Bridging the Health Management & Clinical Divide in Innovation
advertisement
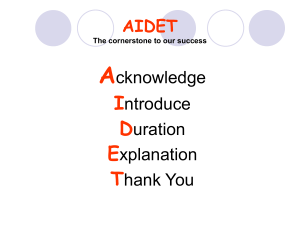
Bridging the Health Management & Clinical Divide in Innovation Presenter: Dr. Larry Gamm, Texas A&M University Recorded on: December 5, 2012 Meeting, with Jim Benneyan and Eva Lee from our partner universities, at Northeastern and Georgia Tech respectively, and it's also based on large part on a paper that Nick is the lead author on that has been submitted to health services research. The presentation is based on our workshop projects, supported by the National Science Foundation, Student Group, San Luis Obispo Health System, and The Medical University of South Carolina in Charleston, South Carolina. St. Luke's, of course, in Houston, Texas. This presentation focuses on, principally, on a project at St. Luke's, that began just over a year ago. But we're also drawing on some insights we've already gained from our Medical University of South Carolina project that just got underway about six months ago. So let me begin then with thank you to our coworkers on this, Sherry Lin, and Jennifer Griffith, and Debbie Talwar who participated in this. >> Just a moment. >> Hello? >> Yes, yes>> Hey, Sharon, this is Nick. We're going. I'm gonna put you on mute, but just flag me if you wanna have any questions. >> I hope people will know how to get on it, because there were two numbers. I hope they can get on it. >> We've got seven or eight attendees, so I think everyone's figuring it out. >> Okay, good, okay. >> All right, we'll keep going now. >> Okay thank you, so we just are getting underway. We're on the first side. We're gonna switch now to the topic of the hard stuff is the soft stuff and that quote I've seen frequently in discussions with implementation of electronic medical records or implementation of quality improvement or patient safety and so forth, that says in effect that we may have hardware, we may have the basic processes identified, but we don't necessarily know how to effectively implement those activities. So, I begin with the notion here that organizations like health systems, educational institutions and law firms and so forth are considered professional organizations and they present particular problems for management. I used to tell my students, I used to head up MHA programs, that the hardest organization to manage is a hospital. As a university, the only that's harder to manage than a university is a hospital and the only thing harder to manage than either of those is an academic health center or a university hospital. And part of that is based upon the fact that you're dealing with professionals that are focused on doing the job the way they learned how to do it and so forth and so when you start talking about changing practice. You frequently have to bridge this divide between management, on the one hand, and professionals. Fortunately some of our managers today are also trained professionals, and help bridge that divide. One way of not to do it is what you saw on 60 Minutes this weekend, where health management associaties was featured as an example of how management tried to control physician behavior and in effect setting quotas, or requiring that physicians admit 20% of their ER patients to the hospital. And obviously, that's illegal and runs afoul of Medicare and a number of other statutes. So in any case, that's not what we're talking about in terms of an example of bridging the divide. On the other hand, the Student Group evidence-based leadership approach really offers an opportunity to strengthen. We've management on the one hand and patient practices on the other. So the question, of course, is how can management contribute to changing care practices among professionals, physicians, nurses, and other support personnel? The contrast that we'd like to make is between two extremes on the continuum. One is the loosely coupled organization, which often is used to describe professional organizations. When you're trying to manage a professional corps, and/or you're also trying to manage such professionals in a number of different sites and there is usually a good bit of autonomy left in the hands of the professionals and other practitioners. At the other extreme our highly liability organizations that are getting a good bit of press now in healthcare particularly in patient safety area. But in organizations, you're really talking about standardizing behaviors to the extent errors are almost impossible, because they would have disastrous consequences. And traditionally thought of HROs, such as nuclear power plants or air traffic control towers. And the like. Now I'll turn it over to Dan. >> All right, so we wanna talk briefly about what we mean by loose coupling. That might be a new term to many of you on the webinar here today, but it's a framework we use to evaluate what one of the benefits of major system-level change initiatives are. And so first a little about loose coupling and what exactly it's driven by. What we say when an organization is loosely coupled is that there's a couple of drivers behind that, and how exactly a hospital could arrive at being a loosely coupled organization. Two of those reasons are causal indeterminacy, something we call causal indeterminacy versus indeterminacy and what we see with indeterminacy is that agents are unable to fully comprehend the complicated ends, means, nature