCCS or CMS operations. Provider agrees to grant UAHP, AHCCCS, CMS, HHS or their designees such audit, evaluation, and inspection rights identified in this Section 6.2 as are necessary for UAHP to comply with its obligations under its contracts with CMS and AHCCCS. Whenever possible, UAHP will give Provider reasonable notice of the need for such audit, evaluation or inspection, and will conduct such audit, evaluation or inspection at a reasonable time and place. UAHP, AHCCCS, CMS, HHS or their designees, as applicable, shall be allowed to make notes and copies at no charge, subject to all applicable Federal and State laws and regulations relating to the confidentiality of patient medical records. Further, Provider agrees to furnish to UAHP at no charge copies of all medical records, x-rays, laboratory reports or any other patient care information within 10 working days of receipt of request. 6.3 Confidentiality of Medical Records. Provider, its PHPs, employees, subcontractors and agents shall maintain, use and disclose records and documents, both medical and non-medical, only as required or allowed by applicable Federal and State laws, rules and regulations including if applicable 42 U.S.C. §1395x(v)(1)(I), 42 C.F.R. § 422.118, Arizona Administrative Code, Title 9, Chapter 22, R9-22-402 (10) as amended, and UAHP medical records policies. In addition, Provider shall safeguard the confidentiality of Member information in accordance with applicable requirements governing the privacy and security of Protected Health Information (as defined in the HIPAA Privacy Rule, 45 C.F.R. § 160.103, promulgated under the Health Insurance Portability and Accountability Act of 1996 (“HIPAA”) and related regulations, including the Privacy of Individually Identifiable Health Information, 45 C.F.R. Parts 160 and 164, Subpart E, the HIPAA Security Standards, 45 C.F.R. Parts 160 and 164, Subpart C, the HIPAA Breach Notification Regulations, 45 C.F.R. Parts 160 and 164, Subpart D and the Health Information Technology for Economic and Clinical Health (HITECH) Act, as may be amended from time to time. 6.4 Continuity of Care. Consistent with laws relating to the confidentiality of patient medical records, Provider shall make the medical records of Members available to other Providers to assure continuity of care for Members. If Provider is not a Member’s PCP, Provider shall provide to Member’s PCP medical information in writing within thirty (30) days of initial date of service, describing all Covered Serviced provided to Member. 6.5 Survival. This Section shall survive the termination of the Agreement for services rendered while the Agreement was in effect. 7. TERM OF AGREEMENT, RENEWAL AND TERMINATION 7.1 Term of Agreement. This Agreement shall begin on the effective date set forth above and shall continue for two years unless continued or terminated as set forth below. 7.2 Renewal. This Agreement shall be automatically renewed under the same terms and conditions for additional two-year Terms unless either UAHP or Provider gives written notice to the other no fewer than sixty (60) days before the expiration of the Term or any renewal Term. 7.3 Termination For Cause. Provider or UAHP may terminate this Agreement at any time for cause. Cause includes, but is not limited to: (a) Failure of UAHP to secure a contract with AHCCCS or CMS, or cancellation, termination or material modification of UAHP's contract with AHCCCS or CMS. (b) Failure of UAHP to make required payments to Provider. (c) Initiation of bankruptcy proceedings by or against either party. (d) Material breach of this Agreement by either party. (e) Failure by Provider or UAHP to maintain licenses, federal certification, designation or registration required to perform Provider's or UAHP’s respective duties under this Agreement, or to comply with applicable laws or regulations. (f) Any misrepresentation or falsification of any information on any Provider's application provided by Provider to UAHP. (g) Any suspension, termination, limitation or reduction of any Provider’s privileges at any hospital or any Provider's failure to obtain or remain in good standing for privileges at a hospital. (h) Provider’s suspension, exclusion, restriction or debarment from any federal or state procurement activity. (i) Failure of Provider to take adequate action, as determined in the sole judgment of UAHP, to correct any deficiencies noted in Plan’s audit of Provider’s obligations under this Agreement or applicable federal or state law. (j) Commission or omission of any act or any conduct or allegation of conduct for which any Provider's license or ability to participate in Medicare or AHCCCS may be subject to revocation, suspension or limitation, whether or not actually revoked, suspended or limited, or if any Provider is otherwise disciplined by any licensing, regulatory, professional entity or any professional organization with jurisdiction over Provider. (k) Failure of any Provider to maintain required insurance and liability coverage protection, or failure of Provider to maintain such coverage on behalf of any PHP, employee and/or agent of Provider. (l) Commission or omission of any act or conduct by Provider which is detrimental to a Member's health or safety as determined by UAHP. (m) Billing, coding, and/or documentation which do not comply with relevant Medicaid or Medicare guidelines, relevant state or federal requirements, and/or relevant UAHP requirements. (n) Failure of Provider to meet with UAHP representatives upon reasonable request to discuss any/all Plan requirements. Any occurrence under paragraphs (e) through (m) above shall be grounds for immediate termination. Termination for any other reason set forth above shall be upon thirty (30) days advance written notice by the terminating party. UAHP may suspend, deny, refuse to renew or terminate the Provider in accordance with the terms of UAHP’s agreement with AHCCCS or CMS and applicable law and regulation. 7.4 Without Cause. This Agreement may be terminated at any time without cause or prejudice upon ninety (90) days advance written notice by either party. Should either party renegotiate terms after written termination notice received the original notice shall automatically be rescinded until renegotiations are final. A new written notice must be submitted for ninety (90) days termination to take effect. 7.5 Rights and Obligations Upon Termination, Plan’s Insolvency or Other Cessation of Operations. Upon termination of this Agreement, regardless of cause or reason, AHCCCS and CMS shall be notified and all rights and obligations of the parties relating to services during the term of and under this Agreement shall survive the termination. Upon termination, Provider's obligations or right to render Covered Services to Members or right to receive payment in accordance with this Agreement shall immediately cease, except for any payments due before such termination. Notwithstanding anything contained in this Section 7 to the contrary, services to Members to Medicare Advantage Beneficiaries will continue through the period for which payment has been paid to Plan, and services to Medicare Advantage Beneficiaries confined in an inpatient facility on the date of Plan’s insolvency or other cessation of operations will continue until their discharge. In addition, Plan shall continue to pay Provider in accordance with the provisions of this Agreement for Medically Necessary Covered Services provided by Provider to any AHCCCS Members hospitalized at the time of termination of this Agreement, pending discharge or transfer of such Member to a UAHP Participating Hospital when medically appropriate as determined solely by UAHP. In continuing to provide such Covered Services to AHCCCS Members or Medicare Advantage Beneficiaries, Provider shall abide by the applicable terms and conditions of this Agreement. Provider further agrees that (i) these hold harmless and continuation of benefits provisions shall survive the termination of the Agreement regardless of the cause giving rise to the termination and shall be construed to be for the benefit of Members; and, (ii) these provisions supersede any oral or written contrary agreement now existing or hereafter entered into between UAHP, a subcontractor or Provider and a Medicare Advantage Beneficiary or persons acting on their behalf that relates to liability for payment for, or continuation of, Covered Services provided under the terms and conditions of these clauses. Provider shall refund that portion of Capitation Payments received by Provider applicable to periods following termination of this Agreement, except for portions of the Capitation Payment for services rendered post-termination to Members in an inpatient facility. In addition, Provider shall refund to UAHP any moneys paid for Covered Services not rendered or not delivered in compliance with applicable laws, rules and regulations. Provider has no obligation under this Agreement to provide services to individuals who cease to be eligible and enrolled Members nor does UAHP have any obligation to make payment for any services provided to such individuals. Upon termination of this Agreement for any reason, the rights of each party under this Agreement shall terminate. Any such termination, however, shall not release Provider or UAHP from obligations under this Agreement in effect before the effective date of termination. 