Angiotensin-(1-7) intracerebroventricular administration generates
advertisement

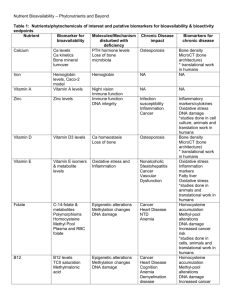
Angiotensin-(1-7) intracerebroventricular administration generates nociceptive effects in hot-plate task and decreased oxidative stress in the temporal lobe Received for publication, April 8, 2014 Accepted, July 5, 2014 OANA ARCAN1, WALTHER BILD1, ALIN CIOBICA2,3, DRAGOMIR NICOLAE SERBAN1*, DANIEL TIMOFTE1, VERONICA NASTASA1,3 1 “Gr. T. Popa” University of Medicine and Pharmacy, 16 Universitatii Street, 700115, Iasi, Romania 2 "Alexandru Ioan Cuza" University, Bd. Carol I, nr. 11, Iasi, 700506, Romania 3 Center of Biomedical Research of the Romanian Academy, Iasi Branch, Romania *Address correspondence to: “Gr. T. Popa” University of Medicine and Pharmacy, Universitatii 16, Department of Physiology, 700115, Iasi, Romania, Tel:+40741066769; E-mail: dnserban@yahoo.com Abstract Lately, there is increased evidence that besides the very well known angiotensin (Ang) II, other renin-angiotensin system (RAS) peptides, including Ang III, Ang IV or Ang-(1–7), could mediate important effects at the central level. Thus, very few aspects are known about the central actions of Ang-(1-7), while the effects of its administration alone on nociception were very rarely tested to date, according to the best of our knowledge. Thus, we were interested in studying the effects of Ang-(1-7) intracerebroventricular administration on nociceptive sensibility, as expressed by the main behavioral parameters in the hot-plate task, a fundamental behavioral tool for the study of pain in rodents, as well as the importance of Ang-(1-7) in the oxidative stress status from the temporal lobe, which is considered one of the most vulnerable brain regions to the oxidative status modifications. Thus, we report here for the first time upon our knowledge a possible nociceptive effect of Ang-(1-7) intracerebroventricular administration, as demonstrated by increased latency-time in the hot-plate task. Moreover, it seems that oxidative stress could be implicated in these aspects, since we found a significant correlation between the latency-time in the hot-plate and the levels of most of the oxidative stress markers from the temporal lobe (such as the glutathione peroxidase enzymatic specific activity or the levels of the main peroxidation marker malondialdehyde). Thus, our results could suggest new perspectives and studies regarding the possible usage of brain RAS in pain management. Still, additional studies are required in order to better understand the effects of Ang-(1-7) administration on nociception and oxidative stress status and also on the possible correlation that might exist between these two aspects. Keywords: angiotensin-(1-7), pain, oxidative stress. Introduction Lately, it is generally accepted that a separate renin–angiotensin system (RAS) exists in the brain, including all the precursors and enzymes required for the metabolism of the angiotensins [1,2]. Moreover, there is increased awareness regarding the fact that besides the well-known angiotensin (Ang) II, other angiotensin peptides such as Ang-(1–7) could mediate important central effects for the brain renin–angiotensin system, such as memory, learning, emotional functions or pain [3,4]. Thus, when it comes to Ang-(1–7), it has been previously demonstrated that it could counterbalance some pressor effects of Ang II [5,6]. Moreover, these effects were also observed when it comes to the superior functions level, as in the case of the long-term potentiation (LTP) process (which is believed to represent one of the most attractive models of memory/learning at the cellular level [7]), since it was demonstrated that Ang-(1–7) could stimulate LTP [8], while Ang II could inhibit it [9]. Also, while our group previously confirmed that brain RAS is implicated in pain processes and reported analgesic effects for Ang II central administration [10], to our knowledge, there are few studies -in fact only one previous report- connected with the role of Ang- (1–7) administration in the mechanisms of nociception, which was however focused on the