Hypovolaemic shock
advertisement

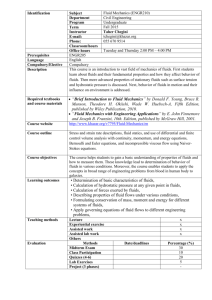
Hypovolaemic shock r/t bowel obstruction Debriefing/Guided Reflection Condition Overview: Hypovolaemia occurs when loss of extracellular fluid volume exceeds the intake of fluid. It occurs when water and electrolytes are lost in the same proportion as they exist in normal body fluids, so that the ratio of serum electrolytes to water remains the same. Hypovolaemia should not be confused with dehydration, which refers to loss of water alone with increased serum sodium levels. Hypovolaemia may occur alone or in combination with other imbalances. Unless other imbalances are present concurrently, serum electrolyte concentrations remain essentially unchanged. Causes: Hypovolaemia results from loss of body fluids and occurs more rapidly when coupled with decreased fluid intake. Causes include abnormal fluid losses such as those resulting from diarrhoea, GI suctioning, sweating, and decreased intake, as in nausea or inability to gain access to fluids. Causes also include third-space fluid shifts, movement of fluids out of the vascular system (trauma), or oedema formation resulting from burns, or ascites resulting from liver dysfunction. Signs and symptoms: Acute weight loss, weakness, Decreased skin turgor Oliguria, Concentrated urine, increased BUN creatinine Postural hypotension, Weak, rapid heart rate Flattened neck veins Increased temperature Cool, clammy skin, muscle weakness and cramps Management of care—nursing interventions include: Three goals exist in the emergency treatment of the patient with hypovolemic shock as follows: (1) maximize oxygen delivery - completed by ensuring adequacy of ventilation, increasing oxygen saturation of the blood, and restoring blood flow, (2) control further fluid loss, (Simulation in Nursing Education) Scenario Estimated scenario time: 15 minutes Guided reflection time: 15 minutes Target group: year 3 nursing students Brief summary: This case is a 45 year old male patient to a surgical ward in your hospital for acute appendicitis 48 hours ago. An acute appendectomy was performed and the client has failed to gain normal bowel sounds after the surgery. He is now complaining of abdominal pain, inability to pass flatus, and dizziness. The student will be expected to follow the standard protocols for the treatment of hypovolaemic shock. LEARNING OBJECTIVES: General: Identifies the primary nursing diagnosis (fluid volume deficit R/T fluid shifts in bowel obstruction) Implements risk assessment—what kinds of shock could this be? Hypovolaemic, septic, cardiogenic? Implements patient safety measures Evaluates patient assessment information including vital signs, pain, and abdominal assessment Implements therapeutic communication with team and in ISBAR format Demonstrates effective teamwork Prioritises and implements doctors instructions appropriately Scenario specific: Tips bed into reverse trendelenburg to ↑BP Shows ability to identify appropriate assessments which may help with differential diagnosis (e.g. abdominal assessment, fluid volume assessment) Able to begin volume resuscitation (either 2L .9NS or 500ml colloid with recheck of BP for effect Initiates check of fluid balance for last 24 hours AUT S1 2014 Report to student Patient Overview: Thomas Jones is a 45-year-old male developed RLQ abdominal pain about a week ago which waxed and waned. About 72 hours ago the pain became acute and sharp and he presented to the emergency department where acute appendicitis was diagnosed. He underwent an acute appendectomy 48 hours ago, at which time surgeons discovered that his appendix had ruptured. It was removed, his abdomen flushed, and he was sent to your ward for recovery. Patient data: male, age 45 years, weight 78Kg, height 1.75 metres DOB: 19-07-XX Hospital ID number: 987654 Past medical history: Thomas has a history of a broken arm as a child, tonsillectomy at age 13. He is not currently on any medications except vitamins and has no allergies. Recent medical history: Has been really ‘pushing’ himself lately and feels the ‘stress’ is starting to get to him. He went out for dinner 3 nights ago and found he was so unwell he was having difficulty eating or drinking. He was having nausea and acute RLQ pain at this time. and (3) fluid resuscitation. Also, the patient's disposition should be rapidly and appropriately determined. Obtaining lab values: o Serum urea, serum creatinine: Volumedepleted