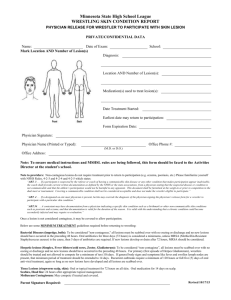
path 740 to 749 [5-6
advertisement

Path p 740-749 Teeth and Supporting Structures Anatomic crown of tooth = projecting part; covered by enamel (acellular; most highly mineralized tissue in body) o Enamel rests on dentin (specialized form of CT that makes up most of remaining hard-tissue portion Cellular; contains dentinal tubules that contain cytoplasmic extensions of odontoblasts (cells that line interface between dentin and pulp; can produce new secondary dentin in interior of tooth when stimulated) o Pulp chamber consists of LCT stroma rich in nerve bundles, lymphatics, and capillaries o Teeth attached to alveolar ridge of jaws by periodontal ligament, which attaches alveolar bone of jaw on one side and cementum (in roots of teeth; anchors periodontal ligament to tooth) Caries – focal degradation of tooth structure; lesions result from mineral dissolution of tooth structure by acid metabolic end products from bacteria in oral cavity fermenting sugars o Fluoride incorporates into crystalline structure of enamel, forming fluorapatite, contributing to resistance to degradation by bacterial acids Gingiva = squamous mucosa between teeth and around them; gingivitis = inflammation of mucosa and associated soft tissues caused by plaque build-up beneath gumline; usually result of lack of proper oral hygiene o Dental plaque – biofilm that builds on surface of teeth; formed by complex of oral bacteria, proteins from saliva, and desquamated epithelial cells o If plaque continues to build, it becomes mineralized to form calculus (tartar) o Bacteria in plaque release acids from sugar-rich foods, which erode enamel surface of tooth; repeated erosions lead to dental caries o Chronic gingivitis – gingival erythema, edema, bleeding, changes in contour, and loss of soft-tissue adaptation to teeth Periodontitis – inflammatory process that affects periodontal ligaments, alveolar bone, and cementum o Loosening and eventual loss of teeth possible o Associated w/marked shift in types and proportions of bacteria along gingiva (poor hygiene contributes) o Facultative Gram+ organisms colonize healthy sites; plaque in areas of active periodontitis contains anaerobic and microaerophilic Gram- flora Primarily Aggregatibacter (Actinobacillus) actinomycetemcomitans, Porphyromonas gingivalis, and Prevotella intermedia o Can be component of AIDS, leukemia, Crohn’s disease, DM, Down syndrome, sarcoidosis, and syndromes associated w/PMN defects (Chédiak-Higashi syndrome, agranulocytosis, cyclic neutropenia) o Etiologic factor in development of infective endocarditis, pulmonary and brain abscesses, and adverse pregnancy outcomes Inflammatory/Reactive Tumor-Like Lesions Irritation fibroma – primarily occurs in buccal mucosa along bite line or at gingivodental margin o Nodular mass of fibrous tissue w/few inflammatory cells covered by squamous mucosa o Treatment is complete surgical excision Pyogenic granuloma – highly vascular pedunculated lesion, usually occurring in gingiva of children, young adults, and pregnant women (pregnancy tumor) o Surface of lesion ulcerated and red to purple in color; can grow quickly o Highly vascular proliferation o Either regress or undergo fibrous maturation; may develop into peripheral ossifying fibroma o Treat w/complete surgical excision Peripheral ossifying fibroma – reactive, not neoplastic; red, ulcerated, nodular lesions of gingiva o Complete surgical excision down to periosteum Tx of choice; recurrence rate of 15-20% Peripheral giant cell granuloma – covered by intact gingival mucosa (may be ulcerated) o Bluish-purple in color o Aggregation of multinucleate foreign body-like giant cells separated by fibroangiomatous stroma o Not encapsulated, but well delimited and easily excised Aphthous ulcers (canker sores) – tend to be prevalent w/in certain families o Shallow hyperemic ulcerations covered by thin exudate and rimmed by narrow zone of erythema o Underlying inflammatory infiltrate at first mononuclear; secondary bacterial infection brings neutrophils o Recurrent lesions associated w/celiac disease and inflammatory bowel disease Glossitis – inflammation of tongue; beefy-red tongue encountered in certain deficiency states, resulting from atrophy of papillae of tongue and thinning of mucosa, exposing underlying vasculature o Atrophic changes can lead to inflammation and shallow ulcerations o Seen w/deficiencies of vitamin B12 (pernicious anemia), riboflavin, niacin, or pyridoxine; can be w/sprue, iron-deficiency