SCP for Tinzaparin
advertisement
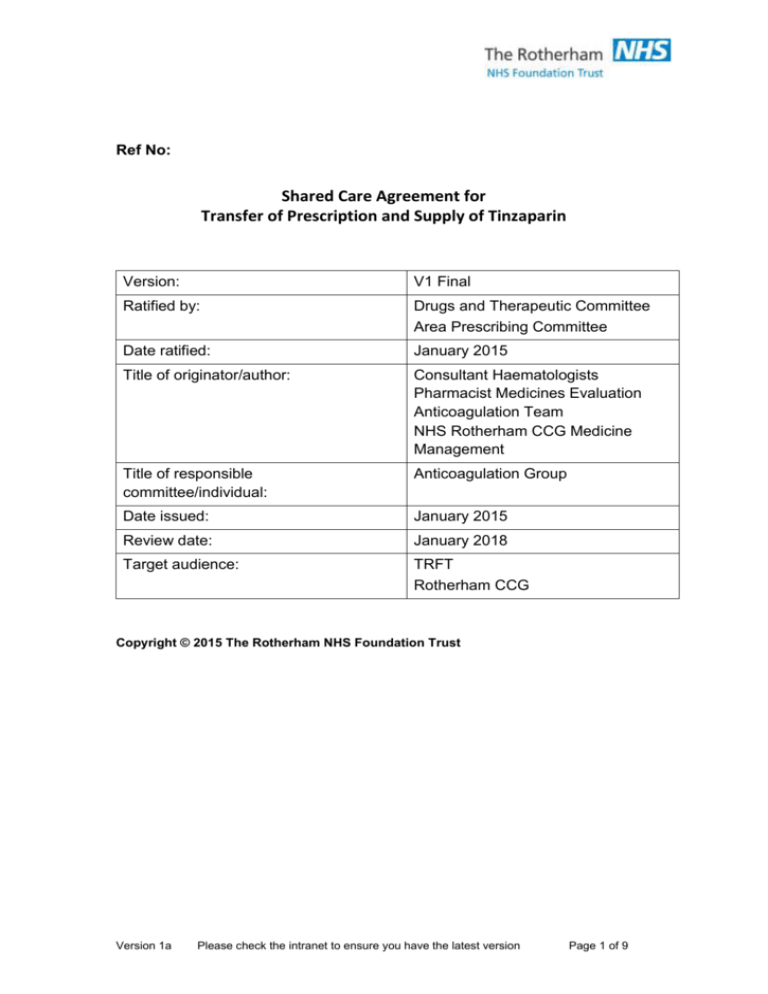
Ref No: Shared Care Agreement for Transfer of Prescription and Supply of Tinzaparin Version: V1 Final Ratified by: Drugs and Therapeutic Committee Area Prescribing Committee Date ratified: January 2015 Title of originator/author: Consultant Haematologists Pharmacist Medicines Evaluation Anticoagulation Team NHS Rotherham CCG Medicine Management Title of responsible committee/individual: Anticoagulation Group Date issued: January 2015 Review date: January 2018 Target audience: TRFT Rotherham CCG Copyright © 2015 The Rotherham NHS Foundation Trust Version 1a Please check the intranet to ensure you have the latest version Page 1 of 9 Version Date Version 1a February 2013 Draft This is a new protocol Version 1a March 2013 Draft Circulated Consultant Haematologists Anticoagulation Specialist Nurses NHS Rotherham Medicines Management Version 1b November 2014 Draft Comments incorporated Approved January 2015 Renamed as Version 1 Final Version 1a Author Status Comment Please check the intranet to ensure you have the latest version Page 2 of 9 Shared Care Protocol Prescribing and Supply of Tinzaparin This should be read in conjunction with the current Summary of Product Characteristics http://medicine.org.uk 1 Indications Licensed: Prevention of VTE in surgical patients Treatment of VTE and PE Unlicensed: Prevention and treatment of VTE in pregnancy 2 Patients suitable for Primary Care continuation Injectable drug users Pregnant patients with VTE or at high risk of VTE Patients with contraindications to vitamin K antagonists Patients unable to be stabilised on Vitamin K antagonists Patients undergoing cancer therapies or with metastatic disease 3 Contraindications Active bleeding Sever hypertension 230/120mmHg or higher Severe hepatic disease Severe renal disease Haemophilia and other untreated inherited bleeding disorders Acute bacterial endocarditis Recent neurosurgery or eye surgery Thrombocytopenia with platelets less than 75x109/L History of heparin Induced Thrombocytopenia (HIT) Hypersensitivity to heparin, tinzaparin or other low molecular weight heparins 4 Drug interactions 5 Adverse drug reactions 6 Base line investigations By TRFT 7 Monitoring by GP Version 1a Clopidogrel NSAIDS Dypyridamole Increased risk of bleeding ACE inhibitors Angiotensin II receptor antagonist increased risk of hyperkalaemia Anticoagulant effect enhanced Haemorrhage Thrombocytopenia Hyperkalaemia Osteoporosis with prolonged use Alopecia Injection site reactions Skin necrosis Hypersensitivity reactions These will be undertaken by TRFT: Day 1 - FBC, U&E , eGFR , LFT Day 5 - FBC FBC – Day 14 Patient’s weight when represcribing tinzaparin Please check the intranet to ensure you have the latest version Page 3 of 9 8 Tinzaparin preparations Prefilled syringes Strength 9 Syringes available Use prefilled syringes only 10000 units/mL 2500 units in 0.25 mL 3500 units in 0.35mL 4500 units in 0.45 mL Do not use vials 20000 units/mL 10000 units in 0.5 mL 14000 units in 0.7 mL 18000 units in 0.9mL Doses Tinzaparin Prescribing Advice See Appendix 1 Doses are based on weight and renal function (eGFR). 10 Route Subcutaneous 11 Pharmaceutical aspects Assessment and training of patients for self-administration. To consider care by district nurses for patients unable to self-administer. Disposal of syringes: sharps bins will be provided with the syringes. Disposal of sharps bins: patient will be given information regarding collection of sharps bins by Rotherham Council. 12 Secondary care Contact information If stopping medication or needing advice, please contact Consultant initiating treatment with tinzaparin Consultant haematologist 13 Criteria for shared care Prescribing responsibility will only be transferred when: Treatment is for specified indication and duration. Treatment has been initiated and established by the secondary care specialist. The patient’s initial reaction to and progress on the drug is satisfactory. The GP has agreed in writing in each individual case that shared care is appropriate. The patient’s general, physical, mental and social circumstances are such that he/she would benefit from shared care arrangements. 