of their work. So you can imagine at other industries where the outcomes are immediate and more visible to someone, someone working on a production line, let's say. They can immediately see the impact of their work. That would be causable determinacy. They can see exactly what it does so if you're painting a toy truck on a production line, you can see if your paint job is shoddy, the end project is shoddy. Issues of course with health care and why we see loose coupled organizations in health care is because there's lots of intangible outcomes. And we've got hundreds of touch points by many different nurses, lobotomists, to lab techs, to custodial staff and physicians and no single touch point necessarily has a direct impact on the outcome so that's causal indeterminacy. So that's one of the root causes of loose coupling. The other DEG example of what we call fragmented internal environment. As we're aware hospitals and hospital nurses are technical specialists with specific units. They're charged with caring for patients in only their unit. For example, a nurse in neonatal intensive care unit is not responsible for, nor really has the opportunity to interact with an adult patient in a thoracic unit. As a result, very few individuals within a hospital are concerned about the system level health of the hospital. So they're basically the organization becomes loosely coupled because very few participants are constantly involved or care about every dimension of the organization's operations. So accounting for this fragmented internal environmental in combination with the causal indeterminacy and the determinacy issue, we understand and we're that's what we're saying when we say that a hospital is a loosely coupled organization. Now just to be sure, though, being a loosely coupled organization isn't necessarily a bad thing. The literature has demonstrated that loosely coupled organizations are shown to be more flexible to their local environment as you can imagine. They're better protected from the spread of some level problems and they're more adapted to local phenomena. So it's not necessarily a bad thing, but in the case that Larry's referring to, with high reliability organizations, it's tough to drive a change across an entire system such as some of the health systems we're evaluating here at CHOT. As they're spread out across large metropolitan areas or even swathes of states in the case of a few of our members. And what we wanted to look at today was how exactly you would go about transitioning a looselycoupled organization into a more tightly-coupled organization. >> I've presented here the competitive classic idea an HRO in health care. This is from an article by Chassin and Loeb in 2011 in Health Affairs where they were applying this to safety cultures. And we're not talking about necessarily patient safety here, exclusively, certainly, but we're talking about what kinds of tools are essential to begin to tighten organizations a little bit more in terms of bringing management and professionals more closely together. And so the HRO, again, is at one end of the continuum. A totally loosely coupled is at the other end of the continuum. We want to move the needle a little bit closer to the HRO end. And so, leadership is mentioned almost in every innovation. It's all about leadership support, champions, and so forth. Culture is another issue. Culture of change, or a set of values, that will support whatever change you're trying to make. And certainly Studer Group has a number of cultural dimensions that it emphasizes. And then process improvement. The focus really is on improving processes and practices, changing the behavior. And so, it's not often times we talk about why you have to change attitudes and then you can change behavior. Well that's not necessarily so, as we know in social psychology that it really does require a focus on processes and behaviors. So Nick, you wanna talk about conceptual issues? >> Sure. So the key conceptual issues here, hope your're still with us, what we're basically looking at is, given the situation of the context with the hospitals that we were evaluating here. One, we wanted to know how do we reduce the loose coupling and its negative impact on organizational changes. And move it towards a more approximate health, or excuse me, high reliability organization. In the process of tightening the organization, if you're still following this analogy, it would basically improve the organization's responsiveness and internal accountability. Something that's lacking in the loosely-coupled organization that, in the case of Saint Luke's, is spread out over a large metropolitan area. And it's tough to implement one change somewhere and be sure that it's being followed at all six hospital locations. And then finally, how do we successfully implement the innovation to tighten the organization. However, as you can imagine, most interventions that want to attempt to tighten an organization, you can quickly and easily realize how that would be perceived as a threat to the autonomy of its end users. We'll get to some of the tools here specifically that were used in the intervention. However many of them, all of them, the goal of tightening the organization that can be perceived as prescriptive in nature. And again, they could be perceived as a threat to the autonomy. So how do you go about walking this fine