specific Mas receptor in these processes [11]. In addition, it has also been suggested that RAS could exert important effects on the oxidative stress status. In this way, while our group has previously confirmed an increased central oxidative stress status as a result of Ang II intracerebroventricular (icv) administration [12,13], controversial data regarding the effects of Ang-(1–7) were previously reported, describing both pro-oxidant [14] and antioxidant actions [15,16]. Additionally, recent studies performed in both rodents and human patients stated a possible causal relationship between pain and oxidative stress. In this way, there are some preliminary data which reported that oxidative stress contributes to the reduction in peripheral vascular responses and the maintenance of thermal hyperalgesia in rats with chronic constriction injury [17], as well as those expressing a rat model of neuropathic pain [18] or capsaicin– induced mechanical secondary hyperalgesia in mice [19]. Also, increased levels of extracellular hydrogen peroxide were observed in the spinal trigeminal nucleus after formalin injection into rat, while this increase was also associated with pain behavior [20]. Thus, considering the previously mentioned aspects, in this paper we were interested in studying the effects of Ang-(1–7) intracerebroventricular administration on pain sensibility, as studied through some main behavioral parameters in the hot-plate task, as well as the importance of Ang-(1–7) in the oxidative stress status from the temporal lobe, which is most vulnerable cortical area to the effects of oxidative stress [21]. Moreover, we want to see if there is any correlation between the behavioral parameter which we used for the pain perception study and the levels of the main oxidative stress markers from the temporal lobe, as a result of central Ang-(1–7) administration. Material and methods Animals Adult male Wistar (n=20) rats, weighing 200–250 g and about 20 weeks of age, were housed in groups of four animals per cage and kept in a room with controlled temperature (22 0C) and a 12:12 h light/dark cycle (starting at 08:00 h), with food and water ad libitum. Rats were allowed to adapt to the experimental room conditions for one week before the beginning of the behavioral experiments. The animals were treated in accordance with the guidelines of animal bioethics from the Act on Animal Experimentation and Animal Health and Welfare Act from Romania and all procedures were in compliance with the European Communities Council Directive of 24 November 1986 (86/609/EEC). This study was approved by the local Ethics Committee and also efforts were made to minimize animal suffering and to reduce the number of animals used. Neurosurgery All surgical procedures were conducted under aseptic conditions, under sodium pentobarbital (45 mg/kg b.w., i.p., SIGMA) anesthesia. Rats were mounted in the stereotaxic apparatus with the nose oriented 110 below horizontal zero plane. Angiotensin- (1–7) (SIGMA) was icv administered (7 consecutive days, 0.1 mg/kg b.w.) by freehand through a plastic (silastic) cannula (Portex, 0.44 mm inside diameter, 0.9 mm outer diameter), stereotaxically implanted in the right lateral ventricle at the following coordinates: 0.5 mm posterior to bregma; 1.3 mm lateral to the midline; 4.3 mm ventral to the surface of the cortex. The cannula was positioned with acrylic dental cement and secured by one stainless steel screw. Ang-(1–7) was icv administered on a volume of 2 ml over a 1 min period. The shamoperated rats were injected with saline. There were no signs of distress during the procedure. Behavioral testing was done on the last day (7th) of the administration. Also, the location of the intracerebroventricular cannulas was verified by injecting a dye (Trypan Blue, SIGMA) through each cannula at the end of the experiment. In this way, after the end of experiments the brains were removed and the cannula placement was checked under light microscopy. Hot-plate The investigation of pain sensibility was performed using a hot-plate (Ugo Basile). A plastic cylinder is used to confine the