as word document
advertisement

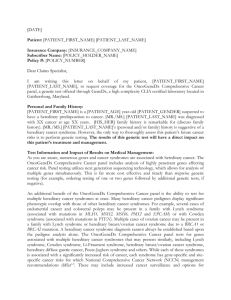
Letter of Medical Necessity Test Code 1325 <<Today’s Date>> <<Insurance Company Name>> <<Address 1>> <<Address 2>> <<City, State ZIP>> Regarding: <<Patient full name>> DOB: <<MM/DD/YYYY>> Subscriber ID: <<Member ID#>> Group ID: <<Group ID#>> Re: Request for prior authorization and coverage for Lynch Syndrome/HNPCC genetic testing. Billing is through <<billing institution>> with testing performed at PreventionGenetics, LLC. CPT codes for PreventionGenetics test code #1325 include: 81295, 81297, 81298, 81300, 81292, 81294, 81317, 81319, 81479 and 81403. The ICD 10 code(s) associated with the patient’s diagnosis include <<ICD code(s)>>. The ordering physician is <<Doctor’s Name>>, NPI#: <<NPI#>>. Lynch Syndrome As many as 2 to 4% of all colorectal cancers and 2 to 5% of all endometrial cancers are associated with Lynch Syndrome, also known as Hereditary Nonpolyposis Colorectal Cancer (HNPCC). Lynch Syndrome a hereditary condition caused by germline mutations in several DNA mismatch repair (MMR) genes including MLH1, MSH2, MSH6, PMS2 and EPCAM. Individuals with mutations in the inherited predisposition genes associated with Lynch syndrome tend to develop cancer at earlier ages, often with bilateral and/or multifocal tumors, with a high lifetime risk of cancer. Families with Lynch Syndrome generally have several family members affected with cancer across multiple generations. Although pathogenic variants in Lynch Syndrome genes are associated with a significantly increased risk for colorectal cancer, (40 -80% lifetime risk) and endometrial cancer (25-60%) additional cancers are seen with lower frequencies including ovarian, gastric, hepatobiliary, urinary tract, small bowel, sebaceous neoplasms, pancreatic and brain . 1 1,2 3 Diagnosis of an individual with Lynch Syndrome has significant effects on medical management. Gene specific medical management guidelines demonstrate the clinical utility of hereditary cancer predisposition testing. Published clinical management guidelines for Lynch Syndrome help to reduce the risk of morbidity and mortality in patients affected patients. Risk reduction strategies outlined in NCCN management guidelines include earlier, increased surveillance (i.e. annual or biennial colonoscopy beginning at age 25), surgical interventions (i.e. prophylactic hysterectomy and salpingo-oopherectomy); as well as screening for associated cancers via ultrasound, serum CA-125 testing, urinalysis, and annual physical and neurologic exams. 2 Personal History <<Personal Medical History: Include details of patient’s relevant medical history>> Family History <<Family History: Include list of relevant family history information if applicable. . Appropriate risk assessment models or limited history should be noted >> Based on published NCCN , Bethesda , and ACMG guidelines, the personal and family history of this patient warrants analysis of genes known to be associated with Lynch Syndrome. Testing of the 5 genes associated with this condition through the Lynch Syndrome NextGen Sequencing Panel and deletion/duplication analysis panel via aCGH is the most comprehensive, cost-effective way to evaluate for Lynch Syndrome. 2 4 5 The laboratory providing the genetic testing is PreventionGenetics, LLC, (Tax ID: 83 0343803) who is a sponsor of Pediatric Lab Utilization Guidance Services (PLUGS®). PreventionGenetics is committed to providing comprehensive, high quality, and affordable genetic testing that adds value to patient care. Through utilization management strategies at PreventionGenetics, over 1.3 million healthcare dollars are saved annually. I am hopeful that we can work together for <<Mr/Mrs/Ms/Miss patient’s last name’s>> benefit. Please contact me at <<Phone #>> with the result of this prior authorization and/or if you need additional information. Sincerely, <<Name, credentials>> <<Title>> <<Institution>> References 1. 2. 3. 4. 5. Jasperson, et al. Gastroenterology, 2010. 138(6): 2044-2058 NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines ). Genetic/Familial High-Risk Assessment: Colorectal. Version 2.2015, 10/07/2015. Jang E. Gut and Liver. 2010; 4: 151 Umar A, Boland CR, Terdiman JP, et al. Revised Bethesda Guidelines for Hereditary Nonpolyposis Colorectal Cancer (Lynch Syndrome) and Microsatellite Instability. Journal of the National Cancer Institute. 2004;96(4):261-268. Hedge, et al. Genet Med, 2014. 16(1):101-116 ®