MenonetallReviewFinalRevised2 track

1
2
Human and pathogen factors associated with Chlamydia
trachomatis-related infertility in women
3
4
5 Menon S.
1
, Timms P.
1,2
, Allan J. A.
6 M.
8,9
, Hocking J.
10
, Huston W. M.
1
3,4
, Alexander K.
1
, Rombauts L.
5
, Horner P.
67
, Keltz
7 1. Institute of Health and Biomedical Innovation, 60 Musk Ave, Q Block, Queensland
8 University of Technology, Kelvin Grove, QLD, 4059, Australia.
9 2. Faculty of Science, Health, Education and Engineering, University of the Sunshine Coast,
10 Maroochydore, QLD, 4558, Australia.
11 3. Wesley and St Andrews Research Institute, The Wesley Hospital, Auchenflower, QLD,
12 4066, Australia.
13 4. UC Health Clinical School, The Wesley Hospital, Auchenflower, QLD, 4066.
14 5. MIMR-PH Institute of Medical Research, Monash, VIC, Australia, Australia
15 6. School of Social and Community Medicine, University of Bristol, Bristol, UK
16 7. Bristol Sexual Health Centre, University Hospital Bristol NHS Foundation Trust, Bristol,
17 UK
18 8. WESTMED Reproductive Services, New York, USA
19 9. Icahn School of Medicine at Mt Sinai Hospital, New York, USA
1
20 10. Centre for Epidemiology and Biostatistics, Melbourne School of Population and Global
21 Health, University of Melbourne, Carlton South, VIC, Australia
22
23 Correspondence: Wilhelmina (Willa) Huston, Institute of Health and Biomedical
24 Innovation, School of Biomedical Sciences, Queensland University of Technology, 60 Musk
25 Ave, Kelvin Grove, QLD, 4059, Brisbane, Australia. Tel: +61 7 31386258; email:
26 w.huston@qut.edu.au
27
2
28
Table of contents
29
Introduction 5
30
The evidence for the association of Chlamydia with infertility
31
Proposed models for the development of infertility following …..
6
32
C. trachomatis infection in women
11
33 Ascension
34 Persistence
35 Cellular paradigm
36 cHSP60 induced delayed hypersensitivity
37
Host/human factors associated with chlamydial infertility in women 17
12
13
15
16
38 Repeat infection and infertility
39 Do co-infections or the microbiome play a role in chlamydial pathology?
40 Sexual behaviour and age of sexual contact
41 Hormonal status at time of infection
42 Human genotypic factors associated with C. trachomatis infertility in women
17
19
43
Immune responses associated with Chlamydia trachomatis in women 25
20
21
22
44 Immune responses from reproductive sites and tissues
45 Immune responses in peripheral blood mononuclear cells (PBMC) in women
3
25
28
46 Immune pathway elucidated by in vitro culture models
47 Conclusions
29
30
48
Chlamydial factors that may influence the development of pathology 31
49 Chlamydial serovar can associate with repeat infection and symptoms that….
50 may link to a propensity to cause pathology and infertility
51 Chlamydial genotypes can mediate tissue tropism and may be a factor …..
52 in pathology development
53
Conclusions
31
32
33
54
55
References
Authors Bios
35
57
56
57
58
59
4
60
Introduction
61 Chlamydia (C.) trachomatis is one of the most common bacterial sexually transmitted
62 infections (STI) worldwide, with WHO’s most recent estimates indicating approximately 100
63
million new infections annually (1), and in the United States of America alone,
64 approximately 2.86 million Chlamydia
infections occurred in 2008 (2). The infection can
65 result in serious reproductive consequences, including pelvic inflammatory diseases (PID),
66 ectopic pregnancy, and infertility in women. Infertilty is defined as the inability to have a
67 healthly live baby after 12 months of unprotected timed intercourse. The majority of studies
68 reviewed for this document state their definition of infertility as inability to achieve
69 successful pregnancy as greater than 12 months. C. trachomatis is a Gram negative, obligate
70
intracellular bacterial pathogen with a unique biphasic developmental cycle (3). The
71 organism has been characterised using biology and genomics as a highly evolved or ancient
72 pathogen with evidence of a reduced genome that is tailored for the obligate intracellular
73
human niche (4). This unique intracellular niche has meant that until recent times, the
74 organism has not been investigated using molecular microbial methods, however, animal
75 models have been used to demonstrate Koch’s postulates in relation to infection and
76 reproductive pathology (with all the hallmarks of pathology including presence of Th1-like
77 cytokines, fibrosis, mononuclear infiltrates and lymphoid follicle formation), with more
78
extensive pathology reported after repeat infections (recently reviewed, (5)). Apari
et al
79 recently proposed the appealing but somewhat controversial and untested hypothesis that the
80 ability to cause infertility may actually be a specialised and evolved trait of STI pathogens
81 (such as Chlamydia and Neisseria ). This infertility was proposed to result in increased sexual
82 promiscuity of the host in the seeking of fecundity, thus enabling enhanced transmission and
83
positive selection of those strains of the pathogen that cause infertility (6).
84
5
85 In spite of the considerable worldwide burden of chlamydial disease it is still not known what
86 the host and pathogen determinants are that result in infertility. We have chosen to
87 specifically focus on infertility in women. WHY do review now wh insert We have used
88 PUBMED searches and reading of the relevant literature to find and review the evidence
89 (focussing on direct human evidence) and to identify the gaps in our knowledge that may be
90 addressed in future to further advance our understanding of the risk factors that could predict
91 or determine infertility outcomes in women.
92
93
The evidence for the association of Chlamydia with infertility
94 Genital Chlamydia infection is asymptomatic in over 70% of cases and as a result there are
95
few population-based prevalence or incidence estimates available (7). Available population-
96 based data from the USA, Australia, and UK suggest that between 3 and 5% of under 30
97 years of age will have Chlamydia
at any point in time (8-12). Estimates of the incidence of
98 disease sequelae (specifically pelvic inflammatory disease, ectopic pregnancy and infertility
99 in women) are lacking, largely because there are very few natural history studies of
100 Chlamydia infections in humans. Although a continuous-time Markov model analysing
101 existing evidence from randomised control trials and observational studies estimated the
102 probability of PID from a chlamydial infection was 0.16 (95% credible interval: 0.06-0.25)
103
(13). These studies that have been conducted are typically limited to the relatively short time
104 frame between diagnosis and treatment, which may not capture the true occurrence of
105
pathology and reproductive consequences (14, 15). Generally, there are two main ways in
106 which clinicians and scientists characterise or associate chlamydial infection with infertility
107 or other infection sequelae. The first is based on longitudinal information that includes
108 infection (cervical), upper reproductive tract symptoms resulting in pelvic inflammatory
6
109 disease (typically symptomatic and detected) and subsequent infertility (specifically tubal
110
infertility) (14, 15). The second is a retrospective approach based on women presenting with
111 tubal damage or unexplained infertility combined with evidence of chlamydial infection
112 history either by medical history review for previous diagnosed infection, history of PID, or
113
serological assessment to indicate previous infection history (16). Current infection with
114 Chlamydia also prevents conception, although this is also the case in males which may
115
confound this data (17). However, this infertility may be a consequence of local response to
116 the active infection and not necessarily indicate permanent reproductive damage; therefore
117 this review will not cover this form of infertility.
118 Infertility is defined by the world health organisation as ‘a disease of the reproductive system
119
120 that is defined by the failure to achieve a clinical pregnancy after 12 months or more of regular unprotected sexual intercourse’, and this is the definition we have used for the
121 purpose of this review. Some studies refer to sub-fertility which is defined as reduced fertility
122 with a prolonged time of unwanted non-conception and we consider this compatible with the
123 definition of infertility for the purpose of this review. Pelvic inflammatory disease (PID) and
124 ectopic pregnancy are also reviewed here, with ectopic pregnancy defined as tubal
125 development of the embryo. Chlamydial infertility typically is detected some years after the
126 infection and so the gold standard NAATs used for active infection diagnosis are not useful
127 in these cases.
128 A systematic review attempting to establish the attributable risk of infertility among women
129 following a genital Chlamydia infection concluded that there is currently not sufficient
130
longitudinal evidence to accurately determine this risk (18). However, there is robust
131 evidence that women who have experienced PID are more likely to develop infertility, and
132 robust evidence for Chlamydia causing PID. One large longitudinal cohort study was
133 conducted by Westrom et al.
(19) to evaluate PID and fertility outcomes. The study followed
7
134 1844 women with abnormal laparoscopic findings upon suspicion of acute PID (cases) (not
135 limited to Chlamydia ) and 657 women who had normal findings (controls). Follow up
136 identified that upon attempting to fall pregnant 16.5% of the cases and 2.7% of the controls
137
failing to conceive (19). Further investigations demonstrated that 141 (10.8%) of the PID
138
cases and none of the controls had developed tubal factor infertility (19). In addition, the
139 ectopic pregnancy rate was also higher in the PID cases, with 9.1% ectopic pregnancy in
140
cases and 1.4% in the controls (19). However, this study did not detail the infectious agent
141 underling the initial PID.
142 A review of studies characterising the risk of sequelae direct from chlamydial infection by
143 Haggerty et al . (2010) reported that PID rates after untreated chlamydial infection (typically
144 in the short time between diagnosis and treatment) found that in ‘high-risk’ settings 2-5% of
145
women developed PID, but this may be lower in an asymptomatic population (20). However,
146 in a randomised controlled trial to evaluate if chlamydial screening can prevent pelvic
147 inflammatory disease (POPI trial), it was identified that the risk of PID after chlamydial
148 infection in a one year time frame was 9.5% (95% CI 4.7%-18.3%) compared to 1.6%
149
women who had not tested positive at baseline during the trial (21). In a population wide
150 retrospective medical chart review approach in Sweden, it was identified that women who
151 had a positive test for Chlamydia (n=2965) had an adjusted odds ratio of 1.27 (95% CI 1.04 -
152 1.55, P<0.0001) of having had treatment for PID compared to women who tested Chlamydia
153
negative (n=2853) (16). Mathematical modelling suggested that PID can occur at any time
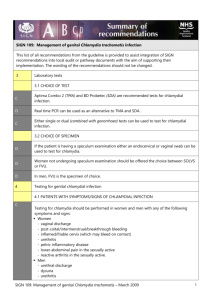
154 point during the natural history of infection, therefore annual chlamydial screening programs
155
may reduce the incidence of PID (22), although a separate model concluded that it is unclear
156 if there is a different risk of PID earlier or later in the infection, but that annual screening
157
could prevent 61% (95% credible interval 55-67) of chlamydial associated PID (13).
8
158 The use of medical record review to retrospectively identify previous diagnosed chlamydial
159 genital infection in women who present with infertility is rare. However, in the same
160 previously mentioned study in Sweden using a retrospective hospital record review process, it
161 was identified that women who had a positive Chlamydia test had an adjusted hazards ratio of
162 1.31 (95% confidence 1.09-1.57, P<0.0001) of having infertility compared to women who
163 tested negative for Chlamydia , although there was no significant difference in ectopic
164
pregnancy outcomes (16). Therefore, at least based on these limited studies, a relatively small
165 proportion of women, who are diagnosed with the infection develop infertility.
166 Much of the evidence of the association between Chlamydia and infertility comes from
167 studies that have used Chlamydia serology to determine previous history of chlamydial
168 infection. The studies typically find a significant association with either the presence of or
169 higher titres of chlamydial antibodies in women who have tubal pathology compared to
170 women who have other forms of infertility. Serology prediction of a past history of
171 chlamydial infection relies on the accuracy of the test. The serological tests are
172 microimmunoflourescence or ELISA (enzyme linked immunosorbant based assay) based
173 tests.
174 There have been attempts to evaluate the performance of these tests by comparing them on
175 the same participants. Using this approach one study found that the pELISA MEDAC was the
176 best of three ELISAs (compared with Savyon and Labsystems) for detection of tubal
177 pathology in infertile women at a fertility treatment clinic with 55% sensitivity and 87%
178
specificity (23). The same study compared two MIF tests (n=315, with 51 tubal pathology
179 cases) reported that with a cut-off titre of 1/64 the Biomerieux test had 71% sensitivity and
180 74% specificity, compared to 47% sensitivity and 95% specificity for the Labsystems test
181
(23). A meta-analysis conducted in 2011 compared MIF and several ELISA and found that
182 MIF had the highest accuracy (area under the curve) for detection of tubal pathology
9
183
P<0.001, and P=0.01 (for bilateral occlusion) (24). However, in the absence of a longitudinal
184 cohort of participant’s directly linking diagnosed active chlamydial infection with subsequent
185 tubal infertility and detectable serological responses it is difficult to assess the accuracy of
186 these tests.
187
188 Regardless of test performance, numerous studies have identified a correlation of Chlamydia
189 serology positivity ( Chlamydia antibody testing: CAT) with diagnosed tubal factor infertility
190 (typically using a case:control design of tubal infertility compared to other causes of
191 infertility). These studies include the following: a significantly higher percentage of women
192 with tubal pathology were CAT positive (50.2%, n=141) compared to infertile for other
193
reasons (29.6%, n= 326, p<0.001) using microimmunoflourescence (MIF) (25). In a separate
194 study high CAT titres using MIF correlated with presence of tubal damage n=434 compared
195
to all women with infertility n=1006 (p<0.001), as did pelvic adhesions (26). Another study
196 reported CAT (MIF) was 74% sensitive and 93% specific for detection of tubal disease (total
197
210 patients) p<0.001 (27). In contrast, in Rwanda infertile participants that had a high
198 proportion of tubal pathology (185 of 303 infertile participants), however, when CAT was
199 conducted using several ELISA kits compared to fertile post-natal controls (n=312) the
200 sensitivity and specificity of three different chlamydial ELISA were poor for tubal pathology,
201 suggesting that Chlamydia
is not a major cause of tubal pathology in this population (28).The
202 MEDAC pELISA (MOMP peptides) in the Netherlands was able to predict tubal disease in
203 infertile women (n=40 CAT positive, compared to n=167 CAT negative) with a sensitivity of
204
0.37 (95% CI: 0.26-0.49) and specificity of 0.88 (95% CI 0.82-0.92) (29).