8. INSURANCE AND LIABILITY 8.1 Insurance. Provider shall be responsible for providing all health, accident, workers' compensation, general liability, automobile and other appropriate insurance for Provider and its employees and agents in connection with this Agreement. To the extent not provided by Provider, Provider shall require all PHPs maintain all necessary forms of insurance relating to the PHP’s provision of services under this Agreement, including to the extent applicable, general liability, accident, and automobile insurance. Provider shall provide UAHP with certificates of insurance annually. 8.2 Provider Professional Liability. Throughout the term of this Agreement, Provider shall maintain at Provider's expense for Provider general and professional liability coverage in a form and amounts acceptable to UAHP. Provider must also provide general and professional liability coverage for Provider’s PHPs, although the insurance coverage requirements of this Section may be met for Provider’s non-employed PHPs performing services pursuant to this Agreement if such PHPs are required to obtain, and do obtain, general and professional liability coverage in the form and amounts acceptable to UAHP. Policies under this provision must cover services performed in all locations, including services provided by Provider, and Provider’s PHPs, employees, contractors and agents outside of any Facility listed on Exhibit 1, including services provided in a Member’s home. At a minimum, coverage will be $1,000,000 per occurrence and $3,000,000 in aggregate. Certificates of insurance are to be provided to UAHP annually. In the event such coverage is claims-made insurance, Provider and/or PHP, as applicable, shall maintain such coverage continuously, and in the event of PHP leaving Provider, or termination of this Agreement, Provider shall secure, or require each such PHP secure, tail coverage with agreed limits of liability to provide continuous coverage for the period of the relevant statute of limitations for any claims that may arise against UAHP as a result of the act or omission of Provider or any PHP under this Agreement. Provider shall give UAHP thirty (30) days prior written notice of cancellation, modification or termination of any such insurance. Provider shall give UAHP prompt written notice of any claims against Provider's or any PHP’s professional liability coverage. 8.3 Indemnification. Provider shall hold harmless the State of Arizona, all State officers and employees, AHCCCS and employees of AHCCCS, all AHCCCS Members, and CMS in the event of nonpayment by UAHP to Provider. Provider shall further indemnify and hold harmless UAHP, its officers and directors, CMS, the State and AHCCCS, and their agents, officers and employees, against all injuries, deaths, losses, damages, claims, suits, liabilities, judgments, costs and expenses (including attorney’s fees) which may in any manner accrue against UAHP, its officers, and directors, CMS, the State or AHCCCS, or their agents, officers or employees, through the intentional conduct, negligence or omission of Provider, its PHPs, agents, officers, employees or contractors, arising out of or relating to this Agreement or the provision of services under this Agreement, although this provision does not create any obligation on the Provider to indemnify UAHP for damage caused to any Member enrolled in a Medicare Advantage plan as a result of UAHP’s denial of Medically Necessary care. Provider agrees that UAHP, its officers and directors, the State and AHCCCS, and their agents, officers and employees shall have no responsibility or liability for any taxes or insurance coverage described in this Agreement. 8.4 Survival. The provisions of this Section 8 shall survive the termination of this Agreement. 9. REPRESENTATIONS 9.1 Provider Representation. Provider represents and warrants that the information set forth in the UAHP Provider application is true and correct and that all such information regarding PHPs, if any, is true and correct. Provider shall promptly notify UAHP in writing of any changes in the information contained in the application, but in no event more than thirty (30) days of such change. 9.2 No Member Guarantees. UAHP makes no representations or guarantees concerning the number of Members it can or will refer to Provider under this Agreement. UAHP reserves the right to direct business to selected Providers at specified medical facilities or in specified geographic areas. 9.3 Marketing and Signage. Provider agrees that Provider's and each PHP’s name, office telephone number, address, specialty, language fluency and areas of special interest may be included in literature distributed by UAHP or any Plan to existing or potential Members and Participating Providers. UAHP may use Provider's and each PHP’s name and affiliation with UAHP or any Plan in advertising, promoting and soliciting Members in an effort to increase Membership and to otherwise carry out the terms of this Agreement and UAHP's contract with AHCCCS or obligations to CMS. Except as set forth above, Provider's or PHP’s use of UAHP's name, or of Provider’s name by UAHP or Plan, shall be upon advance written consent, such consent not to be unreasonably withheld. In addition, Provider may not use UAHP’s or any Plan’s logo in advertising a Medicaid plan unless prior approval is received by the AHCCCS marketing committee. 10. MEMBER AND PROVIDER GRIEVANCES, APPEALS, STATE HEARINGS AND DISPUTE RESOLUTION 10.1 Right to File a Grievance or Appeal/Claim Dispute. UAHP provides Members and Providers the right to file Grievances and/or Appeals and claim disputes in accordance with applicable law, including AAC R9-34 (AHCCCS Members) and 42 C.F.R. Part 422, Subpart M (Medicaid Advantage Beneficiaries). For Medicare Advantage Beneficiaries of a Medicare Advantage Special Needs Plan for dual eligible individuals, the Grievance and Appeals process shall be coordinated with processes applicable to Medicaid eligible Beneficiaries. Provider acknowledges its receipt of UAHP’s Grievance and Appeals procedures with the signing of this Agreement. UAHP’s Grievance and Appeals procedures are also set forth in the Provider Manual. Provider further acknowledges that the Grievance and Appeal procedures are binding on Members and Provider, that Provider must follow the claim dispute procedures set forth in the Provider Manual to dispute any claims not paid or not paid in full, and that UAHP’s decision regarding claim disputes for services provided according to the terms of this Agreement are final and binding. Provider and UAHP agree to attempt to resolve claim disputes informally prior to initiating a formal Appeal, however this provision does not operate as a waiver of any deadlines set forth in the UAHP’s policies and procedures. 10.2 Appeals and Requests for Fair Hearings. Provider acknowledges receipt of the UAHP Appeals and fair hearing procedures for Members and Providers and shall cooperate with UAHP in the implementation of that procedure and shall assist UAHP in taking appropriate corrective action. 10.3 Member Complaints. If Provider receives any complaint regarding Provider in connection with this Agreement, Provider shall notify UAHP within five (5) business days of receipt thereof of all details of such complaint. Provider shall make a good faith effort to investigate and resolve the complaint and inform UAHP of the resolution. In the event UAHP receives a complaint regarding Provider in connection with this Agreement, UAHP shall notify Provider of such complaint within five (5) business days of receipt thereof. 