rat to the heated surface of the plate which is maintained at 55 ˚C using a thermostate. The reaction time (the latency time) to two different types of behavior was monitored: licking the paw and jumping [10]. Tissue collection After the behavioral test, all rats were anesthetized, rapidly decapitated and the whole brain was removed. The temporal lobes were then collected. Each of the tissue samples was weighed and homogenized with a Potter Homogenizer coupled with Cole-Parmer Servodyne Mixer in bidistilled water (1 g tissue/10 ml bidistilled water). Samples were centrifuged for 15 min at 3000 rpm. Following centrifugation, the supernatant was separated and pipetted into tubes. Biochemical estimations Determination of superoxide dismutase Superoxide dismutase (SOD) activity was measured by the percentage reaction inhibition rate of enzyme with WST-1 substrate (a water soluble tetrazolium dye) and xanthine oxidase using a SOD Assay Kit (Fluka, product number: 19160) according to the manufacturer’s instructions. Each endpoint assay was monitored by absorbance at 450 nm (the absorbance wavelength for the colored product of WST-1 reaction with superoxide) after 20 min of as SOD activity units. Determination of glutathione peroxidase Glutathione peroxidase (GPX) activity was measured using the GPX cellular activity assay kit CGP-1 (Sigma Chemicals). This kit uses an indirect method, based on the oxidation of glutathione (GSH) to oxidized glutathione (GSSG) catalyzed by GPX, which is then coupled with recycling GSSG back to GSH utilizing glutathione reductase (GR) and NADPH. The decrease in NADPH at 340 nm during oxidation of NADPH to NADP is indicative of GPX activity. Determination of malondialdehyde Malondialdehyde (MDA) levels were determined by thiobarbituric acid reactive substances (TBARs) assay. 200 mL of supernatant was added and briefly mixed with 1 ml of trichloroacetic acid at 50%, 0.9 ml of Tris–HCl (pH 7.4) and 1 ml of thiobarbituric acid at s, samples were centrifuged at 3000 rpm for 10 min and supernatant read at 532 nm. The signal was read against an MDA standard curve and the results were expressed as nmol/mg protein. Total protein was measured using Bradford dye binding method, with bovine serum albumin as standard [22]. Statistics The animal’s behavior in the hot-plate task was statistically analyzed using one-way analysis of variance (one-way ANOVA). The results are expressed as mean ± SEM. F values for which P<0.05 were regarded as statistically significant. Pearson’s correlation coefficient and regression analysis were used to evaluate the connection between the latency time in the hotplate (as expressed in seconds) and the temporal lobe’s oxidative stress markers. Results Regarding the effects of Ang-(1–7) administration on pain sensibility, as studied in the hotplate task, we did find a significant decrease (F(1,18)=7, p=0.01) for the latency time to jump/licking paws, when compared to the control group (Figure 1). Figure 1. Effect of angiotensin-(1-7) on the latency time in hot-plate. The values are mean ± S.E.M. (n=10 animals per group). **p= 0.01 vs. control group. Moreover, we found significant correlations between the results of the behavioral task, represented by the latency time in the hot-plate (as expressed in seconds) and the levels of some oxidative stress markers from the temporal lobe, such as glutathione peroxidase (GPX) (n=20, r=–0.479, p=0.041) (Figure 2) and malondialdehyde (MDA) (n=20, r=0.575, p=0.025) (Figure 3). However, no significant correlations were found between the specific activity of superoxide dismutase (SOD) and the latency time in the hot-plate: n=20, r=0.238, p=0.313. Figure 2. Correlations between latency time in hot-plate vs. GPX. Figure 3. Correlations between latency time in hot-plate vs. MDA. Discussion Our results presented here describe a possible algesic effect of Ang-(1–7) central administration on rat, as shown by the significant decrease for the latency time to jump or lick the paws in the hot-plate behavioral task, a very well known and generally accepted behavioral tool used for the assessment of the pain