Chlamydia heat
205 shock protein 60 (cHSP60) ELISA detection of CAT was reported to detect women with
206 Chlamydia -associated tubal infertility (n= 72) with a sensitivity and specificity of 81.3%, and
207 97.5% respectively. However, these women were first tested by laparoscopy for tubal damage
10
208 and for a positive result in the MIF serological assay to assign case group before testing the
209
ELISA so this study has likely over-reported the test performance (30). In a subsequent study
210 of a further 77 participants this group further reported that cHSP60 antibodies were 92%
211
specific and 44% sensitive for tubal factor infertility (31). cHSP60 ELISA positivity was also
212 found to be significantly more frequent in women with tubal factor (n=88) compared to
213 controls of infertile women with other know factors for infertility or healthy blood donors
214
(n=163) (43.2% vs 13.5%) in a study conducted in Helsinki (32).
215 A prospective observational study at a reproductive health centre in New York used MIF
216 serological prediction of previous C. trachomatis infection to compare with infertility
217 diagnosis and treatment outcomes. A total of 1279 participants were screened and 70 (5.5%)
218 were positive for C. trachomatis
(33). Of those selected for investigation of tubal disease
219 sero-positive women were significantly more likely to have hysterosalpingography detected
220 tubal blockage (37.5% compared to 10.1%; P= 0.001) or laparoscopically diagnosed tubal
221
damage (85.7% compared to 48.9%, P= 0.002) (33). Sero-positive women also had 57% less
222 pregnancy rates than sero-negative women prior to IVF but once IVF treatment commenced
223
they were equally likely to conceive by IVF as women with other causes of infertility (33). A
224 mathematical model, including a number of assumptions, and adjusting for serology test
225 sensitivity and specificity estimated that 45% of tubal factor infertility episodes are likely to
226 be attributable to C. trachomatis
(CI: 28-62%) (34). Combined, these studies provide
227 substantial evidence that a past history of chlamydial infection is significantly associated with
228 tubal pathology and infertility in women, regardless of serological assay performance.
229 However, they do not allow us to determine how frequently this tubal infertility is an
230 outcome of primary infection, and therefore the attributable risk of Chlamydia for infertility
231 is not known.
232
11
233
Proposed models for the development of infertility following C. trachomatis
234
infection in women
235 We describe what we consider to be the four models that are most commonly referred to
236 within the field to explain the process that underlies the development of infertility following
237 Chlamydia infection. The models are not exclusive of each other and there is evidence for
238 and against each model. We will briefly summarise these models so that the host and
239 pathogen data that we present later can be considered in the context of each model (Fig. 1.).
240
241 Ascension
242 This model suggests that the infection ascends to the upper reproductive tract in only some
243 women, and this ascension is usually typified by the presence of symptoms, development of
244 PID and if unchecked consequent development of tubal pathology. There is considerable
245 direct evidence that the chlamydial infection can ascend beyond the cervix, however, the
246 proportion of cases in which this ascension occurs is unknown. Evidence for ascension
247 includes the following studies; Chlamydia DNA has been detected in salpingectomy
248 specimens from one woman with ectopic pregnancy, and from several endometrial and cervix
249 specimens from women with subsequent ectopic pregnancy although not in their ectopic
250
C. trachomatis DNA was detected in tubal specimens from
251
women with ectopic pregnancy in Myamar (36).
C. trachomatis DNA was detected in
252 endometrium, fallopian tube and ovaries of as many as 56% of women with ectopic
253
pregnancy or tubal factor infertility (37).
C. trachomatis organism presence was associated
254
with endometritis (plasma cell influx in the endometrium) (38, 39). A small study in the UK
255 identified the presence of C. trachomatis in the upper genital tract from 4 out of 10 women all
256 of whom had no symptoms suggesting that is it possible to have asymptomatic ascension and
12
257
that ascension may not occur in all women (40). This ascension model is also supported by
258 substantial evidence of chlamydial inducing a pathological immune response in human cell
259 and tissues (discussed later) and is mutually inclusive with the Persistence and/or Cellular
260 Paradigm models. However, there is only limited evidence to support that; 1. Ascension of
261 the infection occurs in some but not all women or that; 2. that lower genital tract symptoms
262 and/or signs typify upper reproductive infection because mucopurulent cervicitis and other
263 cervical/genital symptoms/signs have been reported in both the presence and absence of
264 upper reproductive tract symptoms or with laparoscopic evidence of salpingitis (ascending
265
However, it is important to note that in the field it is generally agreed
266 that upper genital tract infection does not happen in the absence of cervicitis/lower genital
267 tract signs of inflammation, and these were included in the diagnostic criteria from both the
268
Westrom and PEACH PID studies (19, 43).
269 It seems possible or even likely that ascension may be independently moderated by numerous
270 other factors that could explain the low frequency of pathology development, supporting that
271 it only occurs in some women. These moderating factors could include host factors such as
272 cycle stage or hormone status at time of infection, as chlamydial or gonococcal endometritis
273
was found to be more likely to be detected in women in the proliferative phase (44). Equally
274 important moderating factors could include immune status, genotypic factors, other co-
275 infections, or reproductive tract microbiome composition. Unfortunately, there is no
276 published evidence on these factors and direct evidence of ascension or not. Furthermore,
277 pathogen factors could also moderate the likelihood of ascension such as infectious burden
278 (although chlamydial serovar alone has not been able to be significantly associated with
279
pathogenic potential or clinical manifestations (41)).
280
13
281
282
283 Persistence
284 Chlamydia persistence, or the presence of viable but non-culturable chlamydial organisms,
285 develops in response to adverse conditions, and can remain dormant but present for
286
considerable lengths of time (reviewed (45)). Persistence
in vivo has been proposed as a
287 model where this on-going presence of the organism may drive a long-term pathological
288 immune response resulting in the tissue damage to the fallopian tube (certainly the high
289 expression of the dominant antigen cHSP60 has been detected in laboratory persistence
290
models) (reviewed, (46)). This is a difficult model to test
in vivo , although it was recently
291 attempted by Arsovic et al ., 2014 who defined patients with a persistent infection as those
292 who had IgG and/or IgA MOMP (MEDAC pELISA) and IgG cHSP60 seropositivity, patients
293 who had IgG or IgA with no cHSP60 IgG were defined as recent or past chlamydial infection
294
and sero-negative for all three were considered negatives (47). However, this study included
295 a spontaneous miscarriage group for comparison which is arguably likely highly distinct from
296 tubal infertility and did not include groups with other causes of infertility nor fertile controls,
297 nor recent diagnosed chlamydial infected participants. There are studies that have presented
298 evidence of C. trachomatis DNA or antigens being present in the tubal material of women
299 with tubal infertility or ectopic pregnancy or salpingitis, supporting that organism persistence
300
301 in some form occurs in vivo
(37, 48-50). Recently, morphologies consistent with laboratory
models of persistence were observed in endocervix samples associated with IFN-
, further
302 supporting the likely in vivo
relevance of laboratory models of persistence (51). It is difficult
303 to determine if chlamydial persistence has always occurred leading to pathology. Persistent
304 infection may resolve at any time after pathology develops and prior to detection, given the
14
305 difficulties in specimen collection from the upper genital tract the evidence is reasonably
306 compelling that chlamydial persistence (either consistent with the lab models or a distinct in
307 vivo form) could be a relevant factor in pathology. It is important to highlight a recent review
308
309 that suggested that some forms of persistence may be ‘colonisation’ and in fact not associated
with ‘pathogenesis’ and disease (52). Our suggestion is that perhaps the two are distinct and
310 there is pathology associated persistence (given the evidence reviewed here) and separate
311 cases of non-damaging colonisation. Specifically, the evidence that 1. chlamydial persistence
312 is induced by a range of conditions in vitro
(reviewed, (45, 46)), and 2. persistence like
313 morphology and/or chlamydial antigen/DNA detection in the absence of active infection has
314 been observed in clinical samples, leads us to feel confident to suggest that persistence may
315 be a relevant physiological status in vivo particularly in the case of ascension to the upper
316 reproductive tract tissues, and therefore likely a determinant of pathological outcome from
317 infection.
318
319 Cellular paradigm
320 The cellular paradigm model proposes that the chlamydial infected epithelium or
321 endothelium immediately responds to the presence of the Chlamydia or specific antigens
322 from Chlamydia in a pro-inflammatory manner, typified by pro-inflammatory cytokines and
323 growth factors which in turn induces a pro-inflammatory secondary immune cell activation
324 and migration to form a local lymphoid follicle resulting in cell damage and fibrosis or
325
scarring (comprehensively presented and reviewed elsewhere (53)). This model is widely
326 supported by the published evidence of human epithelia and immune cell responses to
327 Chlamydia and a primary tissue ex vivo model that is discussed in more detail later in this
328 review. This model also presumes that chlamydial ascension is associated with pathology and
15
329 also mutually allows for persistence of Chlamydia
in the upper reproductive tract (53). A
330 pathological adaptive memory response proposed as the secondary component of this model
331 is also supported by the existing data that repeat infections increase the likelihood of
332
pathological outcomes in women (54), and by numerous immunological results (discussed
333 later in this review).
334
335 cHSP60 induced delayed hypersensitivity
336 There has been considerable focus on a pathology model that involves delayed
337 hypersensitivity and/or molecular mimicry in response to specific chlamydial antigens
338
(reviewed (55)). This model has largely resulted from a body of literature demonstrating high
339 titre human antibody response to cHSP60 in participants with tubal pathology and
340 additionally that in several animal models tissue pathology developed after repeated
341
inoculations with cHSP60 protein (reviewed (53)). However, this model is subject to
342 considerable controversy due to; inconsistencies between the different published findings;
343 problems with protein preparations that involved a hypersensitive detergent being used in
344 some animal models; and cross reactivity or poor specificity for some of the antibody tests
345
(56-62). On the other hand there is no doubt that cHSP60 is a predominant chlamydial
346 antigen that does frequently elicit an immune response, and is likely a major antigenic
347 contributor to the pathology development. Furthermore, in human trachoma cases it is
348 frequently possible to observe ongoing follicles present and disease pathology in the absence
349 of PCR detectable Chlamydia suggesting that there is continuing immune activity in the
350
absence of organism during pathology development (63).
351 Interestingly, one group proposed that cHSP60 antibodies detected in the follicular fluid of
352 female IVF patients may induce early destruction of the embryo by cross reacting against
16
353
embryo human HSP60 and result in lower transfer success (64). They observed a 74.1%
354 cHSP60 sero-positivity in women without embryo implantation (n=47) and 47.9% sero-
355 positivity in women with successful embryo implantation (n=91) (p=0.0004). However, this
356 observation directly contradicts a finding in separate and much larger study (n=1279) that
357 cumulative IVF cycle pregnancy rates are the same for women who are chlamydial
358
seropositive compared to those who are seronegative (33). A study in France also
359 contradicted the possible role of adverse embryo implantation impact of anti-chlamydial
360 immunity as it that for found for both men and women with PCR or serological evidence of
361 Chlamydia (n=52) the IVF pregnancy rate and semen characteristics were not different
362
compared to controls that were negative for chlamydial testing (n=119) (65).
363
364
Host/human factors associated with chlamydial infertility in women
365 Repeat infection and infertility
366 Repeat infection represents a substantial proportion of chlamydial infections detected
367
annually (re-infection review; (66)). It is likely that these repeat infections are made up of
368
reinfection, treatment failure, and persistent infections (14). Batteiger
et al ., (2010) conducted
369 a longitudinal cohort of 210 adolescent women (14-17 years old) participants (USA) and
370
identified that 121 experienced a repeat infection (14). In a longitudinal cohort in Australia,
371 1116 women (16-25 year old) were followed, and 14 re-infections were observed from a total
372 of 81 women who were at risk of repeat infection (three of these had two episodes of re-
373
infection) (cumulative risk over 12 months of 20.3%, 95% CI 13.2-37.6%) (67). Interestingly,
374 in this study in Australia organism load was lower in re-infections compared to prevalent
375
infections detected at the study baseline (67), but there were no associations between
376
participant characteristics and re-infection (67) (although this was possibly a statistical power
17
377 issue). However, careful consideration into study design is needed when evaluating repeat
378 infection, the Batteiger and Walker studies tested quarterly for Chlamydia , and PCR may
379 detect residual DNA from dead organisms causing a false positive. A study conducted in
380 Vancouver, showed that the repeat infection occurred in 8 of 42 participants in a longitudinal
381 study (both genders) indicating a cumulative incidence of 29% (95% CI 12-46%), although
382
the study was confounded by re-testing immediately conducted in some participants (68). A
383 study in the UK showed re-infection was 29.9 (19.7-45.4) per 100 person years from a GP
384
clinic setting (69). Infection and repeat infection significantly associates with sexual
385 behaviour risk factors as we would expect, such as new partners or failure to use condoms
386
(67). These repeat infection rates appear to be higher than the reported infertility outcome
387 rates in women who have had a positive Chlamydia test in the Low et al ., (2006)
388
retrospective cohort study (16), suggesting that repeat infection alone is not the sole
389 determinant of infertility or pathology. However, there is some evidence to suggest that
390 repeat infection increases the risk of developing infertility. A retrospective cohort study by
391 Hillis and co-workers in Wisconsin examined the risks of hospitalisation for ectopic
392 pregnancy or PID in 11000 Wisconsin women who had one or more chlamydial infections.