line as managers between desiring to tighten the organization without frustrating the end user of the change initiative? So how we went about doing that. We basically broke this up into two parts. We wanted to first evaluate whether or not the intervention in this case Studer Group's evidence basic leadership had in fact achieved its goal of tightening the organization. So to get that first part, we interviewed 31 corporate, hospital, and unit leaders across six hospitals in a large metropolitan area there in St. Luke's in Houston. We asked them specifically about key support factors of EBL, the benefits of the evidence-based leadership implementation, some of the struggles they had along the way, and ultimately, did they see any change in outcomes. And ultimately, were they successful in tightening the organization? But then we wanted to examine this and analyze the innovation from the perspective of the end users as well, to determine okay, if it was successful, what were some of the things that the organization did correctly? And what were some nuances of the intervention itself that allowed the end users to agree to work in a more tightly-coupled organization, without necessarily losing autonomy, or having it be perceived that management was reducing their professional autonomy. So, with that, we used a specific model called the innovation implementation model developed by Klein and Sorra. I'll get into that later. But it basically looked at the amicable climate. Whether or not the management of the implementation established an amicable climate that increased the likelihood of it being successful. And then we also measured, with these nurses. We surveyed about 1,000 nurses across five hospital sites that were all medical surgery units. Nurses and we're asking them whether or not their perceptions about the climate during the implementation and also the innovation values fit. >> And this is the basic depiction of what we see in the Evidence-Based Leadership model from Studer Group. I've been using Studer Group, Hardwiring Excellence, and so forth, management courses, and emphasizing it for probably eight or so years. I've been researching this for a number of years. We have a couple of articles out already, a couple more in process, and a number of reports that we might talk about later if we have time. But the key thing that I see in this is really, going back to the hard stuff as the soft stuff, is that much of this is focused on practices that are easily understood. And labeled in ways that a wide range of professionals and staff at various levels of expertise can probably understand relatively easily. And these two spheres portrayed here on this graphic on the one side you have management and leadership and the other sphere on the right is more of staff-patient related practices. And in the middle are what I call linkage tools. And then there are feedback loops that connect all of these. And in a sense this depicts how we go about trying to create some of the conditions as we look at Studer Group model creating some of the conditions of a highly reliable organization. Because, in effect, you have practices on the clinical side that are, hopefully, reinforced by the clinical experiences that nurses are having with patients by doing hourly rounding and AIDET and so forth. And then, you also have on the management side, the leader evaluation management, kinda the goal alignment efforts on an ongoing basis up and down the hierarchy, so to speak, of the organization. You have the leadership development institutes. You have the monthly meetings with employees, the high, medium, low approach. And you could add recruitment, retention, a number of other things, to those management related tools. But these things really are designed to quotes, hardwire some of the management practices that then, in turn, reinforce the patient So we looked at these in more detail, I'm not gonna go over these word by word. But the leadership development institute is really set up to have quarterly meetings in a offsite location, involving lots of people, where the case of St. Luke's, it would bring together leaders and managers from all of these six hospitals to talk about student group and these practices that are being implemented. Leader evaluation manager, again, is trying to support automated performance evaluation of these middle level managers. Are they reinforcing these various student group practices? The monthly meeting model certainly encourages that kind of information. And then the high, medium low, as well is opportunity to rearrange your workforce to help support these things. On the other side, patient relationships, like the hourly rounding on patients discharge phone calls, and these are things that are, again, practices that we're, that student group is interested in hardwiring that will produce improved patient satisfaction. Will reduce readmissions that say through the discharge phone call. Through standardized shift reports and the like would also reduce the likelihood of errors in treatment of patients or miscommunication between oncoming and outgoing nurses. So those are the management practices and the staff and patient practices. And then finally you have those linkage practices that help connect the practices on the management side with the practices on the staff and patient side. The rounding on employees is critical, the