sensibility. Moreover, we found a possible correlation between the behavioral marker we mentioned from the hot-plate task and the levels of some oxidative stress parameters from the temporal lobe, which is one of the most sensitive cortical areas to the effects of oxidative stress [21]. In general, very few things are known about the central actions of Ang-(1–7). As reminded, in the same way as in the vascular level (where it was cited to stimulated the nitric oxide and superoxide radical release from endothelial cells – [23]), it seems to exert opposite effects on Ang II, with some stimulatory effects on LTP process in the dentate gyrus [24] or the hippocampus [7]. To support this, it was also previously demonstrated that an Ang-(1–7) specific antagonist, called A-779, is blocking this LTP-stimulating effect of Ang-(1–7) [25]. Also, in the same context of the superior functions, in a study from 2012 we demonstrated that the central administration of Ang II would result in some analgesic-like effects in rats, which were also demonstrated through the usage of hot-plate task [10].Regarding our results described here, concerning the effects of Ang-(1–7) on nociception we demonstrated some nociceptive effects of Ang-(1–7) intracerebroventricular administration. In this way, this report is, to our knowledge, the first study describing its effects on pain perception, as studied through the hot-plate task, a very well recognized behavioral tool for the study of pain sensibility. However, there is a very recent study, published in 2012 by Costa et al. group, which actually demonstrated the opposite thing, by reporting an antinociceptive effect of Ang-(1–7), by the usage of a different test called the rat paw pressure test. Moreover, they showed that the aforementioned specific antagonist for the Mas receptor, called A-779, inhibited the described peripheral antinociception [11]. Additionally, the authors showed that naloxone was unable to inhibit the Ang-(1-7)antinociceptive effect, showing that opioid peptides is not involved in this responses and increasing in this way the relevance of RAS studies in pain modulation. As mentioned before, Costa et al. also reported that Mas receptor is an obligatory component in this matter. Still, it is now accepted that Mas may have additional ligands and that Ang-(1–7) may have additional receptors [8,25]. Thus, the data we are describing here could be very important considering that most of the previous studies regarding the modulation of pain processes were mostly focused only on the opioid peptides. In this way, this sort of results could support an integrative view regarding the modulation of nociceptive processes, with additional data regarding other neurochemical systems, such as the bioactive peptides of RAS [10,11]. Also, it seems that oxidative stress could be extremely relevant in these aspects, since in both the case of Ang II, which is generally known for exhibiting pro-oxidant actions [26], as well as now in the case of Ang-(1–7), we obtained significant correlations between the behavioral parameters of pain assessment [10] and the main markers of the oxidative stress status. In fact, when it comes to the previous studies about the effects of Ang-(1-7) on oxidative stress, the results are quite controversial, with reports stating that the pretreatment with Ang(1–7) can inhibit ischemia reperfusion-mediated oxidative stress by preventing the increase of MDA and lowering of SOD [16], as well as with opinions that Ang-(1-7) creates clear prooxidant actions, as expressed by reduced SOD and GPX specific activities and decreased glutathione levels [14]. As mentioned, in the present study we demonstrated significant correlations between the latency time in the hot-plate and the specific activity of GPX, as well as in the case of the latency time vs. MDA, as an important lipid peroxidation marker. Still, no correlations were found between the specific activity of SOD and the behavioral parameter which we determine in the hot-plate task. This could be perhaps a result of some compensatory mechanism that affected SOD activity, especially since