Student Document- Webquest - Bioinformatics Activity Bank
advertisement

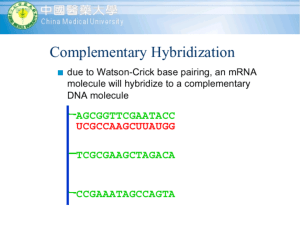
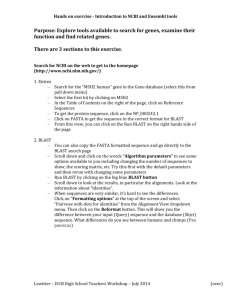
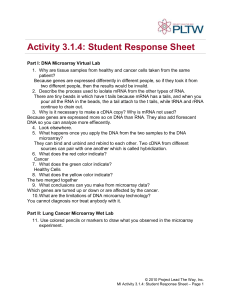
MEDICAL PROBLEM SOLVING INTRODUCTION The Clinic for Special Children in Lancaster County, Pennsylvania, is a nonprofit organization that specializes on the treatment of Amish and Mennonite children with rare metabolic disorders. Utilizing cutting edge biotechnology and bioinformatics, the doctors and geneticists at The Clinic have identified and described the molecular basis for several disorders. The ability of The Clinic to identify and diagnose affected children has drastically improved the incidence, as well as the quality of life, for these “special children” and their families. TASK Imagine that you work at The Clinic for Special Children. A young, Mennonite boy named John is brought to see you by his family. He is suffering from diarrhea, headaches, fatigue, a sore mouth and tongue, as well as tingling of the hands and feet. This combination of symptoms alone is inconclusive. Therefore, The Clinic must begin what can be called the “medical problem solving” process, in hopes of diagnosing and treating John’s disorder. ROLES In a problem solving team, there are two key individuals: 1. The Doctor – meets with the patient, records symptoms, observes and tests for other signs, provides diagnosis, prescribes treatment 2. The Geneticist – surveys the patient’s genome, identifies and sequences the hypothetical “problem gene,” runs a BLAST analysis of the gene sequence, identifies the mutation and biochemical implications Even though both members of the team have distinct roles in the problem solving process, it is important to remember the importance of collaboration in science. Choose the role that you feel suits you best. Now that you know your role, it is time to start the process of diagnosing and treating John. PROCESS – Listing Symptoms and Signs: The Doctor *As good clinical practice, take careful notes and be able to explain/describe all steps of the diagnostic process. Also, do not be afraid to consult your supervisor. When seven-year-old John and his family arrive at The Clinic, he is suffering from diarrhea, headaches, fatigue, a sore mouth and tongue, as well as tingling of the hands and feet. You also note that he is pale. As a doctor, these symptoms automatically cause you to form a list of possible conditions. Since you are not a real doctor, WebMD will help you formulate this list of possible conditions. Simply identify each symptom and answer questions if prompted to - always assume that the answer is either moderate or unknown. http://symptoms.webmd.com/symptomchecker Can you determine what John has? Keep this list of possible conditions open as a reference. Common doctor sense suggests that running a blood test is the next step. A complete blood count (CBC) test shows that John has low hemoglobin levels. Open a new window and go to MedicineNet to read about hemoglobin and conditions characterized by low hemoglobin levels. http://www.medicinenet.com/hemoglobin/article.htm Which condition from the WebMD generated list is characterized by low hemoglobin levels? Again, common doctor sense suggests that additional blood work needs to be done to determine the cause of this condition. A blood smear is performed. A normal blood smear looks like this: http://www.pathologystudent.com/?p=5230 John’s blood smear looks like this: What differences do you notice between the normal erythrocytes (red blood cells) and John’s? These enlarged erythrocytes are called megaloblasts. The additional blood work shows that John has normal levels of folate, but low cobalamin (vitamin B12). Familiarize yourself with this vitamin at http://ods.od.nih.gov/factsheets/VitaminB12.asp . You decided to give him a vitamin B12 supplement, but John returns with no change in his condition. You believe his body is not absorbing the vitamin. Read the following article on the absorption of vitamin B12: http://findarticles.com/p/articles/mi_m0860/is_n2_v52/ai_8540075/ Is John lacking the intrinsic factor necessary for absorption? You run an antibody test which shows no sign of intrinsic factor deficiency. You also are certain to note