rounding on internal customers, where you learn what's going on in other departments of course is highly relevant, and I guess what I would say here in concluding this description of linkages. A number of these things you see emphasized in other kinds of intervention. Like, whether it's improved management via process management, or lean or six sigma, but you also may see elements of this, certainly, in creating a safety culture or improving patient safety or using hospital required conditions. But what you see here in the student group model is bringing those all together. >> Right, so, again, this is getting back to the model we were referring to earlier, the framework that we use to evaluate how the nurses, the shape, the tool that we use to survey the nurses and gather their perceptions about how they received and perceived evidence based on relationship tools. So, the implementation of such innovation can fail as the result of a poor implementation, or a poor fit between the innovation and the organization standards and values. To incorporate each of these threats, developed an innovation implement model that you see here. The focus is on two antecedent conditions that must be met for an implementation to be successful, and further more, for the innovation to be effective. The first condition you see here is the presence of an amicable climate for implementation. And what we mean here with amicable climate is that the model's authors cite the need for adequate training and support, managerial feedback, HR support, and then overall user-friendliness of the innovation, in this case evidence-based leadership. For the purpose of this study, we were interested in evaluating from the nurses, 450, with satisfaction levels with EBL training, managerial feedback and support, leadership support and then ease of use of the EBL tools. Finally next with the innovation values fit basically what the model's arguing is that these the second condition that must be met is a minimum degree of fit between the innovation itself and the value of the values of the change recipient. So innovation values fit describes the extent to which targeted users perceive that the use of the innovation will foster, or conversely inhibit, the fulfillment of their values. A number of studies have confirmed positive associations between change recipients' emotional responses to a new innovation and the success of the implementation. So for the purpose of this study, we were interested in evaluating at the individual level. Again, this is the nurses that we surveyed. The proportion of change recipients whose values coalesce with evidenced-based leadership principles and tools. So, with that, we'll jump here to the results, starting off with the qualitative. >> And I should point out here that this research at Saint Luke's started about a year and a half ago. And we've wrote the interviews, and so these are some of the findings from the interviews with the 31 leaders. And number one, leadership, as we suggested earlier is strongly emphasized. And we saw the CEO of president being credited for initiating the evidenced-based leadership model. There were also, CEO and other corporate, and hospital leaders, were credited for support for the implementation, kind of managing the implementation. And the LDI Studer Group, the Leadership Development Institutes, was identified for creating a common identity across the hospitals. Also the other evidence based leadership tools, particularly the LEM and the some of the hourly rounding and AIDET, and so forth, were credited with standardizing practices across the hospital, so that if you went into one St. Luke's hospital, on one side of the city, you would experience the same thing as you'd gone into the hospital on the other of the city. And that also helped in terms of recruitment and retention, and the like. I point out that we interviewed and did this work at Saint Luke's after it'd been 30 months into the implementation of Studer Group. MEOSC on the other hand has been doing Studer Group for six years or so, and so we're collecting similar data from both organizations that I think will help us bring additional insights to this process. We're currently finishing a case study, where we're actually looking at the difference of importance in terms of the kind of tools at various stages that help with the implementation. >> All right so here are the quantitative results again. We created the survey based around two components, the amicable climates for the implementation and then whether or not the EBL tools, how they fit with the values of the nurses. So this first is looking at the amicable climate we asked five questions you can see here at the bottom, the first is where they provided with training, second how comfortable were they performing in these. Third was whether or not the manager provides regular feedback on the performance of these tools. Is it strongly supported by their manager? And is it strongly supported by hospital leadership? Here we see, we broke it down. We're only able to ask three of the tools Larry showed you in the graphic earlier, there's I think nine or ten different tools. But we're only able to ask three, to keep the survey short enough that they would actually complete it. But you can see here, each of these three columns. AIDET, again was one of the tools, the communication tool. Hourly rounding, and