393 They identified elevated risks of ectopic pregnancy in women who had two (OR 2.1 95% CI
394
1.3-3.4), and three or more infections (OR 4.5 95% CI 1.8-5.3) (54). Pelvic inflammatory
395 disease risk was also increased for women who had two (OR 4.0 95% CI 1.6 - 9.9) and three
396
or more chlamydial infections (OR 6.4 95% CI 2.2-18.4) (54). Therefore, repeat infection is
397 likely to be a significant contributing factor in at least some cases of chlamydial infertility.
398 Treatment failures or persistence induced by antibiotics have also been proposed to be
399
contributing to repeat infection rates (reviewed (70)). Batteiger
et al
400 infections in 13.7% of the patients were due to possible or probable treatment failures.
401 Additionally , in vitro studies have shown that azithromycin induces chlamydial persistence
18
402
(71). Therefore, treatment failure or persistence (presenting as treatment failure) could be a
403 contributing factor to development of infertility in some women via all four of the proposed
404 pathology models.
405 The rise of repeat infections detected over time has resulted in the proposal that increased
406 public health investment into chlamydial screening and treatment is preventing the
407
development of natural immunity to the infection (arrested immunity hypothesis) (72, 73).
408 Furthermore, the authors propose that these repeat infections may be the source of
409 pathological sequelae that may not occur in women who have a protective immunity from a
410
naturally resolved infection (72, 73).
411
412 Do co-infections or the microbiome play a role in chlamydial pathology?
413 Co-infections with other STIs are not uncommon, for example 46% of female patients
414 positive for N. gonorrhoeae were also be positive for Chlamydia in a family planning clinic
415
in the USA (74). However, a serology study in Zimbabwe, demonstrated that women with
416 antibodies to either C. trachomatis of N. gonorrhoeae were significantly more at risk of
417 having PID, ectopic pregnancy, or abnormal fallopian tubes than those women with
418
antibodies to both pathogens (75), suggesting that it is not necessary to have had infection
419 with both pathogens to result in reproductive pathology. Patients with bacterial vaginosis who
420 were a recent contact of a male with chlamydial urethritis had an odds ratio of 3.4 (95 % CI
421 1.5-7.8) to test positive for chlamydial infection. The presence of H
2
O
2
producing lactobacilli
422 in the vagina were protective against acquisition of infection (odds ratio 0.4, 95% CI 0.2-0.8)
423
in vitro model was used to demonstrate that it is actually the acid or pH
424
lowering impact of the lactobacilli that confers the anti-chlamydial activity (77). It has been
425 hypothesized that indole producing organisms that increase in the microbiome during or
19
426 subsequent to bacterial vaginosis enable C. trachomatis to synthesize tryptophan from indole
427
(78), consequently evading the activity of interferon gamma at the infected site and thus may
428
facilitate the infection (78, 79). Bacterial vaginosis during
C. trachomatis or N. gonorrhoeae
429 infection was recently found to be associated with risk of PID, although the authors conclude
430 that difficult to determine if the bacteria underlying the vaginosis facilitated ascension and
431 PID caused by the STIs or alternatively if the bacteria responsible for vaginosis cause the PID
432
(80). Clearly, there is increased chlamydial infection risk associated with co-infection or
433 bacterial vaginosis, and also evidence for an association with PID, supporting that co-
434 infections could therefore result in an increased likelihood of development of infertility.
435
436 Sexual behaviour and age of sexual contact
437 Age is a risk factor for pelvic inflammatory disease, and in most studies generally PID is
438 typically significantly associated with increasing age, whereas younger women tend to have
439 the highest chlamydial infection incidence. Age is also a risk factor in likelihood of
440
contracting chlamydial infection (12, 81). Cross national studies from 1999-2008 in
441 Denmark, Australia and Sweden showed that increasing PID rates were associated with
442 increasing age, with the exception of New Zealand, where the rates were higher in women of
443
ages 15-19 (82). The highest incidence of
C. trachomatis infection is in women of ages 16-24
444
(83). Consistent with these studies, being under 20, having cervical symptoms were all risk
445 factors for endocervical chlamydial infection in women, and the organism burden was also
446
higher in younger women when measured by viable culture counts (84). Potentially the
447 organism burden may influence the ability to ascend to the upper reproductive tract and
448 ability to maintain a longer or persistent infection, therefore even though there is no direct
20
449 evidence, there seems to be the potential for younger age of acquisition of chlamydial
450 infection to increase the risk of pathological outcomes.
451
452 Sexual behaviour (new partners or higher number of partners) is often significantly associated
453 with increased risk of C. trachomatis
infection (9, 85). As shown in the study by Skjeldestad
454 et al
., 2009 (86) , where there was a 37% probability of a woman acquiring
C. trachomatis
455 infection if she has had 3 more partners within 42 months. A younger age at first coitus,
456 higher number of sexual partners, and self-reported history of medically diagnosed sexually
457 transmitted infection were all significantly associated with tubal infertility compared to fertile
458
controls (p<0.01) (87). However, as these are also known to be significant factors for
459 increased likelihood of acquisition of chlamydial infection it is not certain if they directly
460 influence the likelihood of pathology outcomes from the infection.
461
462 Hormonal status at time of infection
463 Oral contraceptive use was found to be a risk factor for C. trachomatis infection (p=0.006),
464
and the organism burden was found to be higher in oral contraceptive users (p<0.001) (84).
465 Prospective recruitment of young female participants (>17) attending genitourinary medicine
466 clinics in the UK identified that those who had a Chlamydia infection were also more likely
467
to have elevated progesterone concentrations (p=0.05) (88). In contrast, oral contraceptive
468 usage has been linked to protection against subsequent infertility or conception problems by
469
two different studies (19, 89). However, it would be extremely difficult to link hormone
470 status at time of infection with subsequent pathological outcomes such as infertility, even in a
21
471 longitudinal study, given the high numbers of oral contraceptive users, and the independent
472 importance of these factors in the risk of acquiring an infection.
473
474
475 Human genotypic factors associated with C. trachomatis infertility in women
476 The development of C. trachomatis related infertility in only some women may be a
477
consequence of a genotypic pre-disposition (reviewed comprehensively (90)). These studies
478 are described below; however, for the sake of brevity we have documented the sample sizes,
479 statistics and details of the alleles in table format (Table 1). Note the above mentioned
480 comprehensive review of this topic has recently been published therefore we have been brief
481
482 Toll-like receptors (TLRs) recognize and bind to antigens of pathogen, and signal to
483 upregulate an immune response. There are 10 Toll like receptors (TLR) identified in the
484
human body, and TLR 1-4 expressed in the female genital tract (91). TLR2 and TLR4 are
485 also expressed on macrophages, dendritic cells and epithelial cells and they bind chlamydial
486
lipopolysaccharide (92). In a prospective genotypic study with female participants attending a
487 sexual health clinic and a fertility clinic in Amsterdam, Karimi et al
488 demonstrated a possible protective role of a TLR2 haplotype. The haplotype consisting of
489 two distinct single nucleotide polymorphisms (SNPS) was found to be present in a
490 significantly higher proportion of women with a history of Chlamydia who did not have tubal
491 pathology and in sexual health clinic attendees was present in a higher proportion of women
492
who were asymptomatic (93). In the PEACH PID study TLR1 and TLR4 polymorphisms
493
were found to significantly associate with chlamydial PID (94), whilst SNPS from TLR2
22
494 (different SNPs from those included in the Karimi study), TLR6, Myd88, and TIRAP did not
495
significantly associate with chlamydial PID (94).
496
Den Hartog et al (95) identified that the risk of tubal pathology was higher in
C. trachomatis
497 IgG positive women with multiple TLR polymorphisms. The study also showed a trend
498 towards association of various individual polymorphisms in TLR9 and TLR4 with increased
499 risk of tubal pathology in C. trachomatis
IgG positive women (95). However, the small
500 sample size in the study makes it difficult to draw a correlation between the polymorphisms
501 and level of risk for female infertility.
502
503
NLRP3, a component of the inflammasome that activates a pro-inflammatory response has been identified to have polymorphisms reported to result in altered IL-1
secretion (a pro-
504
inflammatory cytokine) (96). Several NLRP3 polymorphisms were tested in women
505 prospectively recruited at a sexual health clinic and fertility clinics in Amsterdam, women
506 heterozygous or homozygous with the one of the NLRP3 polymorphisms were at significant
507 risk of developing abdominal pain during C. trachomatis
508 Mannose-binding lectin (MBL) is a pro-inflammatory protein that activates complement and
509
is locally synthesised in the vagina (97). MBL and MBL promoter polymorphisms have been
510
previously demonstrated to alter the levels of MBL produced (97). It was identified that
511 women with tubal factor infertility who were chlamydial sero-positive more frequently had
512
the low MBL producing genotypes compared to healthy controls (97). However, this was not
513 the case in an ectopic pregnancy group who were less likely to have the MBL-deficient
514
genotypes (97). This later finding sheds some doubt on the role of MBL genotypes, given that
515 it seems unlikely that the pathology associate with ectopic pregnancy is distinct from tubal
516 infertility.
23
517 Human leukocyte antigen (HLA) class II molecules (DR, DQ and DP) present peptides to
518 CD4 T cells and induce adaptive immunity. DQ polymorphisms were more frequent in
519 women with tubal infertility who were also C. trachomatis
sero-positive (98).Whilst another
520 polymorphism was negatively associated with C. trachomatis
positive tubal infertility (98).
521 Wang et al
., (99) showed that in adolescent females with recurrent chlamydial infections,
522 certain HLA polymorphisms were significantly associated with recurrent infections. A recent
523 study attempted to link different immune genotypes to immunological outcome by testing a
524 functional role for HLA DQ alleles combined with an IL-10 allele for both frequency in a
525 tubal factor infertility ( Chlamydia positive) cohort compared to controls and also for
526
lymphocyte proliferative response to cHSP60 (100). The HLA alleles and IL-10 allele were
527 more frequently identified in the chlamydial tubal factor cohort compared to the control,
528
529 however the lymphocyte proliferation in response to cHSP60 was not significantly different
in relation to the alleles (100). However, in a different study, distinct IL-10 and IFN-
530 polymorphisms were found to significantly impact on lymphocyte proliferation in response to
531
532
533
534
535
A range of cytokine polymorphisms have been shown to significantly associate with women with C. trachomatis
tubal infertility, including: IL-10 (102), TNF-
Polymorphism in IL-1
and receptor genes were not associated with C. trachomatis related
536 tubal pathology
(104). Adolescent females with recurrent chlamydial infections had a lower
537
frequency of three IL-10 promoter polymorphisms (99). Eng
et al
538 CD14 allele (TLR-4 co-receptor) was associated with increased TNF-α production when
539 whole blood was stimulated with C. trachomatis and C. pneumoniae
24
540 Whilst none of these studies were able to account for all chlamydial tubal infertility cases, it
541 is a convincing body of evidence that human genotype may be a factor in pathology
542 development. It is interesting that to date the vast majority of studies have focussed on
543 immune factors, yet as an obligate intracellular pathogen Chlamydia has key host nutritional
544 requirements, inclusion vacuole requirements, and therefore the ability to ascend and cause
545 pathology may in fact be independently determined by a as yet unknown non-immune host
546 genotype.
547
548
Immune responses associated with Chlamydia trachomatis in women
549 Insight into the immunological factors that may be involved in C. trachomatis infertility in
550 women has been obtained through various human studies, including; local secretions
551 (cervical and vaginal lavages), human tissues, peripheral blood mononuclear cells (PBMC),
552 as well as through in vitro cell culture models. The innate response to infection is clearly
553 critical for the infection outcome, and as outlined in the cellular paradigm model, could be
554 the major determinant of either a pathological or resolution outcome from the infection. A
555 commonly used framework to categorize the adaptive immune response is the Th1:Th2
556
paradigm (reviewed (107)). This paradigm suggests that the immune response can polarize
557 towards a cytotoxic pathological response (Th1) or a humoral antibody mediated response
558 (Th2). The profiles of these responses include Th1 subset of T helper lymphocytes (Th) and
559 cytokine production such as: IL-2, IL-6, tumor necrosis factor (TNF-α), and interferon-
560
gamma (IFN-γ)(108, 109); and Th2 responses involve IL-4, IL-5, IL-6, IL-10 and IL-13
561
(108). In addition to Th1:Th2 regulatory immune profiles typified by IL-17 or IL-23 have
562
also recently been described (reviewed (110)). Here we summarize the existing evidence for
25
563 the human immune response against C. trachomatis and how this evidence fits the four
564 different models of infertility development using these immune categories.
565
566 Immune responses from reproductive sites and tissues
567 Genital secretions have been used to reveal the immunological responses that occur at the site
568 of infection, although it is not possible to link these with subsequent pathology. IFN-γ levels
569 were found to be five times higher in the endocervical secretions of women with C.
570 trachomatis infection detected by culture (n=47) compared to uninfected women (n=52)
571
(111). Analysis of immune factors using multiplex immunoassay in cervical-vaginal lavages
572 of women attending a STD clinic with acute C. trachomatis infection (n=5) compared to
573 controls with no infections (n=13), revealed significantly higher levels of IL-1β, lactoferrin,
574
575
TNF-α, IL-8, VEGF, G-CSF, IL-10, IL-3, IL-7, IL-12 and IL-6 (112). However, in a separate
study in India IFN-
levels were only significantly higher in women with recurrent C .
576 trachomatis infections compared to controls but not higher than those with primary infection
577
(113). IL-17 and IL-22 were 5 times and 3 times higher in the cervical secretion of
C.
578 trachomatis
positive women (n= 27) compared to negative controls (n=17) (114). IgG and
579 IgA antibodies to C. trachomatis EBs were higher in the cervical washes of C. trachomatis
580
positive fertile women during primary infection compared to recurrent infection (113).