that John does not suffer from homocystinuria (symptoms include dislocation of eye lens, skeletal malformations) and methylmalonic acidemia (symptoms include feeding issues, kidney disease, pancreatitis), which should help to narrow your search for a diagnosis. Now it is time to collaborate with the geneticist and determine if anything can be concluded from the survey of John’s genome. PROCESS – Surveying and Sequencing DNA: The Geneticist *As good clinical practice, take careful notes and be able to explain/describe all steps of the amplification, surveying and sequencing process. Also, do not be afraid to consult your supervisor. When seven-year-old John arrives at The Clinic, the doctor immediately suspects a genetic disorder is at the root of his medical problems. His DNA is sampled and sent to you for analysis. In order to determine which (if any) gene is causing John’s condition, you need to survey his genome. In The Clinic’s lab, you have the ability to amplify John’s DNA using PCR and then run a 10K microarray. Go to the lab and amplify the DNA: http://www.dnalc.org/ddnalc/resources/pcr.html Look at the amplification graph – how many target copies are created after 30 cycles? Now you have amplified the DNA – go to the lab and run a 10K Microarray: http://learn.genetics.utah.edu/content/labs/microarray/ *Please note that the process in this simulation involves comparing DNA from two types of cells, so each is labeled with a different color. Since we are only comparing one DNA sample from John, there will be no labeling and the results will be analyzed a bit differently. This simulation does demonstrate the basics of the microarray process and provides an excellent example of its use. Wonder how they make the microarray chip? Check out this brief video: http://www.youtube.com/watch?v=ui4BOtwJEXs And this simulation: http://www.dnalc.org/ddnalc/resources/dnachip.html The 10K microarray has identified regions of John’s genome that are homozygous, meaning he has two copies of the same allele. Why does homozygosity matter to you? Hint: http://www.ncbi.nlm.nih.gov/pubmed/15558715 The microarray displays its results in an Excel file. Familiarize yourself with the parts of this spreadsheet so that you may explain it to the doctor and quickly examine it when hypothetical problem genes have been identified. Once you have identified a potential problem gene, it must be sequenced. Review the sequencing process so that this may be done quickly when the time comes: http://www.dnalc.org/ddnalc/resources/cycseq.html Now it is time to collaborate with the doctor and determine if anything can be concluded from the list of John’s signs and symptoms. PROCESS – Identifying and Analyzing Problem Genes: The Team Now that a comprehensive list of John’s symptoms and signs have been produced and his genome has been surveyed, it is time to start identifying possible disorders and the genes they are associated with. But first, the doctor must give a comprehensive overview of his/her part of the process so that the geneticist has the necessary knowledge to proceed. Now, go to NCBI’s Online Mendelian Inheritance of Man: http://www.ncbi.nlm.nih.gov/omim/ Together, enter combinations of John’s symptoms. Remember to use Boolean search terms like AND, OR, NOT in all capitals. Also, remember that using medical terms such as anemia might be more beneficial than generic symptoms like a headache. How many hits are you getting in the OMIM database? Are there too many/few to make any conclusions? Since you have surveyed John’s genome, limit the search to entries with a known molecular basis that you will be able to check for. To do this, go to the limits page and check the box next to the # sign. How many hits are you getting now? Using the various combinations of John’s symptoms, begin reviewing the information on each disorder. Make a list of the top four or five disorders that are good possibilities from a symptomatic standpoint. For each of the disorders on the list, click on the link next to the gene map locus. Using the chart below, record the name and genetic location of genes that may be causing John’s disorder. To determine the physical location, click on the genetic location and examine the chromosomes for the gene you are