individuals show serum urea elevated out of proportion to the serum creatinine level (ratio greater than 20:1). o Haematocrit higher than normal as RBCs suspended in decreased volume. o Monitor K+ and Na+ levels as they may be reduced or elevated. Two large-bore IV lines should be started. Fluid balance every 4 hours with vital signs hourly Assess daily weights and record Skin turgor and mucous membrane assessment q8hrs Administer fluids or plasma expanders to replace fluids lost or shifted into intravascular space Place bed in reverse trendelenburg position until BP is up over 100 systolic, then flat until boluses completed and BP stable at over 120 systolic. Hypovolaemic Shock - Resources Equipment checklist Equipment to have in the room for this scenario: Standard precautions equipment Stethoscope Blood pressure cuff SpO2 monitor and probe Thermometer ECG monitor and leads Oxygen supply source Oxygen delivery devices (nasal cannula, mask, and ambu bag) Medication and fluids: Normal saline 1000ml infusing at 75ml/hour Tramadol 50-100mg po prn pain Maxalon 10mg po prn for nausea Documentation forms: Doctors instructions/DHB protocols Observation record, medication sheet, nursing notes Fluid balance chart Diagnostic equipment: Nursing Anne: Location: Surgical ward Dress Anne in male clothing Lying down in bed Secure ID band with patient name, DOB, and hospital ID number Student performance objectives Wear gloves Identify patient name from ID band (DOB, hospital ID number) Ask client what prompted him to ring bell Obtain BP, pulse, RR, Temp, SpO2 Place client in trendelenburg Assess pain utilising pain scale Do abdominal assessment Administer bolus IV fluids Monitor vital signs every 2-5 min. Call Registrar with ISBAR report at end of scenario Number of participants: 1 student—recorder and calling ISBAR ROLE 1 student—doing primary assessment, giving medications 1 student—Vital signs and airway management 1 student—play family role to improve team communication Potential nursing problems Acute pain related to bowel obstruction Defining characteristics: Verbal report Changes in BP, resp. rate, AP Fluid volume deficit R/T fluid shifts in bowel obstruction Abdomen hard to palpation Fluid balance In=2100ml Out=300ml last 24 hours Postural hypotension shift of > 20 beats in pulse, and drop of 20 systolic points in BP when sitting Pain r/t increasing abdominal girth and lack of bowel sounds Abdominal girth increasing 20cm in last 4 hours Pain 8-9/10 with no relief with medication Hypovolaemic Shock - Scenario SIM MAN settings Patient/manikin actions Initial state (0-2 min.) Lung sounds: clear bilaterally Heart rate: 140/minute Abdomen: distended and hard Respiratory rate: 24/min. BP: 100/70 SpO2: 97% Hypovolaemia trend: HR: 160/min. Resp. rate: still 24/min. Student should do the following: Wear gloves BP: 90/50 Resp rate: 24/min. Cue: if student does not look at abdomen say, “My stomach is hurting so bad I can hardly stand it. They gave me something last night but nothing since about 10pm” Obtain vital signs & assess pain and abdomen Ask client if passing flatus or stool Last pain medication Do abdominal assessment Vocal sounds: “The pain is ‘10’ out of 10 now.’ I think there are black spots in front of my eyes. What is happening?” Take vital signs, note trending in BP and pulse Report values to recorder Vocal sounds: Eyes roll back and client groans. Patient becomes unconscious. Place bed in trendelenburg Give fluid bolus of 1 Litres .9NS Continue to take vital signs every 1-2 minutes to monitor effect of fluid bolus Continue to monitor vital signs every 2 minutes and report to recorder Role member to provide cue: primary care provider Communicate therapeutically with patient Cue (final orders): Transfer to ICU Monitor and record vital signs (BP, AP, SpO2,) every 2 minutes CALL ISBAR to physician requesting further orders Vocal sounds: “It feels like my abdomen is a block of cement. The pain is ‘8!’” Rates pain as ‘8’ on scale of 1-10 SpO2: to 97% Heart rate: 90/min. Role member providing cue: patient Identify patient and introduce self BP: 70/40 9-12 minutes Cue/prompt Temp. 37 C 3-6 minutes Student interventions Vocal sounds (after saline bolus):—“I feel a little better now.” Role member to provide cue: patient Cue: if nurse does not act, patient will say, “All I see are black spots! Please do something!” Call when blood results are available (Troponin-T, CK-MB, Myoglobin), BUN, creatinine, and HCT/HGB