Admission into the BMed MD
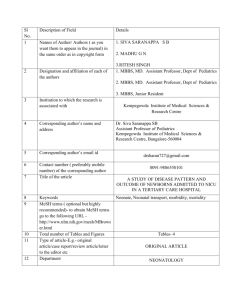
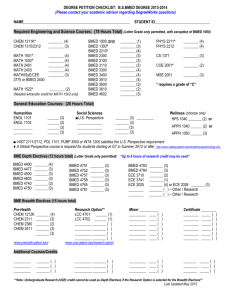
advertisement

BMed MD PROGRAM PROPOSAL Background The current Medicine program is a 6 year undergraduate entry program leading to the MBBS. There is a first year intake of approximately 276 students including 68 international students. There is also a graduate entry pathway for a limited number of students (approximately 15) from the BMedSc at UNSW. These students complete BMedSc Honours before transferring to complete the final three years of the MBBS program. Several Australian medical schools have either implemented or announced their intention to award a MD instead of the MBBS. It is anticipated that all Australian medical schools will eventually adopt the MD to maintain consistency within Australian and offer a more internationally recognisable qualification. This proposal has been developed to ensure compliance with the Australian Qualifications Framework (AQF) and the Higher Education Standards Framework. It does not involve any major restructuring of the current MBBS curriculum. Bachelor of Medical Studies (BMed) /Doctor of Medicine (MD) The proposed Medicine program will lead to the awarding of two degrees: The Bachelor of Medical Studies (BMed) would be based on the first three years of the existing MBBS curriculum including Phase 1 courses and the Integrated Clinical Studies courses in Phase 2. The Doctor of Medicine (MD) would be based on the Independent Learning Project (ILP) and Phase 3. It should be noted that the use of the term Doctor of Medicine (MD) is consistent with the AQF definition of a Masters Degree (Extended). The AQF permits the use of the title “Doctor of Medicine (MD)” for graduates of a Masters Degree (Extended) in Medicine. The structure of the integrated program is shown in Figure 1. The shaded areas in each two-year block reflect the existing three phases in the MBBS program. There are no changes to existing courses. It is essential that the two degrees are considered as an integrated program. The BMed would only be awarded with the MD – it would not be awarded as a standalone degree (see below under Exit Degree). 1|Page BMed Year 1 • Foundations (12 UoC) • Beginnings, Growth & Development A (12 UoC) • Health Maintenance A (12 UoC) • Ageing & Endings A (12 UoC) Year 2 • Society & Health (12 UoC) • Beginnings, Growth & Development B (12 UoC) • Health Maintenance B (12 UoC) • Ageing & Endings B (12 UoC) BMed • Phase 2 Integrated Clinical Studies A (24 UoC) • Phase 2 Integrated Clinical Studies B (24 UoC) BMed Year 3 MD • Independent Learning Project (30 UoC) • General Education (12 UoC) • Clinical Transition (6 UoC) Year 4 MD • Phase 3 Clinical Courses; 5 courses (10 UoC per course) Year 5 MD • Phase 3 Clinical Courses; 3 courses (10 UoC per course) • Elective Course (8 UoC) • Preparation for Internship (8 UoC) Year 6 FIGURE 1: BMED MD PROGRAM STRUCTURE 2|Page Bachelor of Medical Studies (BMed) The Bachelor of Medical Studies (BMed) comprises the courses currently delivered in Phase 1 and Phase 2 of the MBBS program. These courses are unchanged. The specifications of the AQF for a Bachelor Degree (Level 7 qualification) would be clearly addressed in the BMed. The existing graduate capabilities for students completing Phase 1 and the Integrated Clinical Courses of Phase 2 would ensure that students meet learning outcomes in relation to knowledge, skills and application of knowledge and skills at this level. The depth requirement of the Bachelor Degree would be in the discipline of clinical sciences. The volume of learning (i.e. 3 years) is consistent with the AQF. It is noted the General Education requirements are actually met in Year 4 while students are completing the ILP. This is consistent with the current structure of the MBBS and is a consequence of the allocation of UoC in the Phase 1 courses (12 UoC per course) and the Phase 2 courses (24 UoC per course). It is also the most appropriate time in the program for students to complete GE courses as the ILP is not full-time and there is greater flexibility to allow scheduling of GE courses. As the BMed would not be conferred until completion of the MD, the students would have met the GE requirements. Doctor of Medicine (MD) The MD comprises the Independent Learning Project (ILP), the Clinical Transition course and the Phase 3 courses. The GE courses are also counted within the period of the MD. The AQF specifies expectations of graduates of a Masters Degree (Extended) within three broad categories – knowledge, skills and application of knowledge and skills. The descriptors for each category relate to professional practice and research. The ILP clearly addresses the requirements of the Masters Degree (Extended) in acquiring “knowledge of research principles and methods applicable to the discipline and its professional practice”, and acquiring “cognitive, technical and creative skills to investigate, analyse and synthesise complex information, problems, concepts and theories and to apply established theories to different bodies of knowledge or practice”. The ILP requires students to undertake a research project in which they review existing literature on the area