581 However, cervical IgG to specific chlamydial antigens (cHSP60 and cHSP10) was higher in
582 recurrent infection than compared to primary infection, which is what would be expected
583
584
(113). Flow cytometric analysis of lymphocytes present at the cervix of
C. trachomatis infected women identified the increased presence of a unique cell type;
4
7+CLA+memory
585
T cells (115). Stimulation of cervical monocytes with chlamydial EBs showed an increased
586 expression of Toll-like receptors (TLRs) TLR2 and 4, and both receptors were also found to
26
587
588 be expressed at higher levels in cervical cells from women with infection compared to
uninfected women (116). The levels of IL-1
, IL-4, IL-5, IL-6 and IL-10 were reported to be
589 significantly higher from enriched cervical T cells stimulated with chlamydial inclusion
590 membrane (Inc) proteins from C. trachomatis related infertile women (n=18) as compared to
591 C. trachomatis
positive fertile women (n=14) (117). Whilst not always a
Chlamydia related
592 pathology, a study by Balasubramaniam et al ., (2012) that found that level of cytokines IL-8
593 and IL-6 were significantly upregulated in the fallopian tube immediately in the location of
594
595 implantation of ectopic pregnancy, but not in the fallopian tubes of women undergoing
benign hysterectomy (118). A very recent study identified that differences in IFN-
levels
596 correlated with differences in the chlamydial cellular morphologies at the cervix when
597
comparing two patients (51). These local responses all support that immune mediated
598 pathology and key chlamydial antigens are likely involved in the development of infertility,
599 although they are not directly correlated to the fallopian tube.
600
601 The effects of chlamydial infection in human tissue ex vivo studies provided a controlled
602 insight into the cellular responses that likely occur in vivo during the immediate primary
603 infection. Though ex vivo
fallopian tube studies, Hvid et al. (119) showed that addition of IL-
604 1RA receptor antagonists, blocked IL-1 and IL-8 production preventing the pathology from
605
chlamydial infection (119). This confirms that IL-1 along with IL-8 are likely major factors
606
for tubal pathology (119), supporting the cellular paradigm of pathology development and not
607 supporting the hypersensitivity model. Furthermore, implicating the innate immune response
608 as a possible determinant of infection outcome. Fallopian tube explants from ectopic
609 pregnancy cases that were C. trachomatis sero-positive were used to demonstrate that C.
610 trachomatis
induced higher expression of a prokineticin receptor via TLR2 binding (120).
27
611 The prokineticin pathway impacts on smooth muscle contraction and intrauterine
612 implantation as well as angiogenesis, which may imply a mechanism for C. trachomatis
613
damage leading to ectopic pregnancy (120). T lymphocytes from endometrial and salpingeal
614
615 tissues cultured ex vivo in the presence of Chlamydia or cHSP60 showed induction of lymphocyte proliferation and IFN-
secretion from PID or ectopic pregnancy cases (121). In
616 the same participants, higher levels of IFN-γ mRNA expression and lower levels of IL-5 in
617 fallopian tube and peritoneal cavity specimens of PID patients who had T cells proliferating
618 in response to the organism ex vivo further implicated Th1 cytokine production in C.
619 trachomatis
related pathology (121). Primary endocervical cell cultures infected with
C.
620
621 trachomatis also demonstrated a pro-inflammatory cytokine response with abundant production of IL-8, IL-1
and TNF
, all of which were maximally detected during live
622
infection with active bacterial protein synthesis (122). These primary endocervical cultures
623 indicate that the innate immune response to Chlamydia is typically pro-inflammatory, which
624 is what may be required to successfully resolve the infection. Combined these data
625 predominantly support the cellular paradigm and ascending infection models of pathology
626 and link to a Th1 profile of immunity. However, given that a cytotoxic response is needed to
627 resolve infection, differentiating between a successful Th1 profile resolving infection, and
628 one that results in tissue damage is not possible in the absence of longitudinal data..
629
630 Immune responses in peripheral blood mononuclear cells (PBMC) in women
631 Peripheral blood mononuclear cells (PBMC) are often used to provide insight into immune
632 cell responses to Chlamydia from different participant cohorts. PBMC proliferation induced
633 by purified C. trachomatis EBs showed a prominent secretion of IFN-γ in women with
634
genital infection (123). PBMC from women at high risk of acquiring an infection were
28
635 stimulated with cHSP60 and the production of IFN-
strongly correlated with protection
636 against incident C. trachomatis
infection (124). In a separate study PBMC from healthy
637 donors were incubated with C. trachomatis serovar K, leading to the finding that pro-
638
639
640 inflammatory gene expression (measured by microarray and validated by qRT-PCR) was sustained for up to seven days, especially for IFN-
, and IL-2receptor
separate study, cHSP60 PBMC production of IFN-
was lower in women with PID or repeat
641
infections compared to women with current infections (126, 127). Human dendritic cells
642
643 prepared from human PBMC were infected with C. trachomatis serovar E or L2 that induced production of IL-1
, IL-6, IL-8, IL-12p70, IL-18 and TNF-α (128). A separate study also
644 detected production of IL-12 and TNF-α by human PBMC sourced dendritic cells infected
645 with C. trachomatis
et al
. (130), showed that stimulation of PBMC with
646 chlamydial EBs elicited IFN-γ production by natural killer cells. Cohen et al
647 IFN-γ production from PBMC stimulated with cHSP60 correlated with participants who were
648 protected from acquisition of infection in a longitudinal study of 143 female participants
649
(124). This study also showed the PBMC production of IL-13 in response to chlamydial EBs
650
also correlated with a reduced risk of infection (124). Our own research has demonstrated IL-
651 6 production from endometrial and endocervical primary ex vivo cultures from live infections
652 with C. trachomatis
653
654 Immune pathway elucidated by in vitro culture models
655 Epithelial cell culture are most commonly used for in vitro growth and characterisation for C.
656 trachomatis
C. trachomatis infection in HeLA, SiHa (human cervical
657
658 carcinoma epithelial cell) and HEp2 (human epithelial cell) were used to demonstrate that IL-
1α regulated IL-8 production from these cell lines during infection (133). Similarly, mRNA
29
659 measurement of cytokine expression after C. trachomatis infection of HeLa, SiHa cervix
660 squamous carcinoma cells and HT-29 colon adenocarcinoma cells showed increased levels of
661 IL-8, GROα, GM-CSF, IL-6 and IL-1α levels. These cytokines are potent chemoattractants,
662
activators of neutrophils, monocytes and T lymphocytes (134).
A HeLa/THP-1 co-culture
663
664 model attempting to re-capitulate the in vivo cellular cross talk also identified sustained IL-6 and IL-8 cytokine secretion during C. trachomatis infection with IL-1
transiently detected
665
(135). IL-6 and IL-8 were also detected in a separate study using infections of cervical and
666
epithelial cell models (122). A HeLa and THP-1 (mono-nuclear cell) co-cultures model
667 identified that there are distinct profiles of innate immune responses to C. trachomatis
668
669 serovar E compared to L2. The results also showed that the monocyte released innate cytokines (such as TNF-
) had different effectiveness in controlling the infection in infected
670
epithelia model cells between the two serovars (136)
. Using a similar co-culture model our
671 team has also demonstrated sustained IL-6 production in response to C. trachomatis L2
672
infection (122). A RNAseq methodology to examine host and chlamydial gene expression
673 enabled the investigators to identify that a fibrotic profile of gene expression being induced in
674
infected HEP-2 cells (137). The role of TNF-α in inhibiting chlamydial development was
675 evaluated by addition of recombinant TNF-α to Hep2 cells prior to infection which resulted
676
in smaller inclusion bodies (138). Furthermore, addition of IFN-γ to the cell line showed that
677
in combination with TNF-α, chlamydial replication was inhibited (138). Lu
et al
678 showed that chlamydial infection of several epithelial cell lines resulted in the secretion of
679 mature IL-18. IL-18 is known to potentiate the Th1 immune response and enhance production
680
681
682 Conclusion
30
683 Overwhelmingly, the studies of in vivo responses , ex vivo cultures , and laboratory cell culture
684
685
686 models all support a higher level or predominance of a Th1 or cytotoxic profile of immune response to chlamydial infection, with IFN-
, IL-8, IL-1
, and IL-6 findings featuring almost universally in the studies (although IFN-
was also associated with protection against repeat
687 infection). However, it is not clear if the pathological response is moderated or different
688 between women who develop pathology or those who resolve the infection without
689 pathology. Longitudinal sampling and analysis of correlates of the local immune response,
690 PMBC response, infection clearance relative to initial infection burden with the development
691 of upper reproductive tract pathology is one possible study design that could help to clarify
692 the contribution of pro-inflammatory primary immunity.
693
694
695
696
697
Chlamydial factors that may influence the development of pathology
698 Chlamydial serovar can associate with repeat infection and symptoms that may link to a
699 propensity to cause pathology and infertility
700 Chlamydial serovars are assigned based on the outer membrane proteins, typically by
701 sequencing so studies that refer to serovars are actually frequently referring to genovars
702
(140). Serovar E and serovar F are generally found to be predominant in most countries
703
including: Australia, Netherlands, and Sweden (67, 141-144). Using
omp 1 PCR based RFLP
704 genotyping Lan et al.
, (145) reported that in women less than 30 years old, serovars D (4/21
31
705 asymptomatic women) and I (4/21 asymptomatic women) were associated with asymptomatic
706 infection, while serovar G was associated with symptomatic infections (4/30 symptomatic
707 cases). Similarly, Gao et al
., (143) also reported the predominance of serovar G in
708
709
710 symptomatic infection, particularly lower abdominal pain (18/33 patients) as compared to asymptomatic patients (
P < 0.001) amongst female sex workers and STD patients in China.
47.5% (28/59) asymptomatic patients had serovar E (143).
Verweij et al ., (2014) reported
711 that different serovars induced differential serological responses in 510 women with PCR
712 confirmed C. trachomatis
infection (146). The study showed that serovar D (n=45) and E
713 (n=217) from serogroup B elicited the highest IgG response (Median IgG titre of 200)
714
followed by serovar H (n=20) (146). Women with persisting infections were found to have
715 twice as may serovar E infections (67%, 8/12) compared to women who naturally cleared
716 infections (33% 3/9) during a longitudinal study of women with asymptomatic C.
717 trachomatis
infections, however this was not significantly different (147). However, several
718 study design flaws have been raised about the Morre et al., 2002 study and therefore it may
719
not be relevant to include these data to make conclusions (eg see (148, 149)). Whilst not
720 linked directly to infertility, the majority of evidence from these studies support that different
721 serovars do have different associations with symptoms, re-infection, or infection duration, all
722 of which may contribute to pathology development.
723
724 Chlamydial genotypes can mediate tissue tropism and may be a factor in pathology
725 development
726 There are several published examples of C. trachomatis genotypic changes associating with
727 tissue tropism, however, no reports yet aligning chlamydial genotype with pathology
728 development and infertility. The most well know genotype that mediates tissue tropism is
32
729 actually polymorphisms in the trpAB operon and the ability to synthesis tryptophan from
730 indole between C. trachomatis
ocular and genital strains (79, 150) which we will mention
731 here given the significance of this finding to the field even though this review is focussed on
732 infertility.
There is also evidence of positively selected genotypes that align with tissue
733 trophism (ocular, genital, mononuclear/invasive), for example in a review of 59 C.
734 trachomatis genome sequences, it was reported that tarp , and the pmp genes have positively
735
selected polymorphisms that significantly cluster with tissue niche (151). Polymorphisms in
736 three distinct open reading frames have been found to associate with rectal but not cervical
737 serovar G isolates, and two further open reading frame polymorphisms were found to
738
associate with rectal and cervical tropism of serovars E, F and J (152). These studies do not
739 identify pathology associated polymorphisms, however they do support the theoretical
740 potential for chlamydial genotypes to exist that either improved ascension, or upper
741 reproductive tract survival or polymorphisms that alter the immune response. Any association
742 a chlamydial genotype with pathology development would only be possible by a longitudinal
743 study of a large group of women throughout their reproductive years with continual sampling
744 and analysis of infecting chlamydial strains.
745
746
Conclusions
747 A better understanding of the disease mechanism and the risk factors associated with C.
748 trachomatis infertility would enable specific screening for at risk women and inform vaccine
749 development targeted to prevent the progress of infection to infertility or pathology. Whilst
750 there are several convincing models of how the disease pathology potentially occurs, each
751 with some supporting evidence from the human data reviewed here, the actual process or host
752 and pathogen factors that result in infertility remain uncertain and require further
33
753 investigation. It is clear that a pro-inflammatory response is largely elicited in response to
754 chlamydial infection, whether this response or the extent of this response is the primary
755 determinant of pathology remains unclear. Furthermore, whilst there are tantalising
756 associations there are not yet definitive correlates of contributions of many host and pathogen
757 factors to pathology risk including; human genetic polymorphisms, C. trachomatis serovar
758 and genotype specific distinctions, co-infection or microbiome parameters, and risk
759 behaviours like repeat infections or age of sexual debut (summarised in Fig. 2.). A
760 comprehensive and extended longitudinal analysis of each of these factors using a very large
761 cohort study of women prior to any infection in early teen years until post-pregnancy age
762 (with adequate statistical power) would be the most robust way to monitor disease factors and
763 pathology outcomes in women. Identification of the major contributing factors to disease
764 pathology would better inform design of future vaccines and would also enable design of
765 molecular diagnostics for early detection of women at risk of the pathology development.
766
767 In the absence of such comprehensive knowledge and subsequent preventative interventions
768 (enhanced diagnosis or vaccine) there is a real opportunity to alleviate some of the risks and
769 costs associated with the pathological outcome from infection by improving guidelines for
770
screening, as recently proposed in the UK (153). Further to this we propose that improved use
771 of serological diagnosis of pathology risk expediting infertility diagnosis for women, and also
772
as a tool to predict the risk of ectopic pregnancy or PID in women (27, 33), who have had
773 chlamydial infections should also be rigorously evaluated and considered for routine
774 implementation in both fertility and general practice clinic settings.
775
34
References
1.
2.
3.
4.
5.
6.
7.
8.
9.
Anonymous.
