Midterm
advertisement

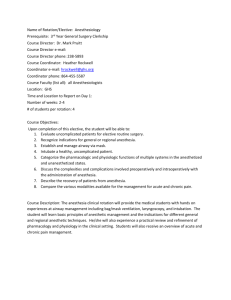
Stevie Willett 1 Midterm Midterm VETE 4335 Equine Anesthesiology/Nursing Stevie Willett Stevie Willett 2 Midterm While administering anesthesia, it is very important that the veterinary technician monitor the patient closely. This is to prevent an over dose of the anesthetic drug and to prevent patient death. To properly monitor a patient under anesthesia, the technician must have knowledge and experience recognizing each stage of anesthesia. A thorough understanding of the stages will help the technician determine if the patient is too deep or light under anesthesia thus allowing the technician to determine what adjustments should be made to keep the patient maintained at the proper plane of anesthesia for surgery. There are four stages of anesthesia with the third stage being further broken down into four planes. During the first stage of anesthesia the patient will begin to lose consciousness. During the time that the patient is losing consciousness disorientation, excitement, or fear may occur causing the patient to become difficult to handle. Additionally, the patient’s heart rate and respiration rate will increase. After the patient has past stage one the patient will slip into stage II of anesthesia. Stage II is called the excitement stage. Heart rate and respiration rate are still increased with the respiration rate being slightly irregular. The patient’s reflexes may become exaggerated, struggling or paddling may occur. The patient’s pupils will dilate and a nystagmus will be present. It is best if a patient passes through stage II fast during induction of anesthesia. A patient will pass through stage I and stage II faster with injectable anesthesia rather than masked gas anesthesia during induction. Stage III is the next stage a patient should enter. Stage III is divided into four planes. Stage III, plane I is indicated when the eyes rotate ventrally or a slight nystagmus will be present and a palpebral reflex should be present. The respiration rate should be more regular at this time. The patient may also swallow in this plane. At this plane the patient will be considered to be under light anesthesia and may move or have an increase in heart rate, respiration, or blood pressure with surgical stimulation. Stage III, plane II is indicated when the Stevie Willett 3 Midterm heart rate, respiration, and blood pressure is mildly decreased. The patient’s pupil size is moderate and the eyes will rotate ventromedial. Surgical stimulation may elicit a mild increase in heart rate and respiration from the patient. The patient will not have a swallow reflex at this plane. Stage III; plane II is the ideal anesthetic stage and plane in which to have a patient when performing surgery. Stage III, plane III is indicated by a significant decrease in heart rate and respiration a patient. The patient’s eyes will rotate to the central position and pupil size will become moderate. This plane is considered to have the patient too deep. If the patient continues to become deeper under anesthesia, they will pass into stage III, plane IV. Stage III, plane IV is considered to be an early anesthetic overdose. This plane is indicated by a dramatic drop in heart rate and blood pressure. The mucous membranes will appear pale rather than pink in color. The patient may also exhibit abdominal breathing. As the patient becomes deeper under anesthesia they will finally pass into stage IV. Stage IV is noted by a cessation of respiration followed by death a patient. When administering anesthesia to a patient there are several steps taken as the anesthetist to get the horse to a surgical plane of anesthesia. For describing the steps that I took to get to the proper plane of anesthesia, I will be using a patient that recently underwent arthroscopic surgery of the right hind tarsocrural joint of the tarsus. The patient was a 9 year- old warmblood mare. The mare became acutely lame in the right hind after becoming tangled in a lunge line. The mare presented with a swollen right hind tarsus, 3/5 lame. Treatment involved a sweat bandage to reduce swelling. The next day the veterinarian performed an arthrocentesis and an ultrasound. A large amount of fibrin and excess joint fluid was noted to be in the tarsocrural joint of the tarsus during the ultrasound exam. The patient was started on oral antibiotics (enrofloxacin) and NSAID (phenylbutazone). When no improvement was seen in the patient, an arthroscopy with a Stevie Willett 4 Midterm sterile joint lavage was performed in the tarsocrural joint. The first steps that were taken begin prior to induction. The patient was given phenylbutazone prior to induction to control pain level which aids in a smoother induction and recovery. Once the patient’s pain level was controlled the patient was sedated with xylazine (100mg/ml) and butorphanol (10mg/ml), and then allowed