then discharge phone call. So we ask for all of these questions for both areas, we asked across those three tools. So as you can see here, though, there's a lot of blue on this screen. Obviously this was a Likert score, question that they answered with a either positive agreement, agreement, neutral, or disagreement, or strongly disagree. And then we then combine those into just three basic categories. You can see there's a lot of blue here. If we look at the sufficient Meaning every single one was above 65%, we think this one on discharge phone calls is actually an anomaly, a large number of nurses didn't, wouldn't have received discharge phone call training because not all units had individual nurses doing it. So we think this one column here is an anomaly so aside from this one. You can see almost 90% agreement that they received sufficient training. The comfort level in performing it, again you can see AIDET and hourly rounding, high levels of agreement that they are comfortable in doing it. Discharge phone calls we see a small dip, but again this is neutral, this isn't necessarily a bad disagreement, this is just saying they weren't comfortable. But again, this could be an anomaly in the sense that some nurses just don't like talking on the phone, or they didn't receive training so that they were just answering frankly. So, we like that we see a similar response here from discharge phone calls from question one to question two. Next we see the only one that only received around 60% agreement across all three tools, and that was the managerial feedback. Again, this isn't necessarily a bad thing. But, this was the lowest as far as agreement, but we see a lot of neutrals. And it did have the biggest number of disagreement, but again, less than 10% of the respondents disagreed across all three tools. Question four here, whether or not the EBL Tool was strongly supported by their manager. Again, we see high levels of agreement, and then finally, strongly supported by hospital leadership, we see almost no disagreement at all, how the nurses responded across all three tools. In general, we can see here that looking at the, again, getting back to our model of whether or not there was an amicable climate. A user friendly climate for the implementation of EBL. We see on the whole and we judge this to say yes, that there was. Next we will look at the innovation values fit and how the nurses responded to our questions for innovation values fit. For this construct we are looking at measuring the following five questions we asked them. They believe that and it was either AIDET, hourly or discharge phone calls. Whether or not it positively contributed to the overall quality of care. We asked all three schools whether or not they were positively contributing to the employee satisfaction of the unit and then we asked all three schools whether or not they had a positive impact on overall patient satisfaction. Again, here, we're looking for the quality of care, we did see agreement, so this of course is indicating that it did positively contribute. We see a slightly more uptick with hourly rounding that they think that may be that contributed more to quality of care than AIDET in discharge phone calls, however, still all three come in about 70% agreement. And then a large number of neutrals. Moving over to employee satisfaction, question two here, this is one where I like to say, we'll see with question three. I think we have a lot of selfless nurses here. We were very surprised by this. Not necessarily saying that these three contribute, you know, it's the least of all five questions that you can see here. But, in general, they're still saying that it did contribute positively towards employee satisfaction. Hourly rounding, AIDET, and discharge phone calls. Now keep in mind, all three of these tools. Again, getting back to the, we expressed a little concern that maybe these were going to be received by nurses as a threat to their autonomy because of their prescriptive nature. But you can see here, employee satisfaction. They're saying over 60, close to three-quarters of the respondents are saying, no in fact this has improved our levels of employee satisfaction. Question three here, when we get to patient satisfaction, this is getting back to my argument that we have a lot of selfless nurses here. Although they're not necessarily saying on question two, that this improved employee satisfaction, everyone is agreeing that AIDET, hourly rounding, discharge phone calls. More or less, it did improve patient satisfaction. So as you can imagine, they're saying the patients liked receiving, being greeted with this communication strategy that's prescribed by EDL. We often see the hourly rounding was very well-received, and the same goes for discharge phone calls. Finally, question four, we just sort of asked them point blank, are you glad your hospital is doing AIDET hourly rounding discharge phone calls? Again, high levels of agreement, close to three quarters, and then a small chunk of neutrals and then a very few people who disagree, that disagree with the hospital's decision to pursue it. And then, finally, the last question that we had for innovation values fit to determine the level of innovation values faced, or to assess it was to, we asked them the question, I find that my values are very similar to this organization. And again almost 