2005. Prevalence and incidence of selected sexually transmitted infections. WHO,
CDC. 2013. http://www.cdc.gov/std/stats/sti-estimates-fact-sheet-feb-2013.pdf
.
Accessed
Land JA, Evers J. 2002. Chlamydia infection and subfertility. Best practice & research Clinical obstetrics & gynaecology 16: 901.
Horn M, Collingro A, Schmitz-Esser S, Beier CL, Purkhold U, Fartmann B,
Brandt P, Nyakatura GJ, Droege M, Frishman D, Rattei T, Mewes HW, Wagner
M. 2004. Illuminating the evolutionary history of chlamydiae. Science 304: 728-730.
De Clercq E, Kalmar I, Vanrompay D. 2013. Animal models for studying female genital tract infection with Chlamydia trachomatis. Infect Immun 81: 3060-3067.
Apari P, de Sousa JD, Muller V. 2014. Why sexually transmitted infections tend to cause infertility: an evolutionary hypothesis. PLoS Pathog 10: e1004111.
Peipert JF. 2003. Clinical practice. Genital chlamydial infections. N Engl J Med
349: 2424-2430.
Lewis D, Newton DC, Guy RJ, Ali H, Chen MY, Fairley CK, Hocking JS. 2012.
The prevalence of Chlamydia trachomatis infection in Australia: a systematic review and meta-analysis. BMC Infect Dis 12: 113.
Sonnenberg P, Clifton S, Beddows S, Field N, Soldan K, Tanton C, Mercer CH, da Silva FC, Alexander S, Copas AJ, Phelps A, Erens B, Prah P, Macdowall W,
Wellings K, Ison CA, Johnson AM. 2013. Prevalence, risk factors, and uptake of
35
interventions for sexually transmitted infections in Britain: findings from the National
Surveys of Sexual Attitudes and Lifestyles (Natsal). Lancet 382: 1795-1806.
10. Datta SD, Sternberg M, Johnson RE, Berman S, Papp JR, McQuillan G,
Weinstock H. 2007. Gonorrhea and chlamydia in the United States among persons 14 to 39 years of age, 1999 to 2002. Ann Intern Med 147: 89-96.
11. Datta SD, Torrone E, Kruszon-Moran D, Berman S, Johnson R, Satterwhite CL,
Papp J, Weinstock H. 2012. Chlamydia trachomatis trends in the United States among persons 14 to 39 years of age, 1999-2008. Sex Transm Dis 39: 92-96.
12. Price MJ, Ades AE, de Angelis D, Welton NJ, Macleod J, Turner K, Horner PJ.
2014. Incidence of Chlamydia trachomatis infection in women in England: two methods of estimation. Epidemiol Infect 142: 562-576.
13. Price MJ, Ades AE, De Angelis D, Welton NJ, Macleod J, Soldan K, Simms I,
Turner K, Horner PJ. 2013. Risk of pelvic inflammatory disease following
Chlamydia trachomatis infection: analysis of prospective studies with a multistate model. Am J Epidemiol 178: 484-492.
14. Batteiger BE, Tu W, Ofner S, Van Der Pol B, Stothard DR, Orr DP, Katz BP,
Fortenberry JD. 2010. Repeated Chlamydia trachomatis genital infections in adolescent women. J Infect Dis 201: 42-51.
15. Burstein GR, Zenilman JM, Gaydos CA, Diener-West M, Howell MR,
Brathwaite W, Quinn TC. 2001. Predictors of repeat Chlamydia trachomatis infections diagnosed by DNA amplification testing among inner city females.
Sexually Transmitted Infections 77: 26-32.
16. Low N, Egger M, Sterne JA, Harbord RM, Ibrahim F, Lindblom B, Herrmann
B. 2006. Incidence of severe reproductive tract complications associated with
36
diagnosed genital chlamydial infection: the Uppsala Women's Cohort Study. Sexually
Transmitted Infections 82: 212-218.
17. Mania-Pramanik J, Kerkar S, Sonawane S, Mehta P, Salvi V. 2012. Current
Chlamydia trachomatis Infection, A Major Cause of Infertility. J Reprod Infertil
13: 204-210.
18. Wallace LA, Scoular A, Hart G, Reid M, Wilson P, Goldberg DJ. 2008. What is the excess risk of infertility in women after genital chlamydia infection? A systematic review of the evidence. Sex Transm Infect 84: 171-175.
19.
Westr¨om L, Joesoef R, Reynolds G, Hadgu A, Tompson SE.
1992. Pelvic inflammatory disease and fertility. A cohort study of 1844 women with laparoscopically verified disease and 657 control women with normal laparoscopic results. Sex Trans Dis 19: 185-192.
20. Haggerty CL, Gottlieb SL, Taylor BD, Low N, Xu F, Ness RB. 2010. Risk of sequelae after Chlamydia trachomatis genital infection in women. J Infect Dis 201
Suppl 2: S134-155.
21. Oakeshott P, Kerry S, Aghaizu A, Atherton H, Hay S, Taylor-Robinson D,
Simms I, Hay P. 2010. Randomised controlled trial of screening for Chlamydia trachomatis to prevent pelvic inflammatory disease: the POPI (prevention of pelvic infection) trial. BMJ 340: c1642.
22. Herzog SA, Althaus CL, Heijne JC, Oakeshott P, Kerry S, Hay P, Low N. 2012.
Timing of progression from Chlamydia trachomatis infection to pelvic inflammatory disease: a mathematical modelling study. BMC Infect Dis 12: 187.
23. Land JA, Gijsen AP, Kessels AGH, Slobbe MEP, Bruggeman CA. 2003.
Performance of five serological chlamydia antibody tests in subfertile women. Human
Reproduction 18: 2621-2627.
37
24. Broeze KA, Opmeer BC, Coppus SF, Van Geloven N, Alves MF, Anestad G,
Bhattacharya S, Allan J, Guerra-Infante MF, Den Hartog JE, Land JA, Idahl A,
Van der Linden PJ, Mouton JW, Ng EH, Van der Steeg JW, Steures P,
Svenstrup HF, Tiitinen A, Toye B, Van der Veen F, Mol BW. 2011. Chlamydia antibody testing and diagnosing tubal pathology in subfertile women: an individual patient data meta-analysis. Human Reproduction Update 17: 301-310.
25. Eggert-Kruse W, Rohr G, Demirakca T, Rusu R, Naher H, Petzoldt D,
Runnebaum B. 1997. Chlamydial serology in 1303 asymptomatic subfertile couples.
Hum Reprod 12: 1464-1475.
26. Akande VA, Hunt LP, Cahill DJ, Caul EO, Ford WC, Jenkins JM. 2003. Tubal damage in infertile women: prediction using chlamydia serology. Hum Reprod
18: 1841-1847.
27. Keltz MD, Gera PS, Moustakis M. 2006. Chlamydia serology screening in infertility patients. Fertil Steril 85: 752-754.
28. Muvunyi CM, Dhont N, Verhelst R, Temmerman M, Claeys G, Padalko E. 2011.
Chlamydia trachomatis infection in fertile and subfertile women in Rwanda: prevalence and diagnostic significance of IgG and IgA antibodies testing. Hum
Reprod 26: 3319-3326.
29. Coppus SF, Opmeer BC, Logan S, van der Veen F, Bhattacharya S, Mol BW.
2007. The predictive value of medical history taking and Chlamydia IgG ELISA antibody testing (CAT) in the selection of subfertile women for diagnostic laparoscopy: a clinical prediction model approach. Hum Reprod 22: 1353-1358.
30. Toye B, Laferriere C, Claman P, Jessamine P, Peeling R. 1993. Association between antibody to the chlamydial heat-shock protein and tubal infertility. J Infect
Dis 168: 1236-1240.
38
31. Claman P, Honey L, Peeling RW, Jessamine P, Toye B. 1997. The presence of serum antibody to the chlamydial heat shock protein (CHSP60) as a diagnostic test for tubal factor infertility. Fertil Steril 67: 501-504.
32. Tiitinen A, Surcel HM, Halttunen M, Birkelund S, Bloigu A, Christiansen G,
Koskela P, Morrison SG, Morrison RP, Paavonen J. 2006. Chlamydia trachomatis and chlamydial heat shock protein 60-specific antibody and cell-mediated responses predict tubal factor infertility. Human Reproduction 21: 1533-1538.
33. Keltz MD, Sauerbrun-Cutler MT, Durante MS, Moshier E, Stein DE, Gonzales
E. 2013. Positive Chlamydia trachomatis serology result in women seeking care for infertility is a negative prognosticator for intrauterine pregnancy. Sex Transm Dis
40: 842-845.
34. Price MJ, Ades AE, Welton NJ, Macleod J, Turner K, Simms I, Horner PJ. 2012.
How much tubal factor infertility is caused by Chlamydia? Estimates based on serological evidence corrected for sensitivity and specificity. Sex Transm Dis 39: 608-
613.
35. Lan J, van den Brule AJ, Hemrika DJ, Risse EK, Walboomers JM, Schipper
ME, Meijer CJ. 1995. Chlamydia trachomatis and ectopic pregnancy: retrospective analysis of salpingectomy specimens, endometrial biopsies, and cervical smears.
Journal of Clinical Pathology 48: 815-819.
36. Khin Nwe O, Wah Wah A, Moe T, Khin Thet W, Hta Hta Y, Win Win M. 2011.
Case-control study of ectopic pregnancies in Myanmar: infectious etiological factors.
Southeast Asian J Trop Med Public Health 42: 347-354.
37. Barlow RE, Cooke ID, Odukoya O, Heatley MK, Jenkins J, Narayansingh G,
Ramsewak SS, Eley A. 2001. The prevalence of Chlamydia trachomatis in fresh
39
tissue specimens from patients with ectopic pregnancy or tubal factor infertility as determined by PCR and in-situ hybridisation. J Med Microbiol 50: 902-908.
38. Mardh PA, Moller BR, Ingerselv HJ, Nussler E, Westrom L, Wolner-Hanssen P.
1981. Endometritis caused by Chlamydia trachomatis. Br J Vener Dis 57: 191-195.
39. Mardh PA, Wolner-Hanssen P. 1982. Three novel manifestations of chlamydia trachomatis infection- endometritis, perihepatitis and meningoencephalitis. Infection
10 Suppl 1: S57-60.
40. Tait IA, Duthie SJ, Taylor-Robinson D. 1997. Silent upper genital tract chlamydial infection and disease in women. Int J STD AIDS 8: 329-331.
41. Persson K, Osser S. 1993. Lack of evidence of a relationship between genital symptoms, cervicitis and salpingitis and different serovars of Chlamydia trachomatis.
Eur J Clin Microbiol Infect Dis 12: 195-199.
42. Wolner-Hanssen P, Mardh PA, Svensson L, Westrom L. 1983. Laparoscopy in women with chlamydial infection and pelvic pain: a comparison of patients with and without salpingitis. Obstet Gynecol 61: 299-303.
43. Ness RB, Soper DE, Richter HE, Randall H, Peipert JF, Nelson DB, Schubeck D,
McNeeley SG, Trout W, Bass DC, Hutchison K, Kip K, Brunham RC. 2008.
Chlamydia antibodies, chlamydia heat shock protein, and adverse sequelae after pelvic inflammatory disease: the PID Evaluation and Clinical Health (PEACH) Study.
Sex Transm Dis 35: 129-135.
44. Korn AP, Hessol NA, Padian NS, Bolan GA, Donegan E, Landers DV, Schachter
J. 1998. Risk factors for plasma cell endometritis among women with cervical
Neisseria gonorrhoeae, cervical Chlamydia trachomatis, or bacterial vaginosis. Am J
Obstet Gynecol 178: 987-990.
40
45. Wyrick PB. 2010. Chlamydia trachomatis persistence in vitro: an overview. Journal of Infectious Diseases 201 Suppl 2: S88-95.
46. Hogan R, Mathews SA, Mukhopadhyay S, Summersgill JT, Timms P. 2004.
Chlamydial persistence: beyond the biphasic paradigm. Infection and Immunity
72: 1843-1855.
47. Arsovic A, Nikolov A, Sazdanovic P, Popovic S, Baskic D. 2014. Prevalence and diagnostic significance of specific IgA and anti-heat shock protein 60 Chlamydia trachomatis antibodies in subfertile women. Eur J Clin Microbiol Infect Dis 33: 761-
766.
48. Bjartling C, Osser S, Persson K. 2000. The frequency of salpingitis and ectopic pregnancy as epidemiologic markers of Chlamydia trachomatis. Acta Obstet Gynecol
Scand 79: 123-128.
49. Campbell LA, Patton DL, Moore DE, Cappuccio AL, Mueller BA, Wang SP.
1993. Detection of Chlamydia trachomatis deoxyribonucleic acid in women with tubal infertility. Fertil Steril 59: 45-50.
50. Patton DL, Askienazy-Elbhar M, Henry-Suchet J, Campbell LA, Cappuccio A,
Tannous W, Wang SP, Kuo CC. 1994. Detection of Chlamydia trachomatis in fallopian tube tissue in women with postinfectious tubal infertility. Am J Obstet
Gynecol 171: 95-101.
51. Lewis ME, Belland RJ, AbdelRahman YM, Beatty WL, Aiyar AA, Zea AH,
Greene SJ, Marrero L, Buckner LR, Tate DJ, McGowin CL, Kozlowski PA,
O'Brien M, Lillis RA, Martin DH, Quayle AJ. 2014. Morphologic and molecular evaluation of Chlamydia trachomatis growth in human endocervix reveals distinct growth patterns. Front Cell Infect Microbiol 4: 71.
41
52. Bavoil PM. 2014. What's in a word: the use, misuse, and abuse of the word
"persistence" in Chlamydia biology. Front Cell Infect Microbiol 4: 27.
53. Stephens RS. 2003. The cellular paradigm of chlamydial pathogenesis. TRENDS in
Microbiology 11: 44-51.