of study, formulate a hypothesis for testing, design the study, address ethical implications of the study, collect and analyse data and report their findings. In addition to undertaking supervised research, the ILP also includes coursework on research methodology in both quantitative and qualitative research projects, statistical analyses and scientific writing. The ILP is assessed by a written literature review, supervisor’s continuous assessment and a final written report (in the form of a manuscript) which is assessed by the supervisor and an external examiner. The learning activities and forms of assessments in the Phase 3 clinical courses, which are closely aligned to the program’s graduate capabilities, ensure that graduates will have met the expectations of a Masters Degree (Extended). All courses are based on an experiential approach to learning in which students are placed in clinical services and required to participate in the professional activities of the clinical unit. The nature and diversity of clinical placements in Phase 3 require students to apply knowledge and skills to new situations across a range of clinical disciplines and settings. The strong focus on self-regulated learning in Phase 3 necessitates a high level of personal autonomy in 3|Page learning. The need for students to complement the prescribed evidence in their portfolio with their own initiatives to document learning similarly ensures a high level of personal accountability. While it could be argued that the experiential nature of all courses in Phase 3 provides a capstone experience for students to apply the knowledge and skills acquired in Phases 1 and 2, the final Preparation for Internship course clearly meets this requirement. Course assessments in Phase 3 are based on practice activities and include supervisor’s reports (based on learning plans which may include additional negotiated learning objectives) and observed application of knowledge and skills (based on mini-clinical skills assessments and case-based discussions). Near the end of Phase 3, students sit the Phase 3 Integrated Clinical Examination which is a high-stakes, summative examination comprising a written examination, clinical skills examination and a structured oral examination. Each component of the final examination is designed to assess the application of knowledge and skills. The students also submit their portfolio for review at the end of Phase 3. The portfolio comprises evidence collated by the student as they progress through Phase 3 to document their development in each of the eight graduate capabilities. In accordance with the Higher Education Standards Framework, all teaching staff in the MD are appropriately qualified in the relevant discipline (by either possessing postgraduate degrees or having appropriate professional experience). The 3 year duration of the MD is acceptable within the AQF as it follows a 3 year Bachelor (level 7 qualification) in the same discipline. Admission into the BMed MD The predominant pathway for entry into the program would remain first-level entry students from high school. The proposal does not change the existing processes for selection into Medicine nor the number of students selected into Medicine. A single code would be offered through UAC for application to the BMed MD program. Students selected into the program would enrol in both degrees. From the outset the students would be classified as medical students and be registered with the Medical Board of Australia and be required to adhere to the requirements of the NSW Ministry of Health for medical students training in teaching hospitals. Students who are offered a bonded position would be advised that the period of bonding would be based on the 6 years to complete both degrees. Graduate Entry Pathway Students entering the new program via the graduate entry pathway will have completed the BMedSc (Hons) Degree and will then complete the Phase 2 Integrated Clinical Courses and Phase 3. As these students already have achieved the desired learning outcomes relating to independent research in the Honours degree, their learning in the MD will focus solely on practice related learning. The graduate entry pathway leading to the BMedSc (Hons) MD is shown in Figure 2. 4|Page BMedSc •Core and elective courses in BMedSc Years 1-2 BMedSc •Prescribed elective courses in Anatomy, Pathology, Microbiology or Pharmacology •General Education courses Year 3 •BMedSc (Honours) •Foundations in Public Health BMed Sc (Hons) •Introductory Clinical and Communication Skills Year 4 MD •Phase 2 Integrated Clinical Studies A (24 UoC) •Phase 2 Integrated Clinical Studies B (24 UoC) Year 5 MD •Phase 3 Clinical Courses; 5 courses (10 UoC per course) Year 6 MD •Phase 3 Clinical Courses; 3 courses (10 UoC per course) •Elective Course (8 UoC) •Preparation for Internship (8 UoC) Year 7 FIGURE 2: BMEDSC (HONS) MD PROGRAM STRUCTURE Combined Medicine/Arts program Currently the combined MBBS/BA requires students to complete 96 UoC in Arts courses. This can be completed in 7 years providing students complete the ILP in an area relevant to medical humanities so as the ILP can be counted towards both degrees. As the ILP counts 24 UoC in the Arts