90% responded in the affirmative. >> Okay, in conclusion we'll on time, as far as implementing change in care practices, you often hear hospital administrators or other nursing department heads and quality people saying we've gotta get on the same page. Got to get everybody on the same page, well in essence that's what we see here to some degree. We see that these tools are being used to help everybody get on the same page, use the same language, certainly leadership is reinforced early on, and the evidence based leadership tools are viewed as providing more structure. To what is done across the system and to creating a common culture and standardizing some practices. That's generally what the larger picture shows in our analysis and, of course, you've already just heard the discussion about the nurses and their response based upon the amicable climate for innovation and the innovation of values fed. Finally, the EDL is a well-thought-out set of tools, and an implementation process. It helps contribute to the change. In other words, we're not just trying to implement one or two things, or if we get this practice installed, we've done it, it's really more like a multi-project management. Each of these tools, in a sense is viewed as a project, an undertaking, that where the pieces all have to fit together. And so they address leadership and management processes, they address staff and patient care processes that we saw earlier, and also have tools that link these two sets of practices. And so, the upside coaching in a standardized implementation process is often mentioned as well when we did the interviews. And speaking of looking at the same page or addressing the same page, what we found, for example at Saint Luke's, was people talking about these tools in a very familiar way. At USC that's been doing it for six years or so, it was, almost everyone was talking about the tools as really standard practices and it was widespread throughout the organization. So I think we're seeing another pattern there, and I think some of the comparisons we can do across those sites will be interesting, so we'll stop there and ask for questions and comments. Okay. >> Any questions or comments? >> Oh, hi>> Hi, this is Kim>> Go ahead. This is Kim Myers. I thought you did a very, very, very good job. >> I'm sorry, I don't know, my phone is or something. But, the, I'll get the card. And I will send another email to Leah, and say, yes, we've walked in the back room. Thank you! Thanks. Yeah, I feel like, Karen what was interesting about that study which I noticed that hourly rounding, they felt that hourly rounding had a bigger effect on patient assessment. I don't know which one it was. Yeah maybe it was this one. Values that. And that when they did this survey we were just kind of rolling it out. So I would be interested to see if you did this again what would that, how some of this would change. It's just kind of fascinating to see that they do see the connection, which I think is good. >> If they saw the connection even despite the fact that yeah, maybe it didn't help out, these weren't negative responses. But yes, the fact that they, again I call them the selfless leaders because they're saying, no this isn't helping us, but it is helping the patient. Exactly. >> Right. Exactly. So sometimes I think we think they don't know the whys. They do. But, see, I think the reason why it wasn't a tie is because this is right when we were kind of starting to do the skill lab, and even though we were doing it, they hadn't really had the in yet. I just think it'd be interesting to see if this graph changed today if we did that, would it be different? Would it be less? Because now that we don't have the CHOT coaching here what is it sustaining is what I'm thinking? >> Yeah, no, and I think that will be interesting as well following up conducting the same survey to these individuals. Maybe a few more months out in advance and see how these two compare. >> We had a question, too, texted in, about should we have done the survey before it started and so forth to get a little clearer handle, particularly on the agreement with values of the organization and that sort of thing. And ideally, absolutely. We would like to do pre-post and the like, but we entered this at a later date. With some of the electronic medical record research we've done, we've had pre-post comparisons and that's extremely valuable. So, what we are seeing, though, and are gonna try to make the most of is, when comparing MUSC with St. Luke's, is to see the differences at different stages of implementation. We already are seeing at St. Luke's in our analysis of leadership responses, asking the leaders what were the most important factors at the beginning of getting started, what were the most important factors in managing the implementation on a day to day basis, and what were the most important factors in terms of sustaining it, or maybe factors that would account for the decline in success over time. So we were finding that different tools, in a sense, or made reference to at these different stages. We're really excited about that result and hope to have an article out on that very soon. >> So yes Dr. Smythe great question. Thanks for texting that in, but, yes, unfortunately given the you know we were allowed a snapshot only at one point in time. We'd love to be able to do this for an organization