54. Hillis SD, Owens LM, Marchbanks PA, Amsterdam LF, Mac Kenzie WR. 1997.
Recurrent chlamydial infections increase the risks of hospitalization for ectopic pregnancy and pelvic inflammatory disease. Am J Obstet Gynecol 176: 103-107.
55. Yang X. 2001. Distinct function of Th1 and Th2 type delayed type hypersensitivity: protective and pathological reactions to chlamydial infection. Microsc Res Tech
53: 273-277.
56. Witkin SS, Askienazy-Elbhar M, Henry-Suchet J, Belaisch-Allart J, Tort-
Grumbach J, Sarjdine K. 1998. Circulating antibodies to a conserved epitope of the
Chlamydia trachomatis 60 kDa heat shock protein (hsp60) in infertile couples and its relationship to antibodies to C.trachomatis surface antigens and the Escherichia coli and human HSP60. Human Reproduction 13: 1175-1179.
57. Spandorfer SD, Neuer A, LaVerda D, Byrne G, Liu HC, Rosenwaks Z, Witkin
SS. 1999. Previously undetected Chlamydia trachomatis infection, immunity to heat shock proteins and tubal occlusion in women undergoing in-vitro fertilization. Hum
Reprod 14: 60-64.
58. Witkin SS, Linhares IM. 2002. Chlamydia trachomatis in subfertile women undergoing uterine instrumentation - An alternative to direct microbial testing or prophylactic antibiotic treatment. Human Reproduction 17: 1938-1941.
59. Hjelholt A, Christiansen G, Johannesson TG, Ingerslev HJ, Birkelund S. 2011.
Tubal factor infertility is associated with antibodies against Chlamydia trachomatis heat shock protein 60 but not human HSP60. Human Reproduction 26: 2069-2076.
42
60. Morrison RP, Lyng K, Caldwell HD. 1989. Chlamydial disease pathogenesis.
Ocular hypersensitivity elicited by a genus-specific 57-kD protein. J Exp Med
169: 663-675.
61. Rank RG, Dascher C, Bowlin AK, Bavoil PM. 1995. Systemic immunization with
Hsp60 alters the development of chlamydial ocular disease. Invest Ophthalmol Vis
Sci 36: 1344-1351.
62. Watkins NG, Hadlow WJ, Moos AB, Caldwell HD. 1986. Ocular delayed hypersensitivity: a pathogenetic mechanism of chlamydial-conjunctivitis in guinea pigs. Proc Natl Acad Sci U S A 83: 7480-7484.
63. Javaloy J, Ferrer C, Vidal MT, Alio JL. 2003. Follicular conjunctivitis caused by
Chlamydia trachomatis in an infant Saharan population: molecular and clinical diagnosis. Br J Ophthalmol 87: 142-146.
64. Jakus S, Neuer A, Dieterle S, Bongiovanni AM, Witkin SS. 2008. Antibody to the
Chlamydia trachomatis 60 kDa heat shock protein in follicular fluid and in vitro fertilization outcome. Am J Reprod Immunol 59: 85-89.
65. de Barbeyrac B, Papaxanthos-Roche A, Mathieu C, Germain C, Brun JL,
Gachet M, Mayer G, Bebear C, Chene G, Hocke C. 2006. Chlamydia trachomatis in subfertile couples undergoing an in vitro fertilization program: a prospective study.
Eur J Obstet Gynecol Reprod Biol 129: 46-53.
66. Hosenfeld CB, Workowski KA, Berman S, Zaidi A, Dyson J, Mosure D, Bolan G,
Bauer HM. 2009. Repeat infection with Chlamydia and gonorrhea among females: a systematic review of the literature. Sex Transm Dis 36: 478-489.
67. Walker J, Tabrizi SN, Fairley CK, Chen MY, Bradshaw CS, Twin J, Taylor N,
Donovan B, Kaldor JM, McNamee K, Urban E, Walker S, Currie M, Birden H,
Bowden F, Gunn J, Pirotta M, Gurrin L, Harindra V, Garland SM, Hocking JS.
43
2012. Chlamydia trachomatis incidence and re-infection among young women-behavioural and microbiological characteristics. PLoS One 7: e37778.
68. Brunham RC, Pourbohloul B, Mak S, White R, Rekart ML. 2005. The unexpected impact of a Chlamydia trachomatis infection control program on susceptibility to reinfection. J Infect Dis 192: 1836-1844.
69. Scott Lamontagne D, Baster K, Emmett L, Nichols T, Randall S, McLean L,
Meredith P, Harindra V, Tobin JM, Underhill GS, Graham Hewitt W, Hopwood
J, Gleave T, Ghosh AK, Mallinson H, Davies AR, Hughes G, Fenton KA,
Chlamydia Recall Study Advisory G. 2007. Incidence and reinfection rates of genital chlamydial infection among women aged 16-24 years attending general practice, family planning and genitourinary medicine clinics in England: a prospective cohort study by the Chlamydia Recall Study Advisory Group. Sex Transm Infect
83: 292-303.
70. Horner PJ. 2012. Azithromycin antimicrobial resistance and genital Chlamydia trachomatis infection: duration of therapy may be the key to improving efficacy. Sex
Transm Infect 88: 154-156.
71. Dreses-Werringloer U, Padubrin I, Zeidler H, Kohler L. 2001. Effects of azithromycin and rifampin on Chlamydia trachomatis infection in vitro. Antimicrob
Agents Chemother 45: 3001-3008.
72. Brunham RC, Rekart ML. 2008. The arrested immunity hypothesis and the epidemiology of Chlamydia control. Sex Transm Dis 35: 53-54.
73. Brunham RC, Rey-Ladino J. 2005. Immunology of Chlamydia infection: implications for a Chlamydia trachomatis vaccine. Nat Rev Immunol 5: 149-161.
44
74. Dicker LW, Mosure DJ, Berman SM, Levine WC. 2003. Gonorrhea prevalence and coinfection with chlamydia in women in the United States, 2000. Sex Transm Dis
30: 472-476.
75. De Muylder X, Laga M, Tennstedt C, Van Dyck E, Aelbers GN, Piot P. 1990. The role of Neisseria gonorrhoeae and Chlamydia trachomatis in pelvic inflammatory disease and its sequelae in Zimbabwe. J Infect Dis 162: 501-505.
76. Wiesenfeld HC, Hillier SL, Krohn MA, Landers DV, Sweet RL. 2003. Bacterial vaginosis is a strong predictor of Neisseria gonorrhoeae and Chlamydia trachomatis infection. Clin Infect Dis 36: 663-668.
77. Gong Z, Luna Y, Yu P, Fan H. 2014. Lactobacilli inactivate Chlamydia trachomatis through lactic acid but not H2O2. PLoS One 9: e107758.
78. Caldwell HD, Wood H, Crane C, Bailey R, Jones RB, Mabey D, Maclean I,
Mohammed Z, Peeling R, Roshick C, Schachter J, Solomon AW, Stamm WE,
Suchland RJ, Taylor L, West SK, Quinn TC, Belland RJ, McClarty G. 2003.
Polymorphisms in Chlamydia trachomatis tryptophan synthase genes differentiate between genital and ocular isolates. The Journal of Clinical Investigation 111: 1757-
1769.
79. Nelson DE, Virok DP, Wood H, Roshick C, Johnson RM, Whitmire WM, Crane
DD, Steele-Mortimer O, Kari L, McClarty G, Caldwell HD. 2005. Chlamydial
IFN-gamma immune evasion is linked to host infection tropism. Proc Natl Acad Sci U
S A 102: 10658-10663.
80. Taylor BD, Darville T, Haggerty CL. 2013. Does bacterial vaginosis cause pelvic inflammatory disease? Sex Transm Dis 40: 117-122.
45
81. Arno JN, Katz BP, McBride R, Carty GA, Batteiger BE, Caine VA, Jones RB.
1994. Age and clinical immunity to infections with Chlamydia trachomatis. Sex
Transm Dis 21: 47-52.
82. Bender N, Herrmann B, Andersen B, Hocking JS, van Bergen J, Morgan J, van den Broek IV, Zwahlen M, Low N. 2011. Chlamydia infection, pelvic inflammatory disease, ectopic pregnancy and infertility: cross-national study. Sex Transm Infect
87: 601-608.
83. Walker J, Tabrizi SN, Fairley CK, Chen MY, Bradshaw CS, Twin J, Taylor N,
Donovan B, Kaldor JM, McNamee K. 2012. Chlamydia trachomatis Incidence and
Re-Infection among Young Women–Behavioural and Microbiological
Characteristics. PloS one 7: e37778.
84. Barnes RC, Katz BP, Rolfs RT, Batteiger B, Caine V, Jones RB. 1990.
Quantitative culture of endocervical Chlamydia trachomatis. J Clin Microbiol 28: 774-
780.
85. Macleod J, Salisbury C, Low N, McCarthy A, Sterne JA, Holloway A, Patel R,
Sanford E, Morcom A, Horner P, Davey Smith G, Skidmore S, Herring A, Caul
O, Hobbs FD, Egger M. 2005. Coverage and uptake of systematic postal screening for genital Chlamydia trachomatis and prevalence of infection in the United Kingdom general population: cross sectional study. BMJ 330: 940.
86. Skjeldestad FE, Marsico MA, Sings HL, Nordbo SA, Storvold G. 2009. Incidence and risk factors for genital Chlamydia trachomatis infection: a 4-year prospective cohort study. Sex Transm Dis 36: 273-279.
87. Okumu CV, Kamau RK, Rogo KO. 1990. Past reproductive and sexual characteristics of women with tubal infertility at Kenyatta National Hospital. East Afr
Med J 67: 864-872.
46
88. Brabin L, Fairbrother E, Mandal D, Roberts SA, Higgins SP, Chandiok S, Wood
P, Barnard G, Kitchener HC. 2005. Biological and hormonal markers of chlamydia, human papillomavirus, and bacterial vaginosis among adolescents attending genitourinary medicine clinics. Sex Transm Infect 81: 128-132.
89. Farrow A, Hull MG, Northstone K, Taylor H, Ford WC, Golding J. 2002.
Prolonged use of oral contraception before a planned pregnancy is associated with a decreased risk of delayed conception. Hum Reprod 17: 2754-2761.
90. Lal JA, Malogajski J, Verweij SP, de Boer P, Ambrosino E, Brand A, Ouburg S,
Morre SA. 2013. Chlamydia trachomatis infections and subfertility: opportunities to translate host pathogen genomic data into public health. Public Health Genomics
16: 50-61.
91. Yu L, Wang L, Chen S. 2009. Toll-like receptors, inflammation and tumor in the human female reproductive tract. Am J Reprod Immunol 62: 1-8.
92. Laisk T, Peters M, Saare M, Haller-Kikkatalo K, Karro H, Salumets A. 2010.
Association of CCR5, TLR2, TLR4 and MBL genetic variations with genital tract infections and tubal factor infertility. J Reprod Immunol 87: 74-81.
93. Karimi O, Ouburg S, de Vries HJ, Pena AS, Pleijster J, Land JA, Morre SA.
2009. TLR2 haplotypes in the susceptibility to and severity of Chlamydia trachomatis infections in Dutch women. Drugs Today (Barc) 45 Suppl B: 67-74.
94. Taylor BD, Darville T, Ferrell RE, Kammerer CM, Ness RB, Haggerty CL. 2012.
Variants in toll-like receptor 1 and 4 genes are associated with Chlamydia trachomatis among women with pelvic inflammatory disease. J Infect Dis 205: 603-609.
95. den Hartog JE, Ouburg S, Land JA, Lyons JM, Ito JI, Pena AS, Morre SA. 2006.
Do host genetic traits in the bacterial sensing system play a role in the development of
47
Chlamydia trachomatis-associated tubal pathology in subfertile women? BMC Infect
Dis 6: 122.
96. Wang W, Stassen FR, Surcel HM, Ohman H, Tiitinen A, Paavonen J, de Vries
HJ, Heijmans R, Pleijster J, Morre SA, Ouburg S. 2009. Analyses of polymorphisms in the inflammasome-associated NLRP3 and miRNA-146A genes in the susceptibility to and tubal pathology of Chlamydia trachomatis infection. Drugs
Today (Barc) 45 Suppl B: 95-103.
97. Laisk T, Peters M, Salumets A. 2011. Mannose-binding lectin genotypes: potential role in tubal damage and adverse IVF outcome. J Reprod Immunol 92: 62-67.
98. Cohen CR, Gichui J, Rukaria R, Sinei SS, Gaur LK, Brunham RC. 2003.
Immunogenetic correlates for Chlamydia trachomatis-associated tubal infertility.
Obstet Gynecol 101: 438-444.
99. Wang C, Tang J, Geisler WM, Crowley-Nowick PA, Wilson CM, Kaslow RA.
2005. Human leukocyte antigen and cytokine gene variants as predictors of recurrent
Chlamydia trachomatis infection in high-risk adolescents. J Infect Dis 191: 1084-
1092.
100. Kinnunen AH, Surcel HM, Lehtinen M, Karhukorpi J, Tiitinen A, Halttunen M,
Bloigu A, Morrison RP, Karttunen R, Paavonen J. 2002. HLA DQ alleles and interleukin-10 polymorphism associated with Chlamydia trachomatis-related tubal factor infertility: a case-control study. Hum Reprod 17: 2073-2078.
101. Ohman H, Tiitinen A, Halttunen M, Paavonen J, Surcel HM. 2011. Cytokine gene polymorphism and Chlamydia trachomatis-specific immune responses. Hum Immunol
72: 278-282.
48
102. Ohman H, Tiitinen A, Halttunen M, Lehtinen M, Paavonen J, Surcel HM. 2009.
Cytokine polymorphisms and severity of tubal damage in women with Chlamydiaassociated infertility. J Infect Dis 199: 1353-1359.