degree, Medicine students only need to complete an additional 72 UoC in Arts courses which is typically done with an additional year of study and overloading. Although the ILP will sit within the MD, it will still be counted towards the requirement of the BA if it is completed in an area relevant to medical humanities. Accordingly students who wish to complete 5|Page combined Medicine/Arts program could complete the Arts requirement within the current time expectations. Note that the BA would not be conferred until completion of the BMed MD as currently applies with the MBBS. The typical structure for students in the combined program is shown in Figure 3. BMed •Phase 1 courses (96 UoC) Years 1-2 BMed •Phase 2 Integrated Clinical Studies A (24 UoC) •Phase 2 Integrated Clinical Studies B (24 UoC) Year 3 BA •Arts courses (48 UoC) Year 4 BA MD •Arts-focused ILP (24 UOC) •Arts courses (24 UOC) •Clinical Transition (6 UOC) Year 5 MD •Phase 3 Clinical Courses; 5 courses (10 UoC per course) Years 6-7 FIGURE 3: BA BMED MD PROGRAM STRUCTURE 6|Page Honours Currently students in the MBBS program may graduate with a BSc (Med) Honours and MBBS Honours. BSc (Med) Honours Students apply, on the basis of academic merit, to complete a BSc (Med) Honours degree in Year 4 instead of the ILP. Students who have completed the BSc (Med) Honours would be exempted from the ILP component of the MD. This is consistent with the AQF framework which specifies that the volume of learning for Masters Degree can be reduced if it follows an Honours qualification. The students would still be required to complete the general education courses and the Clinical Transition course. Students considering applying to do BSc (Med) Honours are advised to complete general education requirements prior to Year 4. After completing the BSc (Med) Honours, these students would progress into Phase3 to complete the MD. Medicine Honours Currently students are awarded MBBS Honours based on aggregate performance across the whole program. As this is no longer in alignment with the AQF, it is proposed that students be awarded Pass with Distinction if they have achieved a weighted average mark of at least 75% in the BMed MD. Exit Degree As noted above the BMed will only be awarded to students who complete the MD. There are a small number of students (typically 1-2 each year) who exit the Medicine program either voluntarily or as a result of failing to progress after completion of Phase 1. Currently students who exit the MBBS program prior to the end-of-Phase 1 examinations do not obtain a qualification. Students who have successfully completed all the Phase 1 courses but who exit as a result of failing the end-of-Phase 1 examinations or exit subsequently in Phase 2 or Phase 3 may apply to transfer to the BSc (Med) program. Depending on the stage of transfer, the student is required to complete up to 48 UoC in biomedical science courses. In the BMed MD program, students who exit prior to completing the program will be allowed to transfer to the BSc (Med) program to complete up to 36 UoC in biomedical sciences courses. These students would also need to complete general education requirements. Transitional Arrangements Program changes The only structural change to the existing program is that all students would complete the ILP in Year 4 as part of the MD. This would necessitate a transitional period to shift from the current practice of splitting students in Year 3 into either the ILP or Phase 2 Integrated Clinical Studies. In order to achieve this with the lowest impact on students and the teaching staff, a three year transitional period will be implemented. The effect will be to increase the size of student enrolment in the 7|Page Phase 2 Integrated Clinical Courses by 15% in 2013-2015 which will affect students currently in Years 1-3. The effect on the size of student groups for campus-based teaching (lectures, laboratory classes, tutorial groups) will be limited because of the organisation of the Phase 2 Integrated Clinical Courses which splits the total student enrolment into four groups. However additional clinical training capacity will be sought through affiliated sites. Implications for current students The change to a BMed MD will not adversely affect the recognition of the current MBBS. While the change to the MD will progressively be introduced by medical schools throughout Australia, registered medical practitioners will be equally recognised by an MBBS or MD for several decades. The proposed program is based on the recognition that the current MBBS curriculum promotes approaches to learning in the ILP and in Phase 3 which fulfil the requirements of a MD. As noted, there are no changes to the curriculum other than a structural change to ensure that all future students complete the ILP within the MD component of the program. As such current students in the MBBS program will complete the requirements of the proposed BMed MD (though not in the proposed structure for half of the cohort which completes the ILP in Year 3). To avoid disadvantaging any current student, all current students (excluding Year 6) will be offered the opportunity to transfer to the BMed MD or continue and graduate with the MBBS. 8|Page