10.4 Member Appeals. Provider agrees to cooperate and comply with the UAHP’s Appeals procedures for review of Member Appeals, as established and amended from time to time by AHCCCS, CMS, or by UAHP, and set forth in the Provider Manual and any amendments thereto. 10.5 Member Hearings. In the event a Member obtains an adverse determination on the Member’s Appeal, the Member may request an administrative hearing as set forth in the Provider Manual. Provider agrees to cooperate and, when necessary, participate in any such administrative hearings and to comply with all final determinations pursuant to Grievance and Appeals policies and procedures. 10.6 Member Litigation. Each party shall promptly notify the other in writing of any claim or lawsuit, which has been asserted or is suspected or anticipated, which involves a UAHP Member or which may affect the other party. 11. CONFIDENTIALITY OF THIS AGREEMENT AND UAHP OPERATIONS. Unless otherwise required by AHCCCS, CMS or other rules or regulations, the terms and conditions of this Agreement, including financial rates and information relating to UAHP operations, are proprietary information and shall not be disclosed or disseminated by Provider or any of its agents or representatives whether during negotiations, during the term of this Agreement, or after its termination. 12. GENERAL PROVISIONS 12.1 Assignments and Delegation of Duties. Neither UAHP nor Provider may assign duties, rights or interests under this Agreement without the advance written approval of the other party and, as applicable, AHCCCS or CMS; provided, however, UAHP may assign its duties, rights and interests under this Agreement in whole or in part to a UAHP affiliate, subsidiary or other entity controlled by UAHP or may delegate any and all of its duties in the ordinary course of business, without Provider’s consent, subject to applicable laws, rules and regulations. 12.2 Independent Contractors. This Agreement is not intended to create nor shall be construed to create any relationship between UAHP and Provider other than that of independent contractors. Neither UAHP nor Provider is acting as the agents, employers, employees or representatives of the other. Provider and its PHPs, employees and any of Provider's independent contractors shall be solely responsible for the payment of any and all obligations for Worker’s Compensation Insurance, other insurance obligations, or any taxes, penalties, assessments and interest thereon which may be due or assessed by any governmental entity or agency, and shall hold UAHP, AHCCCS, CMS and the State of Arizona harmless therefore, which insurance, taxes, penalties, assessments and interest may arise out of monies earned, collected, paid to or charged by Provider for Covered Services rendered to Members. 12.3 No Third Party Beneficiary. This Agreement shall not create, or be deemed or construed to create, any rights in any third party, including, without limitation, any Member or UAHP Provider, or any partner, contractor, employee, agent or representative of the preceding. The above notwithstanding, UAHP and Provider acknowledge and agree that AHCCCS is intended to be benefited by, and shall have the rights of a third party beneficiary under this Agreement. 12.4 Physician Incentive Program. Notwithstanding any provision in this Agreement, UAHP and Provider agree to comply with all applicable Physician incentive plan requirements and conditions set forth in 42 C.F.R. § 417.479 as amended. Provider acknowledges that the provisions of 42 C.F.R. § 422.208 relating to Physician incentive plans apply to any subcontracting arrangements with a Medicare Advantage plan that utilizes Physician incentive plans in their payment arrangements with individual Physicians or Physician groups. 12.5 Venue. If litigation or arbitration is initiated to enforce this Agreement, after all applicable administrative processes have been exhausted, such action shall be filed and litigated, mediated or arbitrated in Tucson, Arizona. 12.6 UAHP’s Obligations to AHCCCS, HCS and CMS. Nothing set forth in this Agreement shall be deemed to amend, interpret, construe or otherwise affect in any way UAHP’s obligations to AHCCCS, HCG or CMS or the contracts between AHCCCS and UAHP, HCG and UAHP, or CMS and UAHP, as amended from time to time. To the extent there are any inconsistencies or contradictions between this Agreement and UAHP’s obligations to AHCCCS, CMS or HCG, or the contracts between UAHP and AHCCCS, CMS and HCG, respectively, the terms and provisions of the contracts shall prevail and control. 12.7 Interpretation. This Agreement shall be governed by and construed in accordance with all applicable Federal and Arizona laws, rules and contractual obligations of UAHP. 12.8 Merger, Reorganization, and Ownership Change. A proposed merger, reorganization or change in ownership of Provider shall require approval of AHCCCS and CMS and a subsequent contract amendment. 12.9 Amendments. UAHP may amend this Agreement, the exhibits and the Provider Manual by providing advance written notice to Provider in accordance with applicable law, policies and procedures as established by UAHP and AHCCCS. Failure of Provider to object in writing to any such proposed amendment within thirty (30) days following receipt of notice shall constitute Provider's acceptance of the amendment. In the event that Federal and State law or regulations should change, alter or modify the present services, levels of payments to UAHP, standards of eligibility of Members, or any operations of UAHP, such that the terms, benefits and conditions of this Agreement must be changed accordingly, then upon notice from UAHP, Provider shall continue to perform services under this Agreement as modified. In the event that any updates or revisions to the most current Healthcare Common Procedure Coding System (HCPCS), Current Procedural Terminology (CPT) or International Classification of Diseases (ICD) Codes should occur during the term of this Agreement, Provider agrees to employ the most recent update or revision without request by UAHP. Provider shall comply with the standards and code sets pursuant to HIPAA. 12.10 Exhibits. Exhibits are a part of this Agreement and their terms shall supersede those of other parts of this Agreement in the event of a conflict. 12.11 Entire Agreement. This Agreement, its Exhibits and the documents referred to in this Agreement constitute the entire agreement between the parties, and supersede all other understandings, express or implied, oral or written. 12.12 Notice. Any notice required under this Agreement shall be in writing and shall be sent by United States mail, postage prepaid, to the Chief Executive Officer at: The University of Arizona Health Plans Chief Executive Officer 2701 E. Elvira Rd. Tucson, Arizona 85756-7124 and to Provider at the first address set forth on the signature page of this Agreement, or to any other address Provider may designate in writing from time to time in accordance with this Notice provision. The date of receipt shall be deemed to be five (5) calendar days from the date of mailing. 12.13 Enforceability and Waiver. The invalidity and non-enforceability of any term or provision of this Agreement shall in no way affect the validity or enforceability of any other term or provision. The waiver by either party of a breach of any provision of this Agreement shall not operate as or be construed as a waiver of any subsequent breach thereof. No consent or waiver, express or implied, by either party of any breach or default by the other party in the performance by the other of its obligations under this Agreement shall be valid unless in writing and no such consent or waiver shall be deemed or construed to be a consent or waiver to or of any other breach or default in the performance by such other party of the same or any other obligations of such party hereunder. 