103. Ohman H, Bailey R, Natividad A, Ragoussis J, Johnson LL, Tiitinen A,
Halttunen M, Paavonen J, Surcel HM. 2012. Effect of IL12A and IL12B polymorphisms on the risk of Chlamydia trachomatis-induced tubal factor infertility and disease severity. Hum Reprod 27: 2217-2223.
104. Murillo LS, Land JA, Pleijster J, Bruggeman CA, Pena AS, Morre SA. 2003.
Interleukin-1B (IL-1B) and interleukin-1 receptor antagonist (IL-1RN) gene polymorphisms are not associated with tubal pathology and Chlamydia trachomatisrelated tubal factor subfertility. Hum Reprod 18: 2309-2314.
105. Eng HL, Wang CH, Chen CH, Chou MH, Cheng CT, Lin TM. 2004. A CD14 promoter polymorphism is associated with CD14 expression and Chlamydiastimulated TNF alpha production. Genes Immun 5: 426-430.
106. Eng HL, Chen CH, Kuo CC, Wu JS, Wang CH, Lin TM. 2003. Association of
CD14 promoter gene polymorphism and Chlamydia pneumoniae infection. J Infect
Dis 188: 90-97.
107. Muraille E, Leo O. 1998. Revisiting the Th1/Th2 paradigm. Scand J Immunol 47: 1-
9.
108. Mascellino MT, Boccia P, Oliva A. 2011. Immunopathogenesis in Chlamydia trachomatis Infected Women. ISRN Obstet Gynecol 2011: 436936.
109. Perry LL, Feilzer K, Caldwell HD. 1997. Immunity to Chlamydia trachomatis is mediated by T helper 1 cells through IFN-gamma-dependent and -independent pathways. J Immunol 158: 3344-3352.
49
110. Khader SA, Gopal R. 2010. IL-17 in protective immunity to intracellular pathogens.
Virulence 1: 423-427.
111. Arno JN, Ricker VA, Batteiger BE, Katz BP, Caine VA, Jones RB. 1990.
Interferon-gamma in endocervical secretions of women infected with Chlamydia trachomatis. J Infect Dis 162: 1385-1389.
112. Spear GT, Kendrick SR, Chen HY, Thomas TT, Bahk M, Balderas R, Ghosh S,
Weinberg A, Landay AL. 2011. Multiplex immunoassay of lower genital tract mucosal fluid from women attending an urban STD clinic shows broadly increased
IL1ss and lactoferrin. PloS one 6: e19560.
113. Agrawal T, Vats V, Salhan S, Mittal A. 2007. Mucosal and peripheral immune responses to chlamydial heat shock proteins in women infected with Chlamydia trachomatis. Clin Exp Immunol 148: 461-468.
114. Jha R, Srivastava P, Salhan S, Finckh A, Gabay C, Mittal A, Bas S. 2011.
Spontaneous secretion of interleukin-17 and -22 by human cervical cells in
Chlamydia trachomatis infection. Microbes Infect 13: 167-178.
115. Kelly KA, Wiley D, Wiesmeier E, Briskin M, Butch A, Darville T. 2009. The combination of the gastrointestinal integrin (alpha4beta7) and selectin ligand enhances T-Cell migration to the reproductive tract during infection with Chlamydia trachomatis. Am J Reprod Immunol 61: 446-452.
116. Agrawal T, Bhengraj AR, Vats V, Salhan S, Mittal A. 2011. Expression of TLR 2,
TLR 4 and iNOS in cervical monocytes of Chlamydia trachomatis-infected women and their role in host immune response. Am J Reprod Immunol 66: 534-543.
117. Gupta R, Vardhan H, Srivastava P, Salhan S, Mittal A. 2009. Modulation of cytokines and transcription factors (T-Bet and GATA3) in CD4 enriched cervical
50
cells of Chlamydia trachomatis infected fertile and infertile women upon stimulation with chlamydial inclusion membrane proteins B and C. Reprod Biol Endocrinol 7: 84.
118. Balasubamaniam ES, Van Noorden S, El-Bahrawy M. 2012. The expression of interleukin (IL)-6, Il-8 and their receptors in fallopian tubes with ectopic tubal gestation. Fertility and Sterility 98: 898-894.
119. Hvid M, Baczynska A, Deleuran B, Fedder J, Knudsen HJ, Christiansen G,
Birkelund S. 2007. Interleukin-1 is the initiator of Fallopian tube destruction during
Chlamydia trachomatis infection. Cell Microbiol 9: 2795-2803.
120. Shaw JL, Wills GS, Lee KF, Horner PJ, McClure MO, Abrahams VM,
Wheelhouse N, Jabbour HN, Critchley HO, Entrican G, Horne AW. 2011.
Chlamydia trachomatis infection increases fallopian tube PROKR2 via TLR2 and
NFkappaB activation resulting in a microenvironment predisposed to ectopic pregnancy. Am J Pathol 178: 253-260.
121. Kinnunen A, Molander P, Laurila A, Rantala I, Morrison R, Lehtinen M,
Karttunen R, Tiitinen A, Paavonen J, Surcel HM. 2000. Chlamydia trachomatis reactive T lymphocytes from upper genital tract tissue specimens. Hum Reprod
15: 1484-1489.
122. Rasmussen SJ, Eckmann L, Quayle AJ, Shen L, Zhang Y-X, Anderson DJ,
Fierer J, Stephens RS, Kagnoff MF. 1997. Secretion of proinflammatory cytokines by epithelial cells in response to Chlamydia infection suggest a central role for eptihelial cells in chlamydial pathogenesis. The Journal of Clinical Investigation
99: 77-87.
123. Kinnunen A, Surcel HM, Halttunen M, Tiitinen A, Morrison RP, Morrison SG,
Koskela P, Lehtinen M, Paavonen J. 2003. Chlamydia trachomatis heat shock
51
protein-60 induced interferon-gamma and interleukin-10 production in infertile women. Clin Exp Immunol 131: 299-303.
124. Cohen CR, Koochesfahani KM, Meier AS, Shen C, Karunakaran K, Ondondo B,
Kinyari T, Mugo NR, Nguti R, Brunham RC. 2005. Immunoepidemiologic profile of Chlamydia trachomatis infection: importance of heat-shock protein 60 and interferon- gamma. J Infect Dis 192: 591-599.
125. Schrader S, Klos A, Hess S, Zeidler H, Kuipers JG, Rihl M. 2007. Expression of imflammatory host genes in Chlamydia trachomatis-infected human monocytes.
Arthritis Research and Therapy 9: 54-62.
126. Debattista J, Timms P, Allan J. 2002. Reduced levels of gamma-interferon secretion in response to chlamydial 60 kDa heat shock protein amongst women with pelvic inflammatory disease and a history of repeated Chlamydia trachomatis infections.
Immunol Lett 81: 205-210.
127. Debattista J, Gazzard CM, Wood R, Allan JA, Allan JM, Scarman A, Mortlock
M, Timms P, Knox CL. 2004. Interactions of microbiology and pathology in women undergoing investigations for infertility. Infectious diseases, Obstetrics and
Gynecology 12: 135-145.
128. Gervassi A, Alderson MR, Suchland R, Maisonneuve JF, Grabstein KH, Probst
P. 2004. Differential regulation of inflammatory cytokine secretion by human dendritic cells upon Chlamydia trachomatis infection. Infect Immun 72: 7231-7239.
129. Matyszak MK, Young JL, Gaston JS. 2002. Uptake and processing of Chlamydia trachomatis by human dendritic cells. Eur J Immunol 32: 742-751.
130. Hook CE, Telyatnikova N, Goodall JC, Braud VM, Carmichael AJ, Wills MR,
Gaston JS. 2004. Effects of Chlamydia trachomatis infection on the expression of
52
natural killer (NK) cell ligands and susceptibility to NK cell lysis. Clin Exp Immunol
138: 54-60.
131. Cunningham K, Stansfield SH, Patel P, Menon S, Kienzle V, Allan JA, Huston
WM. 2013. The IL-6 response to Chlamydia from primary reproductive epithelial cells is hihgly variable and may be invovled in differential susceptibility to the immunopathological consequences of chlamydial infection. BMC Immunol 15: 50.
132. WYRICK PB, DAVIS CH, KNIGHT ST, CHOONG J, RAULSTON JE,
SCHRAMM, NARA. 1993. An In Vitro Human Epithelial Cell Culture System for
Studying the Pathogenesis of Chlamydia trachomatis. Sexually Transmitted Diseases
20: 248-256.
133. Cheng W, Shivshankar P, Zhong Y, Chen D, Li Z, Zhong G. 2008. Intracellular interleukin-1alpha mediates interleukin-8 production induced by Chlamydia trachomatis infection via a mechanism independent of type I interleukin-1 receptor.
Infect Immun 76: 942-951.
134. Rasmussen SJ, Eckmann L, Quayle AJ, Shen L, Zhang YX, Anderson DJ, Fierer
J, Stephens RS, Kagnoff MF. 1997. Secretion of proinflammatory cytokines by epithelial cells in response to Chlamydia infection suggests a central role for epithelial cells in chlamydial pathogenesis. J Clin Invest 99: 77-87.
135. Mpiga P, Mansour S, Morisset R, Beaulieu R, Ravaoarinoro M. 2006. Sustained interleukin-6 and interleukin-8 expression following infection with Chlamydia trachomatis serovar L2 in a HeLa/THP-1 cell co-culture model. Scandinavian Journal of Immunology 63: 199-207.
136. Dessus-Babus S, Darville TL, Cuozzo FP, Ferguson K, Wyrick PB. 2002.
Differences in innate immune responses (in vitro) to HeLa cells infected with
53
nondisseminating serovar E and disseminating serovar L2 of Chlamydia trachomatis.
Infection and Immunity 70: 3234-3248.
137. Humphrys MS, Creasy T, Sun Y, Shetty AC, Chibucos MC, Drabek EF, Fraser
CM, Farooq U, Sengamalay N, Ott S, Shou H, Bavoil PM, Mahurkar A, Myers
GS. 2013. Simultaneous transcriptional profiling of bacteria and their host cells. PLoS
One 8: e80597.
138. Shemer-Avni Y, Wallach D, Sarov I. 1988. Inhibition of Chlamydia trachomatis growth by recombinant tumor necrosis factor. Infect Immun 56: 2503-2506.
139. Lu H, Shen C, Brunham RC. 2000. Chlamydia trachomatis infection of epithelial cells induces the activation of caspase-1 and release of mature IL-18. J Immunol
165: 1463-1469.
140. Mylonas I. 2012. Female genital Chlamydia trachomatis infection: where are we heading? Archives of Gynecology and Obstetrics 285: 1271-1285.
141. Xiong L, Kong F, Zhou H, Gilbert GL. 2006. Use of PCR and reverse line blot hybridization assay for rapid simultaneous detection and serovar identification of
Chlamydia trachomatis. J Clin Microbiol 44: 1413-1418.
142. Jurstrand M, Falk L, Fredlund H, Lindberg M, Olcen P, Andersson S, Persson
K, Albert J, Backman A. 2001. Characterization of Chlamydia trachomatis omp1 genotypes among sexually transmitted disease patients in Sweden. J Clin Microbiol
39: 3915-3919.
143. Gao X, Chen XS, Yin YP, Zhong MY, Shi MQ, Wei WH, Chen Q, Peeling RW,
Mabey D. 2007. Distribution study of Chlamydia trachomatis serovars among highrisk women in China performed using PCR-restriction fragment length polymorphism genotyping. J Clin Microbiol 45: 1185-1189.
54
144. Quint KD, van Doorn LJ, Kleter B, de Koning MN, van den Munckhof HA,
Morre SA, ter Harmsel B, Weiderpass E, Harbers G, Melchers WJ, Quint WG.
2007. A highly sensitive, multiplex broad-spectrum PCR-DNA-enzyme immunoassay and reverse hybridization assay for rapid detection and identification of Chlamydia trachomatis serovars. J Mol Diagn 9: 631-638.
145. Lan J, Melgers I, Meijer CJ, Walboomers JM, Roosendaal R, Burger C, Bleker
OP, van den Brule AJ. 1995. Prevalence and serovar distribution of asymptomatic cervical Chlamydia trachomatis infections as determined by highly sensitive PCR. J
Clin Microbiol 33: 3194-3197.
146. Verweij SP, Lanjouw E, Bax CJ, Quint KD, Oostvogel PM, Dorr PJ, Pleijster J, de Vries HJ, Peters RP, Ouburg S, Morre SA. 2014. Serovar D and E of serogroup
B induce highest serological responses in urogenital Chlamydia trachomatis infections. BMC Infect Dis 14: 3.
147. Morre SA, van den Brule AJ, Rozendaal L, Boeke AJ, Voorhorst FJ, de Blok S,
Meijer CJ. 2002. The natural course of asymptomatic Chlamydia trachomatis infections: 45% clearance and no development of clinical PID after one-year followup. Int J STD AIDS 13 Suppl 2: 12-18.
148. Risser WL, Risser JM. 2007. The incidence of pelvic inflammatory disease in untreated women infected with Chlamydia trachomatis: a structured review. Int J STD
AIDS 18: 727-731.
149. Simms I, Horner P. 2008. Has the incidence of pelvic inflammatory disease following chlamydial infection been overestimated? Int J STD AIDS 19: 285-286.
150. Morrison RP. 2000. Differential sensitivities of Chlamydia trachomatis strains to inhibitory effects of gamma interferon. Infect Immun 68: 6038-6040.
55
151. Borges V, Nunes A, Ferreira R, Borrego MJ, Gomes JP. 2012. Directional evolution of Chlamydia trachomatis towards niche-specific adaptation. J Bacteriol
194: 6143-6153.
152. Jeffrey BM, Suchland RJ, Quinn KL, Davidson JR, Stamm WE, Rockey DD.
2010. Genome sequencing of recent clinical Chlamydia trachomatis strains identifies loci associated with tissue tropism and regions of apparent recombination. Infect
Immun 78: 2544-2553.