14 Responsibilities of initiating consultant Initiate treatment. Undertake base line monitoring. Prescribe dose based on indication/weight/eGFR. Monitor patients initial reaction to and progress on the drug. Ensure that patient has an adequate supply (14 days) of medicine until GP supply can be arranged. Continue to monitor and supervise the patient according to this protocol, while the patient remains on this drug. Provide GP with: Diagnosis, relevant clinical information and baseline results, treatment to date, treatment plan, duration of treatment before consultant review. Patient weight and baseline eGFR, platelet, potassium levels. Provide GP with details of outpatient consultations, ideally within 14 days or inform GP if the patient does not attend appointments. Advice on when to stop drugs. Informed consent to therapy. Understanding of potential side effects and appropriate actions. Understanding of the role of monitoring. 15 Responsibilities of primary care Version 1a Accept referral from secondary care. Reinforce educational points provided by the hospital. Monitoring of FBC on day 14 to complete monitoring for heparin induced thrombocytopaenia (HIT). Monitor for hyperkalaemia in those patients at higher risk of raised Please check the intranet to ensure you have the latest version Page 4 of 9 16 Supporting documentation 17 Patient monitoring booklet GP letter 18 Version 1a plasma potassium concentrations (those with diabetes mellitus, chronic renal failure, acidosis, raised potassium concentrations, those taking potassium sparing drugs/potassium supplements or patients on long term treatment). Monitoring should be done regularly in these patients according to the judgement. Reweigh non-pregnant patients on long term tinzaparin at a frequency according to clinical judgement. Monitor renal function and seek advice if there is deterioration. Keep records or register of all patients for whom tinzaparin has been prescribed. Records should include details such as indication, concurrent medication, dose, start date, expected duration, monitoring details, adverse incidents, consultants involved in treatment, any advice or actions. To ensure that monitoring and dosage record is kept up to date Discontinue treatment if the patient experiences severe side effects and the relevant contact at the hospital is not available. Conformation letter to patient and/or carer if treatment is discontinued. Conduct audit /annual review as deemed appropriate. Tinzaprin patient information leaflet given with sharps bins: For prevention For treatment None Attached below Please check the intranet to ensure you have the latest version Page 5 of 9 References: National Institute of Clinical Excellence Venous thromboembolism: reducing the risk: Reducing the risk of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in patients admitted to hospital (CG92; 2010) http://publications.nice.org.uk/venous-thromboembolism-reducing-the-risk-cg92 Royal College of Obstetrics and Gynaecology The acute management of thrombosis and embolism during pregnancy and the puerperium, the acute management (37b; 2010) http://www.rcog.org.uk/files/rcog-corp/GTG37b_230611.pdf Royal College of Obstetrics and Gynaecology Reducing the risk of thrombosis and embolism during pregnancy and the puerperium http://www.rcog.org.uk/files/rcog-corp/GTG37aReducingRiskThrombosis.pdf National Patient Safety Agency Reducing treatment dose errors with low molecular weight heparin http://www.nrls.npsa.nhs.uk/resources/?q=0%c2%aclow+molecular+weight+heparin%c2%ac Department of Health Accurate patient weight Medical patient weighing scales http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_114048.pdf All Wales Medicines Strategy Group Prescribing of low molecular weight heparin in Wales http://www.wales.nhs.uk/sites3/Documents/371/Published%20to%20website%20v1.5.pdf Sheffield Teaching Hospitals NHS Foundation Trust and NHS Sheffield Shared Care Protocol for the prescription and supply of dalteparin (2012) All Wales Medicines Strategy Group Template for Shared Care Protocols (Adapted) Leo Pharma Summary of Product