12.14 Regulatory Approval. In the event that UAHP has not been licensed or has not received any applicable regulatory approval for use of this Agreement prior to the execution of this Agreement, this Agreement shall be deemed to be a binding letter of intent. In such event, the Agreement shall become effective on the date that such regulatory approval is obtained. If UAHP is unable to obtain such licensure or approval after due diligence, UAHP shall notify Provider and both parties shall be released from any liability under this Agreement; provided, however, that if such licensure or approval is obtained upon the condition of UAHP's amendment of this Agreement, then this Agreement shall continue and UAHP shall amend pursuant to Section 12.9. (The remainder of this page was intentionally left blank) IN WITNESS WHEREOF, the parties hereto have executed and delivered this Agreement as of the effective date. UNIVERSITY PHYSICIANS HEALTHCARE dba THE UNIVERSITY OF ARIZONA HEALTH PLANS Date: _________________________________ By: ___________________________________ (Signature) _________ James V. Stover_____________ (Please print or type name) Title: Chief Executive Officer Yavapai County Community Health Services Date: _________________________________ By: ___________________________________ (Signature) Chip Davis (Please print or type name) Title: Chairman, Yavapai County Board of Supervisors GROUP AHCCCS I.D. Number: See Exhibit 1 for individual AHCCCS ID #’s_______ GROUP NPI Number: See Exhibit 1 for individual NPI #’s______________ Federal Tax I.D. Number: 86-6000561 Tax I.D. Registered Name: Yavapai County Community Health Services Telephone Number: 928-583-1000 Fax Number: 928-771-3539 Correspondence Address: 1090 Commerce Dr (Please include the 9 digit zip code) Prescott, AZ 86305-3700 Pay to Address: 1090 Commerce Dr (Please include the 9 digit zip code) Prescott, AZ 86305-3700 Contract Address: 1090 Commerce Dr (Please include the 9 digit zip code) Prescott, AZ 86305-3700 EXHIBIT SCHEDULE FOR Yavapai County Community Health Services Exhibits Included in this Contract are marked with an “X” Providers: Exhibit 1 Provider Identification Exhibit 3 Compensation – Providers Exhibit 4 Compensation – Obstetrics Exhibit 5 Provider Disclosures (all Providers) Exhibit 6 Addendum (all Providers) (The remainder of this page was intentionally left blank) EXHIBIT 1 FOR Yavapai County Community Health Services Check One: Provider is Primary Care Provider Primary Care Provider including Obstetrics Specialty Care Provider (Specialty: ____ _____) Specialty Care Obstetrician Behavioral Health Provider Ancillary Service Provider ___ Other _____ Dental List of all Participating Providers and Practice Areas to provide Covered Services under this Agreement: Provider Name Location Josephine Kim, MD Jane Chapman, PA Frank Colella, FNP Ravinder Dawke, MD Yamini Goswami, DO Sean Murray, FNP Paul Nault, MD Sheryl Peteuil, FNP Mary Sutter, MD David Green, MD Joonwoo Bae, DMD Mark Emshwiller, DMD Richard Zapfe, DDS Practice Specialty OB/Gyn Physician Assistant, OB/Gyn Family Nurse Practitioner Family Medicine Family Medicine Family Medicine Family Medicine Family Nurse Practitioner Family Medicine Pediatrics Dentist Dentist Dentist AHCCCS ID# NPI # 861353 016776 1881798312 1598854564 178249 1417016759 225005 967979 563455 837693 834920 1275730780 1114011889 1265662233 1366449472 1306877170 502915 763749 471289 404228 334954 1528077781 1073516589 1386769412 1275800880 1972619153 Primary Service List all locations, phone, and fax numbers for Provider under this Agreement: Service Location 1090 Commerce Dr 51 Brian Mickelsen Parkway 3212 N Windsong Dr, 2nd Floor City, State Zip Prescott, AZ 86305-3700 Cottonwood, AZ 86326 Prescott Valley, AZ 86314 Phone 928-583-1000 Fax 928-771-3539 NPI# if applicable n/a 928-639-8132 928-771-3539 n/a 928-583-1000 928-771-3539 n/a NOTE: Provider must notify UAHP of additions or changes in locations and Providers, to get paid for services. *** If additional space is needed for Providers or locations, please attach a sheet indicating Providers and locations. Please indicate on the exhibit that there is an additional attachment. PROVIDER IS PARTICIPATING IN THE FOLLOWING PLANS (AND OTHER PLANS AS MAY BE DESIGNATED BY UAHP FROM TIME TO TIME): University Family Care KidsCare University Care Advantage University Healthcare Group (The remainder of this page was intentionally left blank) EXHIBIT 3 COMPENSATION – PROVIDERS FOR Yavapai County Community Health Services THIS EXHIBIT 3 ONLY APPLIES TO THOSE PROVIDERS CLASSIFIED AS PROVIDERS AS INDICATED IN EXHIBIT 1 SECTION 1. METHOD OF PAYMENT 1.1 General. Plan will reimburse Provider on behalf of Provider and PHPs, if any (hereafter collectively “Provider” except where otherwise noted) for the delivery of Medically Necessary Services to Members during the term of this Agreement. These services will be compensated, if such services are Medically Necessary and Prior Authorization/ Notification requirements of the Plan have been met. Payment will be based upon the lesser of the rates set forth in the Plan fee schedule or billed charges minus any applicable Co-payments, Coinsurance, and/or Deductible. University Family Care and KidsCare. Services shall be reimbursed at the lesser of billed charges or at one hundred percent (100%) of the AHCCCS fee schedule minus any applicable Co-payment, Coinsurance and/or Deductible as determined by the AHCCCS Administration for Covered Services. Upon complying with the notice requirements of Section 12.12 of this Agreement, UAHP reserves the right to change the percentage indicated above at its discretion. In the event that AHCCCS does not have a set fee schedule for a particular service UAHP shall reimburse Provider at the lesser of the current AHCCCS By-Report percentage of billed charges or one hundred percent (100%) of the Medicare fee schedule not to exceed Usual, Reasonable, and Customary charges minus any applicable Co-payment, Coinsurance and/or Deductible. In the event neither CMS nor AHCCCS has a set fee schedule for the particular service UAHP shall reimburse Provider at the current AHCCCS By-Report percentage of billed charges minus any applicable Co-payment, Coinsurance, and /or Deductible, based on Usual, Reasonable, and Customary rates for the area for Medically Necessary Medicare Covered Services provided. No reimbursement will be made for Covered Services that are determined to be unallowable, excessive or inappropriate after Retrospective Review by UAHP. AHCCCS is the payer of last resort. Therefore, after primary payment the reimbursement shall not exceed one hundred percent (100%) of the current AHCCCS fee schedule. University Healthcare Group. Services shall be reimbursed at the lesser of billed charges or at one hundred percent (100%) of the AHCCCS fee schedule minus any applicable Co-payment, Coinsurance and/or Deductible as determined by the AHCCCS Administration for Covered Services. Upon complying with the notice requirements of Section 12.12 of this Agreement, UAHP reserves the right to change the percentage indicated above at its discretion. In the event that AHCCCS does not have a set fee schedule for a particular service UAHP shall reimburse Provider at the lesser of the current AHCCCS By-Report percentage of billed charges or one hundred percent (100%) of the Medicare fee schedule not to exceed Usual, Reasonable, and Customary charges minus any applicable Co-payment, Coinsurance and/or Deductible. In the event neither CMS nor AHCCCS has a set fee schedule for the particular service UAHP shall reimburse Provider at the current AHCCCS By-Report percentage of billed charges minus any applicable Co-payment, Coinsurance, and /or Deductible, based on Usual, Reasonable, and Customary rates for the area for Medically Necessary Medicare Covered Services provided. No reimbursement will be made for Covered Services that are determined to be unallowable, excessive or inappropriate after Retrospective Review by UAHP. AHCCCS is the payer of last resort. Therefore, after primary payment the reimbursement shall not exceed one hundred percent (100%) of the current AHCCCS fee schedule. Mid-Level Providers. Other practitioners such as certified registered nurse first assist, registered and/or license nurse, certified registered nurse anesthesia, Nurse Practitioners, and physician assistants employed by or compensated by Provider in providing professional services shall bill with applicable modifier and reimbursed for all Medical Necessity Covered Services furnished to Members. UAHP shall reimburse Provider at the lesser of billed charges or eighty five percent (85%) of the current AHCCCS fee schedule minus any applicable Co-payment, Coinsurance and/or