prospectively. >> We did talk with both St. Luke's and Studer Group about our interest in doing a follow up of this study next year, so we'd be looking at a five year period. And I think then we could at least, cuz part of the concern is here is sustainability and the challenge in a lot of organizations is not so much getting it going or even getting it going successfully, but again, how do you sustain it? How do you maintain the management support, the supervision, the leadership, and so forth that helped really recreate a culture that will bring this sustainable >> Any other questions? All right. Well with, okay? >> Since there's just a couple minutes left feel free to raise your hand and come in with questions. I just like to share some of my excitement about this line of work. This is, I think, a very good example of what I like to think of as programmatic research. As I said earlier, I've been thinking about Studer Group for probably nearly ten years, but about 2009, Josh Best and I published an article in Implementation Science where we looked at evidence based practice and research that would meet current standards of regarding evidence, excuse me, evidence and implementation of lien, implementation of six sigma, implementation of Studer Group. And we found very few articles in any of those areas. Surprisingly you'd think it'd be more and lean in six sigma but really not that many that you would have great confidence in methodologically. So that's helped guide our work and then secondly, Aaron Spaulding and some others of us wrote an article in 2010 in hospital topics where we looked at some of the management related elements of Studer Group, because I think a lot of focus was on the and hourly rounding and so forth, but the importance of the management side wasn't necessarily being presented in the literature. And then we have, this presentation now has been submitted to the Health Services Research Journal for publication. Then we have a case study for St. Luke's implementation coming out, and we've sent the first reports to MUSC based upon our work there. Finally, we're beginning analysis of the impact of discharge phone calls on readmissions at both MUSC and St. Luke's. So with the help of these organizations bringing together those data sets that will allow us to see the impact of discharge phone calls over time on readmissions. Nick, you want to add anything else? >> No I just wanted to comment Dr. Smythe, you pointed out that the deal was obviously the intervention leaders, the managers, it would be nice to know whether or not, here we demonstrated after the intervention that in fact there was a high level of innovation values fit. He brings up the point how do you know before implementing it whether or not there's going to be a high level of fit and that is a very expensive question that we would love to answer, presumably that you could answer prior to an intervention but hopefully the next project go around we can attack something like that. >> Let me comment just briefly because with MUSC we're working on an article from our first ground interviews there, where we asked them specifically questions about how Studer Group, to what extent, if any, has helped them leverage new projects or leverage other current projects, and the responses to that are pretty interesting. If I were to go beyond the data for just a moment, I would say what I think is happening is that, to some degree, those that have successfully implemented Studer Group may be creating more of a learning environment. A learning organization that maybe has more absorptive capacity, greater ability to take on additional innovations and maybe be more successful with them because they have a structural, a model for how to do that in a way that reaches effectively across the organization. >> All right with that, are there any last questions or comments? >> We thank all of you for. Oh go ahead. >> No, that's all right, I just thought that was an interesting point that Larry made about being a learning organization, that Studer was a learning organization. Did you mean that's just that they provide learning versus providing how to sustain? Is that what you meant by that comment? I'm not sure. >> Actually thank you for the request for clarification. Actually I was referring to it helps MUSC become a learning organization or it helps St. Luke’s become a learning organization, because they have created additional capacity by understanding how the pieces fit. These various management tools for reinforcement as well as the practice tools that are trying to be changed so that they have more familiarity and maybe even greater confidence. Other than some of these other innovations who are just taking one at a time without having had the Studer Group group experience. I'm not trying to for Studer Group. But those are some of the thoughts that I'm having. >> No, that's a good point, that they helped create that environment. So, okay. >> All right. Well thank you all very much for attending. Again we will be hosting at another announcement here, probably after the Christmas holiday, but we do have the next upcoming webinar will be by Dr. Eva Lee out of Georgia Tech on some readmissions work she's been doing. I'll send that out, but I look forward to hearing back some feedback from this webinar and we'll talk to you soon. Thanks. >> Thank you all. >> Thank you. >> Bye-bye. Hello?