a doubly-labelled water study
advertisement

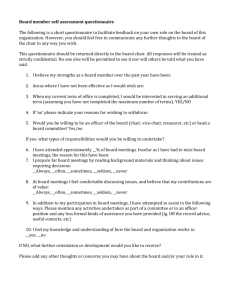
O34 CAN A QUESTIONNAIRE ESTIMATE METABOLIC RATE IN CKD ? A DOUBLY-LABELLED WATER STUDY Vilar, E1,2. Sridharan, S1,2. Wong, J1,2. Machado, A1. Summerhayes, B1. Farrington, K1,2 1 Lister Renal Unit, Stevenage, UK, 2Department of Postgraduate Medicine, University of Hertfordshire, UK BACKGROUND: Assessment of energy requirements in patients with CKD is usually performed with algorithms derived from normal individuals that are not validated in CKD. Patients with CKD often demonstrate evidence of malnutrition requiring dietetic input and estimation of Total Energy Expenditure(TEE) using simple tools is required. We set out to determine whether an established 7 day recall questionnaire for physical activity is able to predict TEE in patients with CKD by validating it against a gold-standard measure, the doubly-labelled water isotope-excretion technique. METHODS: 80 clinically stable subjects with CKD 1-5 from our unit underwent a two week metabolic study whereby their TEE was measured over 14 days using doubly-labelled water after ingestion of 18-O and 2-H enriched water doses. The Stanford 7 day recall questionnaire was used to assess physical activity level and for each block of time Metabolic Equivalent of Task(MET) was estimated. All patients underwent whole body bioimpedance analysis to estimate body composition and indirect calorimetry at rest using an overhead canopy. TEE was calculated from the doubly-labelled water technique(TEEDLW) using standard methodology. In addition, TEE was calculated from the Stanford questionnaire using four methods: Method 1: Average MET over the 7 day period was multiplied by an equation for Resting Energy Expenditure specific to patients with renal disease1. Method 2: For each time block metabolic rate was calculated by assuming a typical 1MET=3.5ml 02/kg/min and 200ml 02=1kCal2. Method 3: For each time block metabolic rate was calculated assuming that 1MET= predicted resting V02(ml 02/kg/min) based on a bioimpedance fat mass algorithm3. Method 4: For each time block it was assumed that 1MET=resting V02 (ml 02/kg/min) as measured by indirect calorimetry. We compared the relationship of gold-standard TEE (TEEDLW) against TEE from the Stanford questionnaire using each of the methods above by correlation and also the Bland-Altman technique. RESULTS: Mean subject age was 56.7±SD16 years and 60% were male. 40 patients had CKD stage 4-5 and 40 stage 1-3. Mean daily MET was 1.35±SD0.3 using the Stanford 7 day questionnaire and indirect-calorimetry measured resting VO2 had a mean of 2.9±0.4ml 02/kg/min. The Pearson correlation(r2) of TEEDLW with each of the four methods of calculating TEE from the Stanford questionnaire above was 0.24, 0.19, 0.24 and 0.32 respectively(p<0.001 for each). The optimum method (4) which utilised measured resting V02 was compared to TEEDLW with Bland-Altman technique and had bias -29.7±SD kCal and limits of agreement 1195kCal to +1136kCal. CONCLUSION: In keeping with previous data, physical activity level in this CKD population was strikingly low. We were able to compare a gold-standard measure of TEE with that calculated from the Stanford 7 day recall physical activity questionnaire data using various methods. The particular calculation used to convert Stanford questionnaire data into TEE appears to be important and the best methods relied on indirect calorimetry to estimate resting V02 or bioimpedance fat mass to predict resting VO2. Method 4 explained 32% of the variance in TEE but with disappointing limits of agreement, though without significant bias. If questionnaires are to be used to calculate TEE in the CKD population then they are likely to need modification to capture low levels of physical activity not measured by the Stanford questionnaire. If MET is used to calculate TEE then consideration should be given to the method used to calculate the energetic equivalence of 1MET as mean resting VO2 for our population was relatively low at 2.9ml 02/kg/min (typical normal value=3.5).