Deductible. In the event that AHCCCS does not have a set fee schedule for a particular service, UAHP will reimburse Provider at the lesser of the current AHCCCS By-Report percentage of billed charges or eighty five percent (85%) of the Medicare fee schedule not to exceed Usual, Reasonable, and Customary charges minus any applicable Co-payment, Coinsurance and/or Deductible. In the event neither CMS nor AHCCCS has a set fee schedule for the particular service the UAHP shall reimburse Provider at the current AHCCCS By-Report percentage of billed charges minus any applicable Copayment, Coinsurance, and/or Deductible, based on Usual, Reasonable, and Customary rates for the area for Medically Necessary Covered Services provided. No reimbursement will be made for Covered Services that are determined to be unallowable, excessive or inappropriate after Retrospective Review by UAHP. AHCCCS is the payer of last resort. Therefore, after primary payment the reimbursement shall not exceed one hundred percent (100%) of the current AHCCCS fee schedule. University Care Advantage. Services shall be reimbursed at the lesser of billed charges or one hundred percent (100%) of current CMS fee schedule for Covered Services furnished to Medicare Advantage Beneficiaries on a fee-forservice basis minus any applicable Coinsurance, Co-payment, and/or Deductible determined by Plan. In the event that CMS does not have a set fee schedule for a particular service and AHCCCS has a set fee schedule for the particular service UAHP shall reimburse Provider at the lesser of billed charges or one hundred percent (100%) of the current AHCCCS fee schedule minus any applicable Co-payment, Coinsurance and/or Deductible. In the event neither CMS nor AHCCCS has a set fee schedule for the particular service UAHP shall reimburse Provider at the current AHCCCS ByReport percentage of billed charges minus any applicable Co-payment, Coinsurance, and/or Deductible, based on Usual, Reasonable, and Customary rates for the area for Medically Necessary Medicare Covered Services provided to Medicare Advantage Beneficiaries. No reimbursement shall be made for Covered Services that are determined to be unallowable, excessive or inappropriate after Retrospective Review by UAHP. AHCCCS is the payer of last resort. Therefore, after primary payment the reimbursement shall not exceed one hundred percent (100%) of the current AHCCCS fee schedule. Mid-Level Providers. Other practitioners such as certified registered nurse first assist, registered and/or license nurse, and physician assistants employed by or compensated by Provider in providing professional services shall bill with applicable modifier and reimbursed for all Medical Necessity Covered Services furnished to Medicare Advantage Beneficiaries. UAHP shall reimburse Provider the lesser of billed charges or eighty five percent (85%) of the current CMS Professional fee schedule minus any applicable Co-payment, Coinsurance and/or Deductible. In the event that CMS does not have a set fee schedule for a particular service and AHCCCS has a set fee schedule for the particular service UAHP shall reimburse Provider at the lesser of billed charges or one hundred percent (100%) of the current AHCCCS fee schedule minus any applicable Co-payment, Coinsurance and/or Deductible. In the event neither CMS nor AHCCCS has a set fee schedule for the particular service UAHP shall reimburse Provider at the current AHCCCS By-Report percentage of billed charges minus any applicable Co-payment, Coinsurance, and/or Deductible, based on Usual, Reasonable, and Customary rates for the area for Medically Necessary Medicare Covered Services provided to Medicare Advantage Beneficiaries. No reimbursement shall be made for Covered Services that are determined to be unallowable, excessive or inappropriate after Retrospective Review by UAHP. AHCCCS is the payer of last resort. Therefore, after primary payment the reimbursement shall not exceed one hundred percent (100%) of the current AHCCCS fee schedule. Plan’s Medicare Advantage Plans may include mandatory additional benefits. Plan shall reimburse Provider for these mandatory additional benefits at the lesser of billed charges or at the Plan’s fee schedule for these mandatory additional benefits. Plan shall notify the Provider of any changes to the Plan’s covered mandatory supplemental benefits via the Plan’s Provider Resource Guide. SECTION 2 BILLING AND REPORTING REQUIREMENTS Required Claim Information. At a minimum, all Claims shall provide the information required within the CMS 1500 form and the following AHCCCS required information: Member’s name, sex and date of birth Member’s AHCCCS Identification or Medicare Number Diagnosis Code (International Classification of Diseases (ICD) Codes) Procedure Code (Current CMS Common Procedure Coding System HCPCS Codes including Current Procedural Terminology (CPT) Units of service Place of service Type of service Dates of service (must be reported using individual dates of service. Date spans are not acceptable) Amount billed (usual and customary) COB & subrogation flag (indicate yes/no) UAHP’s Authorization Number Provider’s name, address and authorized signature Provider’s AHCCCS Identification Number, AHCCCS assigned service locator code, or NPI, as applicable (The remainder of this page was intentionally left blank) EXHIBIT 4 COMPENSATION –OBSTETRICAL CARE FOR Yavapai County Community Health Services SECTION 1 METHOD OF COMPENSATION General Plan will reimburse Provider on behalf of Provider and Affiliated Physicians, if any (hereafter collectively “Provider” except where otherwise noted) for the delivery of Medically Necessary Services to Members during the term of this Agreement. These services will be compensated, if such services are Medically Necessary and Prior Authorization/Notification requirements of the Plan have been met. Payment will be based upon the lesser of the rates set forth in the Plan fee schedule or billed charges minus any applicable Co-payments. AHCCCS is the payer of last resort. Therefore, after primary payment the reimbursement shall not exceed one hundred percent (100%) of the current AHCCCS fee schedule. No reimbursement shall be made for Covered Services that are determined to be unallowable, excessive or inappropriate after retrospective review by Plan. Prior Authorization Provider must receive Prior Authorization from Plan for any Fee-For-Service Medically Necessary Covered service to the Member in accordance with Plan policies. Failure to follow the Prior Authorization/Notification process may result in denial of payment. Prior authorization is not a guarantee of payment. Provider must meet all terms and conditions of provision of care, documentation, and billing. Obstetrical Package Reimbursement Plan shall reimburse Provider the lesser of billed charges or one hundred (100%) percent of the current AHCCCS fee schedule allowable for Total OB Vaginal Delivery or Total OB Cesarean Delivery. A single Obstetrical Package will be paid for multiple births. If Provider does not perform the delivery, the Plan will pay the physician who performed the delivery based on the Plan fee schedule. Provider shall be reimbursed for antepartum and postpartum care based on the Plan fee schedule. Prenatal visits with resulting terminated pregnancy are billed with appropriate antepartum CPT codes. Excluded services within the obstetrical package will be paid at the Plan fee schedule. Fee Schedule Services shall be reimbursed at the lesser of billed charges or at one hundred percent (100%) of the AHCCCS fee schedule minus any applicable Co-payment, Coinsurance and/or Deductible as determined by the AHCCCS Administration for Covered Services. J -Codes shall be reimbursed at the lesser of billed charges or onehundred (100%) percent of the AHCCCS Fee Schedule minus any applicable Co-payment, Coinsurance and/or Deductible as determined by the AHCCCS Administration for Covered Services. Upon complying with the notice requirements of Section 12.12 of this Agreement, UAHP reserves the right to change the percentage indicated above at its discretion. In the event that AHCCCS does not have a set fee schedule for a particular service UAHP shall reimburse Provider at the lesser of the current AHCCCS By-Report percentage of billed charges or one hundred percent (100%) of the Medicare fee schedule not to exceed Usual, Reasonable, and Customary charges minus