it is known that SOD is the first enzyme in the way of the reactive oxygen species (ROS), catalyzing the conversion of superoxide radicals to hydrogen peroxide, which is then converted into water by GPX and catalase [27]. In this way, the connections that might appear between the nociceptive processes and oxidative stress status could represent an important aspect, which actually began to raise increased awareness in the current literature, since it was showed for example that the number of neurons exhibiting mitochondrial ROS production was significantly increased in the lumbar spinal dorsal horn of some specific models of neuropathic rats [28]. Additionally, it was demonstrated that SOD could exert some positive actions, as expressed in reduced inflammation markers and hyperalgesia after carrageenan injection into the rat paw [29]. Of course, all these aspects lead to discussions regarding the relevance of antioxidants administration in pain management. Thus, it was practically shown that the administration of some antioxidant-like substances, such as phenyl N-tert-butylnitrone and 4-hydroxy-2,2,6,6tetra methylpiperidine 1-oxyl could result in some important analgesic effects in both inflammatory [30] and neuropathic pain [31]. Still, as mentioned before, while it is becoming increasingly clear that oxidative stress status could be involved in nociception, the exact mechanisms by which this is contributing to pain are still unknown [10]. Conclusions We report here some possible nociceptive effects of Ang-(1–7) administration, as demonstrated by the decreased latency time in hot-plate task, a very well known and widely accepted behavioral task used for the assessment of pain sensibility. Moreover, we found a significant correlation between this behavioral parameter and the levels of some oxidative stress markers from the temporal lobe, which is considered to be the most vulnerable cortical area to oxidative stress modifications. However, further studies are necessary in order to elucidate the effects of Ang-(1–7) central administration on nociception and oxidative stress status and also on the possible relationship that might exist between them, although our results are clearly suggesting the relevance of brain RAS and its components in pain modulation and perception. References 1. O. VON BOHLEN UND HALBACH O, D. ALBRECHT, The CNS renin angiotensin system. Cell Tissue Res. 326, 599–616 (2006). 2. A. CIOBICA, W. BILD, L. HRITCU, I. HAULICA, Brain renin angiotensin system in cognitive function: pre-clinical findings and implications for prevention and treatment of dementia. Acta Neurol Belg. 109, 171–80 (2009). 3. M. MC KINLEY, A. ALBISTON, A. ALLEN, M. MATHAI, C. MAY, The brain renin-angiotensin system: location and physiological roles. International Journal of Biochemistry & Cell Biology 35, 901–918 (2003). 4. R. SANTOS, M. CAMPAGNOLE-SANTOS, S. ANDRADE, Angiotensin-(1–7): an update. Regulatory Peptides 91, 45–62 (2000). 5. E. TALLANT, C. FERRARIO, P. GALLAGHER, Angiotensin-(1–7) inhibits growth of cardiac myocytes through activation of the mas receptor. American Journal of Physiology—Heart and Circulatory Physiology 289, H1560–H1566 (2005). 6. R. MACHADO, R. SANTOS, S. ANDRADE, Opposing actions of angiotensins on angiogenesis. Life Sciences 66, 67–76 (2000). 7. C. HÖLSCHER, Long-term potentiation: a good model for learning and memory? Prog Neuropsychopharmacol Biol Psychiatry. 21, 47-68 (1997). 8. K. HELLNER, T. WALTHER, M. SCHUBERT, D. ALBRECHT, Angiotensin-(1-7) enhances LTP in the hippocampus through the G-protein-coupled receptor Mas. Molecular and Cellular Neuroscience. 29, 427–435 (2005). 9. D. ARMSTRONG, E. GARCIA, T. MA, B. QUINONES, M. WAYNER, Angiotensin II blockade of long-term potentiation at the perforant path-granule cell synapse in vitro. Peptides. 17, 689–693 (1996). 10. O. ARCAN, A. CIOBICA, W. BILD, L. HRITCU, D. COJOCARU, The effects of central angiotensin II and its specific blockers on nociception. Possible interactions with oxidative stress status. J Med Biochem. 32, 52–58 (2013). 