BIOLOGICAL THERAPIES FOR DEPRESSION
advertisement

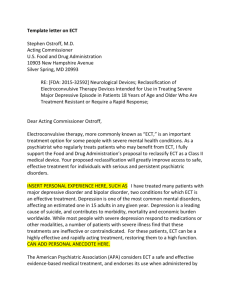
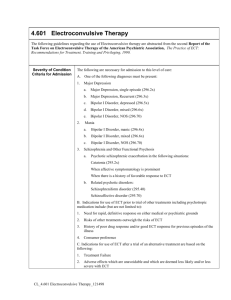
BIOLOGICAL THERAPIES FOR DEPRESSION To read up on the biological therapies for depression, refer to pages 451–459 of Eysenck’s A2 Level Psychology. Ask yourself If a biochemical imbalance is the cause of depression what would be the treatment? Should electroconvulsive therapy be used for depression? What do you think are the weaknesses of biological therapies? What you need to know DRUG THERAPY: MAJOR DEPRESSIVE DISORDER ELECTROCONVULSIVE THERAPY: MAJOR DEPRESSIVE DISORDER MAOIs Research evidence Tricyclics Evaluation Selective serotonin reuptake inhibitors (SSRIs) Evaluation Drug therapy: Major depressive disorder Individuals with major depressive disorder often have low levels of the neurotransmitters serotonin and noradrenaline, according to the monoamine theory. Accordingly, drugs to treat this disorder are designed to rectify these low levels. MAOIs The MAOIs block monoamine oxidase and by doing so help to prevent the destruction of noradrenaline. The increased noradrenaline activity leads to a reduction in depressive symptoms. The MAOIs are reasonably effective in reducing depression, but they do produce various side effects, such as blocking the production of monoamine oxidase in the liver, leading to the accumulation of tyramine. This is dangerous, because high levels of tyramine cause high blood pressure. Accordingly, depressed patients taking MAOIs have to follow a careful diet, making sure to avoid foods containing tyramine (e.g. cheese, bananas). Tricyclics Tricyclics slow down the re-absorption of serotonin and noradrenaline by the presynaptic vesicles. Consequently more of the neurotransmitters are left in the synapse, and so serotonin and noradrenaline activity increase at the postsynaptic receptors. This is linked to arousal and improved mood. The tricyclics are less dangerous than the MAOIs, but they can impair driving to a dangerous extent, and other side effects include dry mouth and constipation. Selective serotonin re-uptake inhibitors (SSRIs) The most common drugs used to treat depression are the serotonin re-uptake inhibitors (SSRIs), of which Prozac is the best known. These drugs are more selective in their functioning than the tricylics, in that they increase serotonin activity by blocking the re-uptake of serotonin, so leaving the serotonin to have an enhanced effect on the postsynaptic neuron without influencing other neurotransmitters such as noradrenaline. The SSRIs are as effective as the tricylics, but they possess some advantages. Depressed patients taking SSRIs are less likely to suffer from dry mouth and constipation than those taking tricyclics, and it is harder to overdose on SSRIs. However, SSRIs conflict with some other forms of medication, and Prozac is reported to have severe effects in some people, including suicidal thoughts where none were experienced previously. OVERALL EVALUATION OF ANTIDEPRESSANT DRUGS Effectiveness Empirical support for effectiveness. The MAOIs, the tricyclics, and the SSRIs have proved consistently effective in the treatment of major depressive disorder, but the tricylics are generally more effective than the MAOIs, and produce fewer side effects. Side effects. All three types of antidepressants have side effects. Do not work for all patients. It is not clear why the various drugs are ineffective with some patients. Compliance. There are problems of non-compliance (i.e. discontinuing mediation, disregarding instructions on dosage and timing) due to the side effects. However, this is not such an issue with SSRIs because there are fewer side effects, although it should be noted SSRIs have severe side effects in rare cases. Treats symptoms not causes. Treatments can either cure the processes causing the disorder (curative treatments) or suppress the symptoms of a disorder without changing the underlying processes (palliative treatments). Drug therapy for major depressive disorder is palliative rather than curative, and consequently there are high relapse rates when the drugs are stopped. Relapse rates. Hollon et al. (2005, see A2 Level Psychology page 453) studied three groups of patients over a continuation period of 12 months: (1) those who had received cognitive therapy but had no treatment during the continuation period; (2) those who had received drug therapy but had no treatment during the continuation period; and (3) those who had received drug therapy and continued to receive drug therapy throughout the continuation period. Of those withdrawn from cognitive therapy, 31% suffered a relapse, 47% of those who received drug therapy throughout relapsed, and 76% of those withdrawn from drug therapy suffered a relapse. These findings strongly suggest that drug therapy is mainly a palliative treatment whereas cognitive therapy is a curative treatment. Thus, drug therapy is effective only for as long as depressed patients continue to take medication, as without it relapse rates are high. Drugs work less well with those who have already been treated with drug treatment. Leykin et al. (2007, see A2 Level Psychology page 454) found the recovery rate in patients treated with the selective serotonin reuptake inhibitor paroxetine was nearly 60% among those who had never received drug therapy before but was under 20% among those who had received drug therapy for depression twice or more in the past. This compares unfavourably to cognitive therapy because approximately 40% of patients who had received drug therapy before recovered when given cognitive therapy. This suggests that it is not just that those with persistent depression are harder to treat but that once the biochemical systems have been affected by drugs then subsequent drug therapy has less impact. Placebo effect. The placebo effect occurs when patients given an inactive substance or placebo (e.g. a salt tablet) show significant reductions in their symptoms. It is difficult to know how much any improvement is due to the drug and how much to the placebo effect, i.e. the patient improves because they expect the drug to work. Appropriateness Individual differences. About 30% of patients fail to respond to any given drug or show only very modest beneficial effects, therefore drug therapy is not effective for all, although often patients who do not respond to one drug do respond to a different one. Lack understanding of their effect. We do not fully understand how the antidepressants reduce the symptoms of depression. It is not as simple as drugs increasing neurotransmitter levels, because they do this almost instantly, but can take a few weeks to have an effect. Some would