any applicable Co-payment, Coinsurance and/or Deductible. In the event neither CMS nor AHCCCS has a set fee schedule for the particular service UAHP shall reimburse Provider at the current AHCCCS By-Report percentage of billed charges minus any applicable Co-payment, Coinsurance, and /or Deductible, based on Usual, Reasonable, and Customary rates for the area for Medically Necessary Medicare Covered Services provided. No reimbursement will be made for Covered Services that are determined to be unallowable, excessive or inappropriate after Retrospective Review by UAHP. AHCCCS is the payer of last resort. Therefore, after primary payment the reimbursement shall not exceed one hundred percent (100%) of the current AHCCCS fee schedule. Mid-Level Providers. Other practitioners such as certified registered nurse first assist, registered and/or license nurse, certified registered nurse anesthesia, Nurse Practitioners, and physician assistants employed by or compensated by Provider in providing professional services shall bill with applicable modifier and reimbursed for all Medical Necessity Covered Services furnished to Members. UAHP shall reimburse Provider at the lesser of billed charges or eighty five percent (85%) of the current AHCCCS fee schedule minus any applicable Co-payment, Coinsurance and/or Deductible. In the event that AHCCCS does not have a set fee schedule for a particular service, UAHP will reimburse Provider at the lesser of the current AHCCCS By-Report percentage of billed charges or eighty five percent (85%) of the Medicare fee schedule not to exceed Usual, Reasonable, and Customary charges minus any applicable Co-payment, Coinsurance and/or Deductible. In the event neither CMS nor AHCCCS has a set fee schedule for the particular service the UAHP shall reimburse Provider at the current AHCCCS By-Report percentage of billed charges minus any applicable Copayment, Coinsurance, and/or Deductible, based on Usual, Reasonable, and Customary rates for the area for Medically Necessary Covered Services provided. No reimbursement will be made for Covered Services that are determined to be unallowable, excessive or inappropriate after Retrospective Review by UAHP. AHCCCS is the payer of last resort. Therefore, after primary payment the reimbursement shall not exceed one hundred percent (100%) of the current AHCCCS fee schedule. Obstetrical Care Package Components: Covered services for the obstetrical package include the following services: Initial Evaluation Antepartum Follow Up Visits Periodic Lab Services and Diagnostic Procedures Pre term Labor (office and hospital) False Labor (office and hospital) Labor Delivery (vaginal, spontaneous or assisted, or abdominal) Post Partum visits (office and hospital – including initiation family planning/contraception) Procedure Initial Evaluation Complete H & P & EPSDT if less than 21 years old Included In Package X X Lab Testing (Blood Draws) Glucose, finger stick Urine Dipstick HGB/HCT X X X X Follow-up Visits Provider Exam and History BP Weight FHT X X X X Ancillary Services Initial, Routine Ultrasounds for Size and Dates** Biophysical Profiles *** Non Stress Tests ** Complex Ultrasounds*** Stress Test External Version ER visits by Provider Rhogam - Pre & postpartum*** Labor & Delivery Cervical Ripening Artificial rupture of membrane Pitocin induction Vaginal delivery (vacuum, forceps) Cesarean section Multiple births Episiotomy/Repair Curettage, Postpartum Postpartum Care (6 weeks) Prior Authorization Required*** Amniocentesis CVS Excluded from Package X X X X X X X X X X X X X X X X X X X Genetic Counseling Diabetic counseling Ultrasounds (3+) X X X ** In addition to the Total OB package, 2 ultrasounds and 1 non stress test will be prior authorized. This means 2 authorization numbers will be issued for each OB member. If more than 2 ultrasounds and/or 1 non stress test are needed, a prior authorization request must be submitted for every additional test. *** Prior Authorization required for all services excluded from the obstetrical package. Excluded Services The Provider is not responsible for providing and the Plan is not responsible for paying costs for the Member Services set forth below. No Legal Obligation Medical Services for which neither the recipient nor any other person or organization incurs a legal obligation to pay. Such non-covered services may include, but are not limited to: Free chest x-ray provided by voluntary health organization Free samples of items received at no cost. Non Covered Services Services which are not covered with Participating Plans or Services which AHCCCS does not cover, including but not limited to: Services mandated for the purposes of meeting non-medical requirements, such as employment physicals and physician visits required for license, certificate, obtaining insurance, third party liability or disability payments. Services provided by or under the direction of naturopaths. Personal comfort items or services. Cosmetic surgery intended solely to improve the physical appearance of a recipient and which does not restore bodily function or correct a deformity. Reconstructive surgical procedures intended to improve function and appearance of any body which has been altered by disease, trauma, congenital or developmental anomalies or previous surgical processes unless the services are Covered Services that are Medically Necessary and Prior Authorized. Clear and precise documentation substantiating Medical Necessity for reconstructive surgery is required for a Covered Service determination. Post mastectomy breast reconstruction. An initial prosthesis, including a surgical brassiere, is covered if medically necessary. Therapeutic legally induced abortions and abortion counseling unless: o The abortion is performed to save the life of the mother with prior approval of the AHCCCS Office of the Medical Director. o The abortion is performed when the pregnancy is a result of rape or incest. Penile implants for recipients over 21 years of age. Infertility services, reversal of surgical sterilization, sex change operations. Hysterectomies unless medically necessary. Hearing aides except as allowed under EPSDT program for recipients under age 21. Eye examination and eyeglasses, except as allowed under EPSDT program, for recipients under 21. Glasses and contact lenses are not excluded if they are the sole prosthetic devise after cataract extraction. Routine dental care, except as allowed under EPSDT program for recipients under 21. Orthognathic surgery for recipients over 21 years of age. Outpatient occupational or speech therapy except as allowed under EPSDT, ALTCS, or KidsCare. Service for items requiring Prior Authorization for which prior authorization has not been obtained or has been denied. Services determined to be experimental or provided primarily for the purpose of research. Artificial or mechanical hearts of xenografts. Heart transplantation and allogeneic and autologous bone marrow transplantation, unless the recipient is categorically eligible. Liver transplantation, unless the recipient is categorically eligible and under age 21. Behavioral health services for non-categorically eligible acute care recipients, except for limited emergency/crisis stabilization services. Behavioral health services for ALTCS recipients ages 21 through 64, except for limited emergency/crisis stabilization services. Services to prison inmates or residents of a tuberculosis or Behavioral Health treatment center. Treatment for drug abuse unless authorized in the AHCCCS rules. Non emergency transportation for KidsCare Enrollees. Ineligible Covered Persons: Negative Retroactivity In the event the Plan determines at any time that a Member is ineligible or terminated from coverage by AHCCCS or the Plan, Provider shall return to Plan any capitation or fee for service payments paid by Plan for that Member on or after the effective date of Member’s termination or ineligibility. Provider may seek payment for Medically Necessary Covered Services provided to an ineligible or terminated Member after loss of eligibility or the termination date from either a new third party payer or from the individual. Supplemental Payment Program Provider has chosen not to participate in the supplemental payment program. Physician Incentive Regulations Notwithstanding any provision in this Agreement to the contrary, Plan and Provider shall comply with all applicable physician