to become sedate in the induction area of the surgery room. The room was made quiet during this time to minimize the patient from becoming stimulated. Once the patient became sedated (head to the knees) the induction drug was given (ketamine 100mg/ml and midazolam 5mg/ml). The patient then passed from stage I to stage III, plane I quickly. Once the patient was unconscious it was placed in lateral recumbency with the head and neck stretched out. A gag was placed between the incisors and the tongue was moved out of the way. The sterilely lubricated endotracheal tube (ETT) was advanced through the mouth gag and advanced easily into the trachea. The patency of the endotracheal tube was checked with a slight press on the thorax to verify air coming out of the endotracheal tube. The endotracheal tube cuff was inflated appropriately. The patient was then hoisted on to the surgery table as the veterinarian wanted in dorsal recumbency. As the anesthetist, the ETT was guarded to maintain an open air way. Once positioned the patient was then connected to the anesthesia machine that administered isoflurane and oxygen. Oxygen flowmeter was adjusted to 5L/min and isoflurane was adjusted to 2%. Mechanical ventilation was also started on the patient at 8-10 breaths a minute. The patient was next connected to IV fluids and a monitor that reads the ECG, arterial blood pressure, pulse oximetry, and end tidal CO2. An arterial line was placed for invasive blood pressure monitoring. The blood pressure transducer was zeroed prior to connecting to the patient. The patient’s heart rate, respiration, eye position and palpebral reflex, mucous membrane color, CRT, and mean arterial blood pressure were then evaluated. The patient’s eye position was in a ventromedial Stevie Willett 5 Midterm position and no nystagmus was present. Heart rate was auscultated at 32-36 beats per minute. Mean arterial blood pressure read at 68-70 mmHg. As an anesthetist I felt that the patient had reached the surgical plane of anesthesia. At this time the breaths per minute were decreased to 67 on mechanical ventilation. Patient vitals were monitored and documented every 5 minutes throughout surgery. Only minor adjustments to respiration rate or isoflurane were made to maintain the patient at the surgical plane of anesthesia. Dobutamine (62.5mg/250ml LRS), was given as a constant rate infusion (CRI) (1µg/kg/min) was occasionally used to keep the patient’s mean arterial blood pressure at or above 70mmHg. Once the surgeon was nearing the end of the procedure (about 10 min until done) steps were made to lighten the patient to ready for recovery. Small adjustments (0.5%) were made to decrease the percent of isoflurane over several minutes. Once the isoflurane was off, breaths per minute were decreased (2-4 breaths per minute) to stimulate the patient to breath on own. After a few minutes the patient began to breathe on own and was disconnected from the anesthesia machine at that time. The patient was rolled into the padded recovery room, hoisted then place in left lateral recumbency. The lower fore-limb was stretched forward to prevent radial nerve damage. Once in the recovery room the patient developed a nystagmus and began to swallow. The endotracheal tube cuff was deflated and removed. The patient was visualized to ensure a patent airway was present after removing the endotracheal tube. The patient was then administered romifidine (10mg/ml) IV to help keep the patient sedate and calm while passing through stage 2 and 1 of anesthesia during recovery. The patient had an uneventful recovery. Safely anesthetizing and monitoring horses under anesthesia can be tricky and stressful if a technician has little experience. In regards to anesthetizing patients I think it is very important for technicians to receive in-depth training by an experienced veterinarian or technician in all Stevie Willett 6 Midterm anesthetic and monitoring equipment. When it comes to changes that I would like to see in my clinic regarding anesthetizing patients, I would like the new incoming technicians to understand the importance of monitoring clinical signs more during anesthesia. I find that many technicians rely heavily on monitoring equipment rather than their own personal clinical skills and experience. I think it important for them to know that monitoring equipment should be used as an adjunct tool only rather than fully relied upon as the only means of patient monitoring. Equipment can malfunction and often does when needed most. Technicians need to recognize that the best kind of patient monitoring is their clinical skills and educated judgment when making decisions regarding appropriate changes required for patient safety and well-being. Stevie Willett 7 Midterm References: Thomas, John A. and Lerche, Phillip. (2011). Anesthesia and Analgesia for Veterinary Technicians (4th ed.). St. Louis, MO: Mosby Elsevier.