looking for. The physical location can be determined using the scale on the left side of the screen and will be in millions of base pairs. Candidate gene Genetic location Physical location GIF 11q13 CUBN 10p12.1 AMN 14q32 SLC56A1 17q11.1 Chr 11 55.95MB Chr 10 17.05MB Chr 14 102.45MB Chr 17 23.75MB Number homozygous markers 3 Size of homozygous region (bp) 3 4,981,811 873,898 27 9,251,483 7 5,720,239 Now it is time to examine the 10K microarray data to see if John displays regions of high homozygosity in any of the previously identified genes. But first, the geneticist must give a comprehensive overview of his/her lab work so that the doctor has the necessary knowledge to proceed. Together, find the SNP markers in the previously identified candidate genes using the genetic and physical locations you recorded in the chart. Record the number of homozygous SNPs that are in a row at each gene, as well as the number of base pairs each homozygous region extends for. Does your team hypothesize that any of the candidates is the problem gene? Which one? Why? Once the hypothetical problem gene is identified, it must be sequenced. If the geneticist has not previously reviewed the sequencing process with the doctor, he/she should do so at this point. After sequencing John’s DNA, you receive the following electropherogram and sequence: CCGCCCCTCGCACCAGGCGCAGCCGTGGATCTGCGCGGCCCTGCTCCAGCCCCGGCCCAGGGGCAGTGC TGTGACCTCTGTGGTAAGCGCCCCCGCCGGGCCCTGCTTGCTGGGAAGGCCTGGAGGACCAGGTTCGTC CCCCGCCTCAGTTTCCTGCCGGGCCCGGATCCACGGCGCTGACCCCTGCCCTCCCGCCGCAGGAGCCGTT GTGTTGCTGACCCACGGCCCCGCATTTGACCTGGAGCGGTACCGG How can John’s sequenced DNA be of use? How will you know if the hypothetical problem gene has a mutation? BLAST is a sequence comparison tool that will take your sequence of interest and compare it to more than ten million sequences that are stored in the public database (NCBI). It will also calculate the statistical significance of similarity for the matches it finds. Go to BLAST: http://blast.ncbi.nlm.nih.gov/Blast.cgi?PROGRAM=blastn&BLAST_PRO GRAMS=megaBlast&PAGE_TYPE=BlastSearch&SHOW_DEFAULTS=on& LINK_LOC=blasthome Enter John’s sequence and BLAST with a high stringency. What kind of results do you see? Remember that you sequenced a candidate gene so the best match will be the reference sequence, which will likely cover 100% of John’s sequence. Now try BLASTing John’s sequence with less stringency – choose “more dissimilar sequences.” How have your results changed? Finally, try BLASTing his sequence with the lowest stringency. What are the differences in your results? After carefully analyzing the BLAST results, is there a problem with John’s gene? If so, what is it? PROCESS – Treating the Patient’s Disorder – The Team You have now successfully found the genetic cause of John’s disorder. You have done nothing, however, to actually help John feel better! To do so, you must formulate a treatment strategy. A good place to start is to look at the OMIM entries for the identified disorder and gene. Doctor – You are interested in the disorder: http://www.ncbi.nlm.nih.gov/entrez/dispomim.cgi?id=261100 How does John compare with other recorded clinical cases? Geneticist – You are interested in the gene: http://www.ncbi.nlm.nih.gov/entrez/dispomim.cgi?id=605799 What role does the gene play? What biochemical effect does the mutation have on John? Utilizing the information you both gathered, brainstorm possible treatments that could help John. After your discussion, consult other professionals: http://www.nutritionmd.org/consumers/hematology/megoblastic_dia gnosis.html http://www.healthline.com/treatments/megaloblasticanemia__#prescriptions http://www.vitabase.com/supplements/energy/sublingualb12.aspx What is the best treatment plan for John? CONCLUSION Congratulations! You have successfully diagnosed and treated John! He and his family are very grateful to you and The Clinic for Special Children. *Special Note: All information, user guides and other data has been adapted from an activity used during the 2009 Bioinformatics Seminar at Franklin & Marshall College, in conjunction with The Clinic for Special Children. Biology department faculty from F&M College and doctors from The Clinic designed the original activity this WebQuest is based on.