incentive plan requirements and conditions set forth in 42 C.F.R. SS 417.497 as amended. Risk Pool Sharing Provider has chosen not to participate in risk pool arrangements. EPSDT Provider agrees to fill out EPSDT tracking forms for pregnant members under 21 years of age as they qualify for EPSDT services and return to the Plan. The Plan uses the information to track and trend service needs of this population. Vaccines for Children (VFC) Program The vaccine portion of childhood immunizations shall be reimbursed through the State of Arizona’s VFC Program. It is the responsibility of Provider to submit billings to the VFC Program for reimbursement. The Plan will not reimburse Provider for the administration of the vaccines in excess of the maximum allowable as set by CMS. SECTION 2 BILLING AND REPORTING REQUIREMENTS General Regardless of the payment or reimbursement method (capitation or fee schedule), for every Medically Necessary Covered Service for which Provider seeks reimbursement on behalf of itself and all Affiliated Physicians, Provider agrees to submit a Clean Claim to Plan on a properly executed, current CMS 1500 form, and an itemized statement upon request of Plan, within ninety (90) days from the date of service, whether fee for service or capitated. Claims initially received more than ninety (90) days from the date of service will be denied. Plan agrees to pay Provider within forty-five (45) days receipt of a Clean Claim. Global Billing When appropriate, obstetrical services should be billed under a global services code. The Global Package consists of: Five (5) or more prenatal visits, delivery, and postpartum care. When billing globally, the claim should consist of two (2) lines. The first line is for the delivery charges and the second line is for the visit information (HEDIS line). Refer to the Provider Manual, OB Billing Requirements section for specific billing information. Non-Global Billing If less than 5 prenatal visits are provided, the OB package is not billed. The components provided are broken down into individual billable services. Refer to the Provider Manual, OB Billing Requirements section for specific billing information. Required Claim or Encounter Information At a minimum, all Claims or Encounters shall provide the information required within the CMS 1500 form and the following information: Ø Ø Ø Ø Ø Ø Ø Ø Ø Ø Ø Ø Ø Member’s name, sex and date of birth; Member’s AHCCCS Identification Number Diagnosis Code (International Classification of Diseases (ICD) Codes); Procedure Code (Current HCFA Common Procedure Coding System (HCPCS) Codes including Current Procedural Terminology (CPT) Units of service Place of service Type of service Dates of service (must be reported using individual dates of service. Date spans are not acceptable) Amount billed (usual and customary) COB & subrogation flag (indicate yes/no) Plan’s Authorization Number Provider’s name, address and authorized signature Provider’s AHCCCS Identification Number and AHCCCS assigned service locator code Failure to submit any of the above information and data, failure to respond to a request from Plan for additional information or data, or failure to comply with Plan’s Prior Authorization/Notification policy requirements of this Agreement within the described time period may result in delay or denial of payment. If Plan is subject to penalties or sanctions under its contract with AHCCCS due to failure of Provider to report or submit accurate claim or Encounter information, supported by the medical record, Provider shall either reimburse Plan or Plan shall deduct the amount of the penalty from future payments to Provider, on behalf of Provider or any Affiliated Physician, at the sole discretion of Plan. If any Provider’s failure to comply with Plan’s policies and procedures or this Agreement result in either (1) inappropriate or unauthorized medical expenses, or (2) sanctions to Plan, Plan may deduct such costs from future payments to Provider or demand repayment from Provider. Encounters and claims are to be mailed to: University Family Care PO Box 35699 Phoenix, AZ 85069-5699 University Healthcare Group PO Box 37279 Phoenix, AZ 85069-7279 University Care Advantage PO Box 38549 Phoenix, AZ 85069-8549 Retrospective Review Through retrospective review, Plan shall ensure that services rendered were Medically Necessary Covered Services, provided in compliance with AHCCCS Medical Policy Manual (AMPM) guidelines and medical standards of care, and substantiated with documentation supporting the level of services billed as specified by AHCCCS regulations. Plan shall deny any claim not satisfying these criteria. Plan shall conduct retrospective review on both a pre-payment and post-payment basis. Plan may deduct the amount of erroneous payments from future payments to Provider or demand repayment from Provider. Claims Processing Plan’s date of receipt of claims is the date the claim was received by Plan as indicated by the date stamp on the claim and the claim reference number. Claims will be considered paid on the date indicated on disbursement checks. Denied claims will be considered adjudicated on the date of their denial. Claims that are denied and are resubmitted will receive new date stamps. Claims that are pending for additional supporting documentation from Provider will receive new date stamps upon receipt of the additional documentation except as provided under Section 2.4 of this Exhibit. SECTION 3 COORDINATION OF BENEFITS Plan is the payer of last resort and Provider shall identify and first bill other third-party carriers or insurers. If Member has third-party coverage, including, but not limited to Part A or Part B Medicare, Provider shall identify and seek such payment before submitting claims to Plan in accordance with the following: Provider shall include a completed copy of the third-party carrier’s explanation of benefits (EOB) or remittance advice (RA) when submitting a claim for a non-capitated service for the balance due under non-duplication of benefits. A claim, plus a completed copy of the third-party carrier’s EOB or RA for any balance due, must be initially received by the Plan within sixty (60) days form the third-party carrier’s EOB or RA date. For Members, only the difference between the Medicare allowable charges, as shown on the Explanation of Medicare Benefits (EOMB), and the Medicare reimbursement received, will be eligible for payment by Plan. Plan’s payment of coinsurance plus any applicable deductibles will constitute payment in full to Provider. For Plan’s non-Medicare Members, the allowed amount will be based upon the Plan fee schedule, less the paid amount of the other third-party carrier(s); any balance of which will be paid by Plan as non-duplication of benefits. In the event Provider identifies any third party source of payment or liability, Provider shall immediately notify Plan of such source. SECTION 4 CLAIMS RESUBMISSION Provider may resubmit claims that have been denied or adjudicated by Plan, but they must be received by Plan within one-hundred and twenty (120) days from the date of the initial Plan EOB. Plan will re-adjudicate claims resubmitted by Provider only if an initial claim has been filed within the described submission deadline. Claim submissions shall be designated as such and shall consist of the following: Ø Ø Ø Ø Copy of claim Copy of Plan remits Supporting documentation; and Written explanation as to reasons for resubmission. Resubmitted claims are to be addressed and mailed to the Plan Claims Department at the following address: University Family Care PO Box 35699 Phoenix, AZ 85069-5699 University Healthcare Group PO Box 37279 Phoenix, AZ 85069-7279 University Care Advantage PO Box 38549 Phoenix, AZ 85069-8549 A tracer claim may be submitted in follow up to claims that have been determined to be “not received” or “not in the system” by the Plan. Tracer claims must be received within 90 days from the date of service and must be marked “tracer” or “second submission”. Tracer claims should not be submitted less than 21 days from the first submission, allowing for processing of the original claim. (Remainder of page intentionally left blank) EXHIBIT 5 FOR Yavapai County Community Health Services Provider Disclosures List the name, address, and, if applicable, date of birth, social security number and tax id number, of any person (individual or corporation) with an