153. Akande V, Turner C, Horner P, Horne A, Pacey A, British Fertility S. 2010.
Impact of Chlamydia trachomatis in the reproductive setting: British Fertility Society
Guidelines for practice. Hum Fertil (Camb) 13: 115-125.
154. Ouburg S, Spaargaren J, den Hartog JE, Land JA, Fennema JS, Pleijster J,
Pena AS, Morre SA. 2005. The CD14 functional gene polymorphism -260 C>T is not involved in either the susceptibility to Chlamydia trachomatis infection or the development of tubal pathology. BMC Infect Dis 5: 114.
155. Mei B, Luo Q, Du K, Huo Z, Wang F, Yu P. 2009. Association of MICA gene polymorphisms with Chlamydia trachomatis infection and related tubal pathology in infertile women. Hum Reprod 24: 3090-3095.
56
Author Biographies
Shruti Menon
Shruti Menon received her B.Sc. (Honours) in Biotechnology from Monash University,
Malaysia in 2011. She is currently doing her PhD in Microbiology at Queensland University of Technology. Her project focuses on developing a novel peptide-based serological diagnostic for women with Chlamydia trachomatis -related infertility. Her current interests involve chlamydial diagnostics and mechanisms that lead to C.trachomatis
–related infertility in women.
Peter Timms
Peter Timms obtained his PhD from the University of Queensland, Australia in 1989 and was made a Fellow of the Australian Society for Microbiology in 1991. He joined Queensland
University of Technology in 1991 and rose to the level of full professor in 2003. He moved from QUT to University of Sunshine Coast, Australia in 2014 where he is Professor of
Microbiology. He has spent 25 years working on all aspects of Chlamydia, in both humans and animals. His team has made major discoveries in chlamydial genomics, evolution, vaccine development and basic mechanisms of pathogenesis.
John Allan
John A. Allan obtained his MB.BS from University of Queensland in 1973 and his fellowship in Obstetrics and Gynaecology in 1984. Associate Professor John Allan was director of
Reproductive Medicine from 1988 till 2014 at the Wesley Hospital Brisbane and is currently
Head of UnitingCare Health Clinical School and Director of Gynaecology at The Wesley
Hospital. Dr Allan is a member of the Society of Pelvic Surgeons and his areas of research have been in advanced laparoscopic surgery, investigation of the microbiome of endometrium, fallopian tubes and follicular fluid. Dr Allan developed a technique for freezing spermatozoa in the seminiferous tubule.
Kimberly Alexander
Kimberly E. Alexander is a Senior Lecturer within the School of Nursing at the Queensland
University of Technology, Brisbane, Australia. She is a registered nurse with a clinical background in oncology. She has a Bachelor of Nursing, Bachelor of Health Science (Public
Health), a Graduate Certificate in Academic Practice, a Masters of Education (Higher
Education) and a PhD in epidemiology. Kim has cross-disciplinary research experience in epidemiology, genetics, and nursing with a particular interest in patient-reported outcomes such as symptoms and quality of life.
57
Luk Rombauts
Luk Rombauts was awarded a PhD in 1993 from the University of Leuven, Belgium, and completed his general O&G training in 1996. He relocated to Australia in 1999 and successfully completed his subspecialty training in Reproductive Endocrinology and
Infertility in 2001. He was appointed as Monash IVF Research Director in 2001, Clinical
Director of Monash IVF (2003-2008) and a Monash IVF Company Board Member between
2010-2012. He is an Adjunct Clinical Associate Professor in the Department of Obstetrics and Gynaecology at Monash University. His main research interests include endometriosis and embryo implantation. He is an associate editor for Human Reproduction. Associate Prof
Rombauts is a Board Member of the World Endometriosis Society since 2008 and is the editor of the World Endometriosis Society's electronic Journal. In 2011 he was appointed to the World Endometriosis Research Foundation Board of Trustees and to the Board of the
Fertility Society of Australia.
Paddy Horner
Paddy Horner has been a consultant at Bristol in Genitourinary Medicine since 1994 and works at the Bristol Sexual Health Centre. In 2007 he was awarded a Walport Clinical Senior
Lectureship at the School of Social and Community Medicine, University of Bristol. He has long standing research interests in the epidemiology diagnosis and treatment of Chlamydia trachomatis, Mycoplasma genitalium, and non-gonococcal urethritis (NGU) on which he has published widely in peer reviewed journals.
Martin Keltz
Martin Keltz, a board certified endocrinologist, established WESTMED Reproductive
Services in 2015. Dr Keltz graduated from Harvard College in 1985, the NYU School of
Medicine in 1989, and completed his OB/GYN residency at NYU/Bellevue in 1993. Since completing his fellowship in reproductive endocrinology at Yale University in 1995, Dr Keltz has been director of reproductive endocrinology at St Luke’s and Roosevelt Hospitals, where is he now an associate professor at the Ican School of Medicine at Mt Sinai. He cares for couples challenged by infertility and recurrent miscarriage as well as women suffering with fibroids, endometriosis, or any reproductive disorder. His busy practise focuses on IVF, SHG,
IUI, and minimally invasive hysteroscopy and laparoscopy. Dr Keltz has been awarded the
“Top Reproductive Endocrinologist” in New York Magazine for the years 2012, 2013, and
2014. He has authored over 40 peer-reviewed articles and 50 abstracts in reproductive medicine.
Jane S Hocking
58
Jane S Hocking is an epidemiologist with a particular interest in the epidemiology and control of genital Chlamydia trachomatis. Dr Hocking is a Professor at the University of Melbourne,
Australia where she heads up the Sexual Health Unit in the Melbourne School of Population and Global Health. She obtained a Master of Public Health in 1998 and a PhD in 2005, both from the University of Melbourne. As part of her PhD, she generated Australia’s first population-based estimates of genital chlamydia prevalence among young women aged 18 to
25 years. She has subsequently provided Australia’s first estimates of chlamydia incidence and re-infection rates among young women. She currently leading a world first chlamydia screening randomised controlled trial of a chlamydia testing intervention in general practice that aims to determine whether chlamydia screening is cost-effective and should be introduced in Australia. She is also interested in treatment efficacy for chlamydia.
Wilhelmina M Huston
Wilhelmina (Willa) Huston is a senior lecturer at Queensland University of Technology. Her
PhD was completed at The University of Queensland (conferred 2004). She held a
Postdoctoral Fellowship in the UK at The University of York (2003-2005), and returned to
Australia in 2005 as Postdoctoral Fellow at Queensland University of Technology in the field of Chlamydia research (2005-2007). She held a NHMRC Peter Doherty Fellowship (2007-
2010), Lecturer (2011), and Senior Lecturer (2012) positions at Queensland University of
Technology. Dr Huston is interested in the molecular microbiology of the human intracellular pathogen Chlamydia, how we can better understand the pathogenesis mechanisms of this organism leading to better treatment and diagnosis. Dr Huston has been in the Chlamydia research field since 2005.
59
Fig. 1. The four major models of development of pathology associate with chlamydial infertility in women.
The figure shows the four models summarised here that are supported within the field by evidence from human studies.
Fig. 2. Summary of host and pathogen factors that have some evidence of contribution to the development of chlamydial infertility in women.
60
Summary
Chlamydia trachomatis is the most common bacterial sexually transmitted pathogen worldwide. The infection can result in serious reproductive pathologies including pelvic inflammatory disease, ectopic pregnancy, and infertility in women. However, the processes that result in these reproductive pathologies have not been well defined. Here we review the evidence for the human disease burden of these chlamydial reproductive pathologies. We present the four most widely accepted models of pathology development. We then review all of human based evidence that links Chlamydia with reproductive pathologies in women and how they support these models of disease. We present data supporting that host, immunological, epidemiological, and pathogen factors may all contribute to the development of infertility. Specifically, we review the existing evidence that host and pathogen genotypes, host hormone status, age of sexual debut, sexual behaviour, co-infections and repeat infections are all likely to be contributory factors to development of infertility. Pathogen factors such as infectious burden, treatment failure and tissue tropism’s or ascension capacity are also potential contributory factors. We highlight the limitations to the evidence and propose future studies that could be beneficial to improve understanding of how chlamydial infertility in women occurs and possible future interventions to reduce this disease burden.
Table 1: Summary of genotypes that have been significantly associated with chlamydial infection or pathology
61
Locus
TLR1
(RS5743618) TT
TLR2
-16934 T>A
(rs4696480)
+2477 G>A
(rs5743708)
TLR4
Rs1927911 CC allele
CD14 -260C>T
Study parameters
Prospective recruitment
PEACH PID study:
PCR confirmed CT negative women with PID n=111
PCR confirmed CT positive women with PID n=94
Fertility clinic:
CT IgG negative women with
Tubal pathology n=17)
CT positive women without tubal pathology n=13
CT IgG positive women with tubal pathology n=26 (CT status MIF test titre >1:32)
Sexual Health Clinic:
CT IgG positive women n=147
CT IgG positive asymptomatic women n=81
CT IgG positive symptomatic women n=66
CT IgG negative women n=
321
Prospective recruitment
PEACH PID study: CT negative (PCR) women with
PID n=111
CT positive (PCR) women with PID (n=94) a
Whole blood from healthy females n=44
Distribution of TNF-α allele among male and female participants in Taiwan (TT n=26, CT, n=36, CC n=22) b
Dutch women Caucasian origin, CT positive test determined by MIF with a titre
≥1:32.
Significance
TT increased risk of developing PID with chlamydial infection
(Adjusted Odds ratio: 2.8
95% CI 1.3-6.2; P=0.008)
Individual SNPs not significantly associated with infection, risk, symptom or infertility
Haplotype: (-16934A with
+2477G) higher women with CT but not tubal pathology (P=0.015;
OR:0.28; 95% CI: 0.1-
0.75), and decreased proportion when women ranked from asymptomatic to symptomatic infections to CT+ and tubal infertility
CC allele significantly associated with being chlamydial positive in PID participants (P=0.002)
TT allele associated with significantly higher TNFproduction when whole blood stimulated with C. trachomatis P<0.05
(relatively minor differences in actual concentration)
No significant difference
in the distribution of CD14
Ref
a
b
62
NLRP3
AG or AA at SNP rs12065526
STD clinic
CT IgG positive n= 135
CT IgG negative n=49
Subfertility clinic
CT IgG positive women n= 41
CT IgG negative women n =212
CT IgG positive with tubal pathology n=28
CT IgG negative women with tubal pathology n=22
Healthy control group n=170
Sexual health clinic: CT positive n=99, CT positive symptomatic n=44,
CT negative n=219,
CT negative symptomatic n=75
Healthy fertile control n = 93 polymorphism in STD or infertility cohort
MBL
High MBL2 producing genotypes
(HYA/HYA)
(HYA/LYA)
HLA class II allele
DRB1*1503
CT IgG positive women with
TFI n=76 (n=157)
CT IgG positive women without TFI n= 71(n=398)
Infertility clinic, Kenya.
CT IgG positive women with
TFI (MIF titre ≥1:16) n=33
AG or AA at SNP rs12065526 were at significant risk of developing abdominal pain when CT infected
(P=0.047, OR 2.9 95% CI
1.8-8.0) (not significantly associated with infection risk or tubal pathology)
High MBL2 producing genotypes (HYA/HYA)
(P=0.054; OR 3.72; 95%
CI=1.07-12.78) and
(HYA/LYA) (P=0.019;
OR=0.28; 95% CI=0.11-
0.75) higher in CT positive women as compared to CT positive TFI women.
MBL2 genotypes
(LXA/LXA) were higher in CT positive TFI women compared to CT positive women without TFI
(P=0.025; OR 2.34;
95%CI 1.17-4.69)
DRB1*1503 detected in 7
TFI women who were CT negative and absent in CT
63
DRB5*0101 CT IgG negative women with
TFI n=37
Cytokines
IL-10 1083AA
TNF-
-308A
IL-12B rs3212227 AC
Il-10 1082A
Major histocompatibility complex class I chain related A
(MICA) a
Infertility clinic at Helsinki
Infertile women n=114
Fertile control n=176
CT IgG positive women with
TFI (MEDAC ELISA kits) n=
96 b
TFI n=100
Pregnant fertile controls n=125
CT IgG positive with TFI n=94
CT IgG negative with TFI n=
69
CT cHSP60 IgG positive with
TFI n=90
CT cHSP60 IgG negative with
TFI n=73 c
TFI from IVF clinic, Helsinki n=47
CT IgG antibodies n=23
Infertility Clinic China-
TFI women n=63
Non TFI=151
CT IgG positive women with
TFI (determined by commercial immunoassay kits) n= 42
CT IgG positive women without TFI n=59 positive TFI women
(P=0.01; OR 0.05; 95%
CI=0-0.7).
DRB5*0101 was more common in TFI CT seronegative than TFI CT seropositive (P=0.05;
OR=0.2; 95% CI=0.02,1) a
IL-10 increased the risk of tubal damage in CT positive women (OR 7.3,
95% CI 1.3-4.2) a
TNF-
increased the risk of tubal damage in CT positive women (OR 4.0,
95% CI 1.0-16) b
IL-12B AC heterozygote increased risk of chlamydial tubal factor infertility (OR 2.44; 95%
CI 1.23-4.87) c
Il-10 1082A allele frequency higher in CT positive TFI cases than CT negative TFI cases (0.72 vs 0.46; P=0.01)
MICA *008 higher in infertile patients without
CT infection than infertile women with CT infection
(P=0.00367; OR=2.14;
95% CI=1.4-3.28)
MICA allele confers protection against CT tubal infertility. a
b
c
64
Fig 1
65
Fig 2
66
Menon Bio pic
67
Timms Bio pic
68
Allan Bio pic
69
Alexander Bio pic
70
Luk Rombauts Bio pic
71
Horner Bio pic
72
Keltz bio pic
73
Hocking bio pic
74
Huston bio pic
75