argue we shouldn’t use them if we do not fully understand how they work. Palliative not curative. Antidepressants treat symptoms not causes and so don’t cure depression. Compare unfavourably to cognitive treatment. The fact that patients treated with cognitive therapy have lower relapse rates, particularly if they have been treated with drugs on more than one occasion, suggests that cognitive therapy may be more appropriate than drug therapy, particularly given that cognitive therapy is far less invasive as it does not have the side effects of drug therapy. Electroconvulsive therapy: Major depressive disorder Electroconvulsive therapy (ECT) was based on the observation that epileptics did not have schizophrenia and so it was concluded that the two disorders were antagonistic (cannot not have one if have the other). This led to the deduction that inducing seizures could help treat schizophrenia and this was done initially using drugs such as camphor and then cardiazol. It was then discovered that electric shocks could produce seizures and that ECT had better outcomes than cardiazol. ECT was then used for other mental disorders such as depression. ECT involves passing an electric current through the head to produce brain seizures. It used to be a dangerous process and result in patient terror and broken bones because traditionally no anti-anxiety drugs were used so the whole body would be in seizure. The modern use of ECT has a number of improvements including muscle relaxants to minimise the convulsions and the use of anaesthetics so that the patient is asleep during the treatment and so does not experience the same anxiety. In addition, bilateral ECT (administering ECT to both brain hemispheres) has been mainly replaced by unilateral ECT (applying it only to the non-dominant hemisphere) to reduce any memory loss. Studies designed to assess the effectiveness of ECT often compare it against simulated ECT, in which patients are exposed to the equipment and believe falsely that they have received ECT. This is done to ensure that the beneficial effects of ECT are genuine and not simply a placebo effect—seeing the equipment and believing that you are receiving shocks might be enough to reduce symptoms in the absence of any actual shocks. RESEARCH EVIDENCE FOR ECT Janicak et al. (1985, see A2 Level Psychology page 455) found that 80% of all severely depressed patients responded well to ECT, compared with 64% given drug therapy. ECT is also often the treatment of choice in the case of patients with very severe depression when rapid reduction in symptoms is especially important. This can be essential in cases of severe depression in which suicide attempts are possible. Petrides et al. (2001, see A2 Level Psychology page 455) reported that between 65% and 85% of depressed patients had a favourable response to ECT. Pagnin et al. (2004, see A2 Level Psychology page 455) carried out a metaanalysis which concluded that ECT was more effective in the treatment of depression than antidepressants or simulated ECT. EVALUATION OF ECT Effectiveness ECT is highly effective. Certain patients benefit more from ECT than others. De Vreede, Burger, and van Vliet (2005, see A2 Level Psychology page 456) identified four patient factors predicting good response to ECT: age above 65 years, the absence of a psychotic depression (involving more severe symptoms), the absence of a personality disorder, and responding well to antidepressants. ECT is used when drug treatment fails. ECT can be an effective treatment when patients have been unresponsive to drug treatment. Treats symptoms not causes. ECT reduces the symptoms of depression; it does not produce a cure. Thus, it is a palliative rather than a curative treatment. Appropriateness ECT is consistent with the biological basis of depression. Some of the symptoms of depression seem to involve deficient functioning within the brain, and so a form of treatment that alters brain functioning may well prove to be appropriate. Side effects. Memory loss, other cognitive impairments, and possible neurological damage do question the appropriateness of the treatment. However, this must be balanced against the fact most side effects are relatively short lasting. Memory loss is not permanent. The American Psychiatric Association and the British National Institute for Health and Clinical Excellence have both concluded that ECT does not cause permanent brain damage. We do not understand how it works. Some would argue that because we do not understand how it works then we should not use the treatment. This is the equivalent of hitting a computer to make it work, we have no idea what the true effects are. Ethical issues. Issues of protection and informed consent are raised because most patients dislike receiving ECT, and some might be put under excessive pressure to become involved in this form of therapy. Historically it was used as a form of punishment and to exert control over patients. Reductionism. ECT only focuses on one level—the biological, and so ignores the psychological approach to treatment. Dosage. ECT is generally most effective at reducing symptoms when given to both hemispheres at a high dose. However, this produces the most severe side effects. Thus, therapists have to strike a delicate balance between effectiveness on the one hand and unwanted side effects on the other. Individual differences. De Vreede et al.’s (2005) research shows ECT works better for some than for others. So what does this mean? We have considered two forms of biological therapy for depression, drugs and ECT. Both have been assessed in terms of effectiveness and appropriateness and this leads to the conclusion that tricyclic drugs are generally better than MAOIs because they have fewer side effects. SSRIs may be better again as they are harder to overdose, have fewer side effects, and so help resolve the issue of non-compliance, but unfortunately they do have severe side effects in some case as they have been reported to cause suicidal thoughts where there were none previously. Thus, all biological treatments raise issues of appropriateness such as side effects, individual differences, and the fact they treat the symptoms not the causes, which leads to a high relapse rate. This last criticism is a key weakness as this makes biological treatments palliative because they manage the disorder rather than cure it and so we need to consider if psychological treatments offer more hope of a cure. Evidence suggests that this is the case as drugs have been compared negatively to cognitive therapy. Over to you (a) Outline one or more biological therapy(ies) for depression. (9 marks) (b) Evaluate the therapy(ies) described in (a). (16 marks)