ownership or control interest in Provider. This includes any person with a direct and/or indirect interest of 5% or more in the Provider, an owner of an interest of 5 percent or more in any mortgage, deed of trust, note, or other obligation secured by the Provider if that interest equals at least 5 percent of the value of the property or assets of the Provider, is an officer, director or partner in Provider if organized as a corporation or partnership. The address for corporate entities must include, as applicable, primary business address, every business location and PO Box address. If the person (individual or corporation) with an ownership or control interest in Provider is related to another person with ownership or control interest in the Provider as a spouse, parent, child, or sibling; or whether the person (individual or corporation) with an ownership or control interest in any subcontractor in which the Provider has a 5% or more interest is related to another person with ownership or control interest is related to another person with ownership or control interest in the disclosing entity as a spouse, parent, child, or sibling. Also include the name of any other disclosing entity in which an owner of the Provider has an ownership or control interest. Name Address Date of Birth SSN (The remainder of this page was intentionally left blank) Tax ID EXHIBIT 6 FOR Yavapai County Community Health Services ADDENDUM This Addendum contains specific provisions that apply to specific Provider-types, based on medical specialty. Providers should take care to identify the provisions applicable to their medical specialty as they are required to comply with the requirements listed that apply to their specific Provider-type. A. PRIMARY CARE PROVIDER OR PCP Each PCP shall accept a panel of no less than 100 Members. AHCCCS enrollees may not be a majority of PCP’s patient panel. 2. Each PCP shall supervise, coordinate and provide Medically Necessary Covered Services to Members through the following mechanisms (except for children’s dental services when provided without a PCP referral): 2.1. Counsel Members and their families regarding the Member’s medical care needs, including family planning and Advance Directives; 2.2. Initiate referrals for Medically Necessary Covered Services to UAHP’s contracted Participating Providers, in accordance with generally accepted standards of medical practice in the community and the Provider Manual. 3. Provide preventive health services in accordance with AHCCCS rules and regulations, and UAHP policies, as applicable. Preventive health services shall include, but not be limited to: 3.1. Periodic health assessments for all AHCCCS Members twenty-one (21) years of age and over that include major medical, social history and family history within a two (2) year period; 3.2. Immunization and tuberculosis screening (but not immunizations solely for travel) and other measures for the prevention and detection of disease, including instruction in personal healthcare measures and information on proper and timely use of medical resources; 3.3. EPSDT services for all AHCCCS Members up to the age of twenty-one (21) years in accordance with UAHP policies and utilizing AHCCCS EPSDT periodicity schedules, tracking forms and specific behavioral health services for certain eligible Members. Provider shall comply with all AHCCCS records and audit requirements for EPSDT services. EPSDT Periodicity Tables are located in the EPSDT Section of the Provider Manual. 3.4. Provider will strive to meet or exceed the AHCCCS Minimum Standard for each performance indicator. If the Provider has met or exceeded the performance standard, the Provider will strive to meet or exceed the AHCCCS goal, and then benchmark. The UAHP Quality Improvement Department will measure these performance indicators on a yearly basis. 4. The PCP must maintain each assigned Member’s continuity of care. 5. The PCP must maintain the Member’s medical record, including documentation of all services provided to the Member by the PCP, as well as any specialty or referral services including behavioral health. 6. When a PCP receives behavioral health information from the RHBA or Provider about an assigned Member, the PCP must establish a medical record for the Member, even if the PCP has not yet seen the assigned Member. In lieu of actually establishing a medical record, such information may be kept in an appropriately labeled file but must be associated with the Member’s medical record as soon as one is established. 7. The PCP must respond to RHBA/Provider and other treating Provider requests for the Member’s clinical information within ten (10) business days of receiving the request. The response should include all pertinent information, including, but not limited to, current diagnoses, medications, laboratory results, last PCP visit, and recent hospitalizations. The PCP must document or initial signifying review of Member behavioral health information received from a RHBA behavioral health Provider who is also treating the Member. 8. AHCCCS maintains clinical took kits for the treatment of anxiety, depression, and ADHD which are available to PCPs in their treatment of Members. These tool kits are a resource only and may not apply to all patients and all clinical situations, and are not intended to replace clinical judgment. 9. If the RHBA/behavioral health Provider provides documentation to UAHP that step therapy has already been completed, or is medically contraindicated, the AHCCCS Member shall be continued on the medication at the dosage at which the Member has been stabilized unless there is subsequently a change in the Member’s medical condition. PCPs shall prescribe medication at the dosage at which the Member has been stabilized. 10. When a PCP has initiated medication management services for an AHCCCS Member to treat a behavioral health disorder, and it is determined by the PCP or UAHP that the Member should be transferred to a RHBA prescriber for evaluation and/or continued medication management services, PCP or UAHP shall coordinate the transfer of care. 11. If serving children, the PCP must enroll as a “Vaccines For Children” Provider. 1. B. 1. 2. 3. 4. 5. 6. 7. 8. 9. PROVIDER INCLUDES OBSTETRICS WITHIN PROVIDER’S SCOPE OF PRACTICE Provider shall have training and experience in obstetrics/gynecology, have completed an approved training program, or be generally recognized by the Physician community as being skilled in obstetrical/gynecological practice. Provider shall provide Medically Necessary obstetrical/gynecological Covered Services to Members with the same standard of care, skill and diligence customarily used by licensed Obstetricians/Gynecologists in the community in which such services are rendered. Provider shall obtain Prior Authorization in accordance with the UAHP’s list of obstetrical services requiring Prior Authorization/Notification. Provider shall make provisions and schedule appointments for enrolled pregnant Members to obtain initial and ongoing prenatal care consistent with the appointment standards set forth in the Provider Manual. Provider, upon the receipt of a PCP referral for continued obstetrical care, shall report the referral to the UAHP patient coordinator (the “Coordinator”) within two (2) working days. Provider shall report all multiparity pregnancies to the Coordinator within one (1) week of identification of multiparity. PCP Providers providing continued obstetrical care shall report any pregnancy to the Coordinator within (2) working days and shall report all multiparity pregnancies to the Coordinator within one (1) week of identification of multiparity. Referrals by PCPs to Provider are valid through the termination of pregnancy and for the number of days postpartum required by AHCCCS or the applicable Commercial Plan, provided Member has continued UAHP enrollment. Provider may refer Members to a UAHP participating perinatologist for consultation and/or continued obstetrical care upon Prior Authorization from UAHP. Provider shall cooperate with perinatal case management and other perinatal support programs that may be authorized by UAHP. All Physicians and certified nurse midwives who perform deliveries shall have OB hospital privileges or a documented hospital coverage agreement for those practitioners performing deliveries in alternate settings. (The remainder of this page was intentionally left blank)