11. A. COSTA, L. BECKER, E. MORAES, T. ROMERO, L. GUZZO, R. SANTOS, I. DUARTE, Angiotensin-(1-7) induces peripheral antinociception through mas receptor activation in an opioid-independent pathway. Pharmacology. 89, 137-44 (2012). 12. W. BILD, L. HRITCU, C. STEFANESCU, A. CIOBICA, Inhibition of central angiotensin II enhances memory function and reduces oxidative stress status in rat hippocampus. Progress in Neuropsychopharmacology & Biological Psychiatry. 43, 79–88 (2013). 13. A. CIOBICA, L. HRITCU, V. NASTASA, M. PADURARIU, W. BILD, Inhibition of central angiotensin converting enzyme exerts anxiolytic effects by decreasing brain oxidative stress. Journal of Medical Biochemistry. 30, 109–14 (2011). 14. S. GONZALES, G. NORIEGA, M. TOMARO, C. PENA, Angiotensin-(1–7) stimulates oxidative stress in rat kidney. Regulatory Peptides. 106, 67–70 (2002). 15. I. BENTER, M. YOUSIF, G. DHAUNSI, J. KAUR, C. CHAPPELL, D. DIZ, Angiotensin-(1–7) prevents activation of NADPH oxidase and renal vascular dysfunction in diabetic hypertensive rats. American Journal of Nephrology. 28, 25–33 (2008). 16. X. LIAO, R. GUO, H. MA, L. WANG, Z. CHEN, C. YANG C, J. FENG, Effects of angiotensin-(1–7) on oxidative stress and functional changes of isolated rat hearts induced by ischemia-reperfusion. Nan Fang Yi Ke Da Xue Xue Bao. 28, 1345–1348 (2008). 17. Z. KHALIL, T. LIU, R. HELME, Free radicals contribute to the reduction in peripheral vascular responses and the maintenance of thermal hyperalgesia in rats with chronic constriction injury. Pain. 79, 31–7 (1999). 18. H. KIM, S. PARK, J. ZHOU, G. TAGLIALATELA, K. CHUNG, R. COGGESHALL, ET AL, Reactive oxygen species (ROS) play an important role in a rat model of neuropathic pain. Pain. 111, 116–24 (2004). 19. E. SCHWARTZ, I. LEE, K. CHUNG, J. CHUNG, Oxidative stress in the spinal cord is an important contributor in capsaicin–induced mechanical secondary hyperalgesia in mice. Pain. 138, 514–24 (2008). 20. A. VIGGIANO, M. MONDA, A. VIGGIANO, D. VIGGIANO, E. VIGGIANO, M. CHIEFARI, ET AL., Trigeminal pain transmission requires reactive oxygen species production. Brain Res. 1050, 72–8 (2005). 21. E. KARELSON, N. BOGDANOVIC, A. GARLIND, B. WINBLAD, K. ZILMER, T. KULLISAAR, The cerebrocortical areas in normal brain aging and in Alzheimer’s disease: noticeable differences in the lipid peroxidation level and in antioxidant defense. Neurochem Res. 26, 353–361 (2001). 22. C. GURZU, V. ARTENIE, L. HRITCU, A. CIOBICA, Prenatal testosterone improves the spatial learning and memory by protein synthesis in different lobes of the brain in the male and female rat. Cent. Eur. J. Biol. 3, 39-47 (2008). 23. H. HEITSCH, S. BROVKOVYCH, T. MALINSKI, G. WIEMER, Angiotensin-(1-7)Stimulated Nitric Oxide and Superoxide Release From Endothelial Cells. Hypertension. 37, 72-76 (2001). 24. T. WALTHER, D. BALSCHUN, J. VOIGT, H. FINK, W. ZUSCHRATTER, Sustained long term potentiation and anxiety in mice lacking the Mas protooncogene. Journal of Biological Chemistry. 273, 11867–11873 (1998). 25. N. ALENINA, P. XU, B. RENTZSCH, E. PATKIN, M. BADER, Genetically altered animal models for Mas and angiotensin-(1–7). Experimental Physiology. 93, 528–537 (2008). 26. A. CIOBICA, V. BILD, L. HRITCU, M. PADURARIU, W. BILD, Effects of angiotensin II receptor antagonists on anxiety and some oxidative stress markers in rat. Central European Journal of Medicine. 6, 331-340 (2011). 27. H. SIES, Oxidative stress: oxidants and antioxidants. Exp Physiol. 82, 291-295 (1997). 28. E. PARK, X. GAO, J. CHUNG, K. CHUNG, Levels of mitochondrial reactive oxygen species increase in rat neuropathic spinal dorsal horn neurons. Neurosci Lett. 391, 108–11 (2006). 29. Z. WANG, F. PORRECA, S. CUZZOCREA, K. GALEN, R. LIGHTFOOT, E. MASINI, ET AL, A newly identified role for superoxide in inflammatory pain. J Pharmacol Exp Ther. 309, 869–78 (2004). 30. A. HACIMUFTUOGLU, C. HANDY, V. GOETTL, C. LIN, S. DANE, R. STEPHENS, Antioxidants attenuate multiple phases of formalin-induced nociceptive response in mice. Behav Brain Res. 173, 211–16 (2006). 31. M. TAL, A novel antioxidant alleviates heat hyperalgesia in rats with an experimental painful peripheral neuropathy. NeuroReport. 7, 1382–4 (1996).