Characteristics Innohep Version 1a Please check the intranet to ensure you have the latest version Page 6 of 9 Patient name The Rotherham NHS Foundation Trust Unit No Tinzaparin Shared Care Form Date of birth Fax this form referral to GP for ongoing prescription of Tinzaparin in accordance with the TRFT Tinzaparin Shared Care Agreement. TRFT will provide initial 14 days supply and monitor full blood count on day 1 and 5 – 7. GP to monitor full blood count on day 12 - 14 GP to continue prescribing and carry out further monitoring as appropriate. Patient’s medical care remains with the hospital consultant who initiated tinzaparin. Refer to Consultant Haematologist for further thrombosis care where appropriate. 1. REFERRING CONSULTANT Referring Consultant_______________________Consultant contact number____________________ Fax Number ________________ Next consultant clinic appointment___________________________GP/Practice referral____________________________ 2.INDICATION FOR TINZAPARIN VTE Prophylaxis VTE treatment □ Pregnancy □ Central line □ Surgery □ Cancer □ Pregnancy □ Injectable drug use □ Associated cancer/ cancer therapies □ Unsuitable for oral anticoagulants 3. TREATMENT INFORMATION Patient details: Weight ____________kg Dose of tinzaparin_________________units ONCE/TWICE daily (delete as appropriate) Proposed duration of treatment: 6 weeks□ Tinzaparin to be administered by: 3 months□ Patient or carer□ 6 months□ long term□ Other___________________ District nurse □ (fax this form together with DN referral) Further relevant information (clinical problems, concurrent medication):□ 4. MONITORING REQUIREMENTS Baseline results: eGFR____________micromol/1.73m2 Platelets________________(X109/L) Potassium__________________(mmol/L) □ Heparin induced thrombocytopenia (HIT) monitoring is complete (Day 1, 5 and 14) or □GP to monitor FBC day 14 to HIT monitoring. 5. FORM COMPLETED BY Signature__________________________Print name___________________________Designation___________________________ Contact No. (bleep/ext)__________________Date_____________________ Faxed by:_____________________________Time________________________________Date_____________________ Received at GP practice by: _____________ ______Time__________________Date_______________________________ (Sign and fax back to sender to confirm referral has been received) This fax is confidential and is intended for the person to whom it is addressed. If you have received this fax in error, please notify us immediately and return in the post to us. If the reader of this fax is not the intended recipient you are hereby notified that any distribution or copying of the message is strictly prohibited. Version 1a Please check the intranet to ensure you have the latest version Page 7 of 9 Tinzaparin Shared Care Agreement for Transfer of Prescribing and Monitoring from Hospital to Primary Care Patient……………………………………………… Consultant………………………………………… Speciality…………………………………………. Name of General Practitioner: Dr………………………………………………………………………….... Name of GP Practice: ……………………………………………………………………………………………… □ I am happy that from………/………/20…………… the practice will take over the prescribing of Tinzaparin for the above patient in accordance with the shared care guidelines which are attached. □ The practice is happy to supply Tinzaparin for the duration stated. □ The practice is happy to undertake monitoring as above. □ I also confirm that I will take appropriate action, in accordance with the above- mentioned Guidelines in the event of abnormal blood tests or other adverse reactions, and will inform the patient’s Consultant if I advise the patient to stop □ Tinzaparin treatment □ I am aware that the consultants are happy to be contacted about their patients via their secretaries if there are any concerns. GP Signature………………………………………………………Print Name…………………………………………….. Date………………………………………………… Please FAX once complete to the Consultant. Version 1a Please check the intranet to ensure you have the latest version Page 8 of 9 Appendix 1 Tinzaparin prescribing chart (to insert following review January 2015) Version 1a Please check the intranet to ensure you have the latest version Page 9 of 9