anemia, or deficiency of other B vitamins o Iron-deficiency anemia + glossitis + esophageal dysphagia = Plummer-Vinson syndrome (Paterson-Kelly) o Glossitis characterized by ulcerative lesions can be seen w/jagged carious teeth, ill-fitting dentures, and rarely w/syphilis, inhalation burns, or ingestion of corrosive chemicals Infections Nature defenses of oral mucosa = competitive suppression of potential pathogens by low virulence flora, elaboration of secretory IgA and other Ig’s by submucosal collections of lymphocytes and plasma cells, antibacterial effects of saliva, and irrigating effects of food and drink Most orofacial herpetic infections caused by HSV-1; increase in HSV-2 (genital herpes) observed in oral cavity o Primary HSV infection occurs in children 2-4 years, often asymptomatic; 10-20% have acute herpetic gingivostomatitis (abrupt onset of vesicles and ulcerations throughout oral cavity, especially in gingiva Lesions accompanied by lymphadenopathy, fever, anorexia, and irritability o Vesicles at first filled w/clear serous fluid; often rupture to yield painful, red-rimmed, shallow ulcerations; intracellular and intercellular edema (acantholysis) Individual epidermal cells in margins of vesicle or lying free in fluid sometimes develop eosinophilic intranuclear viral inclusions; several cells may fuse to produce multinucleate polykaryons (giant cells) Tzanck test – based on microscopic exam of vesicle fluid; positive if giant cells o Vesicles and ulcers clear spontaneously, but virus goes along regional nerves and becomes dormant in local ganglia (trigeminal) o Virus can reactivate to cause cold sore; can be activated by trauma, allergies, exposure to UV, URI, pregnancy, menstruation, immunosuppression, and exposure to extremes of temp o Recurrent herpetic stomatitis occurs at site of primary inoculation or adjacent mucosal areas associated w/same ganglion; groups of small vesicles Lips (herpes labialis), nasal orifices, buccal mucosa, gingiva, and hard palate most common locations for recurrent lesions Candidiasis – Candida albicans is normal oral flora in 50% of population; factors for infection include immune status of patient, strain of candida, and composition of individual’s oral flora o Major clinical forms of oral candidiasis: thrush (pseudomembranous), erythematous, and hyperplastic o Pseudomembranous form = gray to white inflammatory membrane composed of matted organisms enmeshed in fibrinosuppurative exudate that can be scraped off to reveal underlying erythematous inflammatory base o Usually only occurs in immunosuppressed or when broad-spectrum antibiotics eliminate other flora Oral Manifestations of Systemic Disease Hairy leukoplakia – seen in immunocompromised; 80% of patients have HIV o White confluent patches of fluffy (hairy) hyperkeratotic thickenings, almost always situated on lateral border of tongue; lesion can’t be scraped off (distinguishing from thrush) o Hyperparakeratosis and acanthosis w/balloon cells in upper spinous layer o Sometimes koilocytosis of superficial nucleated epidermal cells, suggesting HPV infection; EBV present in most cells (this is cause, though HPV can be present) o Superimposed candida infection on surface of lesions adds to hairiness Tumors and Precancerous Lesions Early lesions don’t demonstrate any clinical characteristics observed in advanced oral cancer (ulceration, induration, pain, or cervical lymphadenopathy) Leukoplakia – white patch or plaque that can’t be scraped off and can’t be characterized clinically or pathologically as any other disease o 5-25% of leukoplakias premalignant; consider precancerous until proven otherwise o May occur anywhere in oral cavity; white patches or plaques, often w/sharply demarcated borders o o o o May be slightly thickened and smooth or wrinkled and fissured; can be raised, corrugated, verrucous Hyperkeratosis overlying thickened acanthotic but orderly mucosal epithelim Can have markedly dysplastic changes (carcinoma in situ) The more dysplastic or anaplastic the lesion, the more likely that subjacent inflammatory infiltrate of lymphocytes and macrophages will be present Erythroplakia – red, velvety, possibly eroded area in oral cavity that remains level with or may be slightly depressed in relation to surrounding mucosa o Epithelium atypical, incurring higher risk of malignant transformation than leukoplakia o Virtually all have superficial erosions w/dysplasia, carcinoma in situ, or already developed carcinoma in surrounding margins o Intense subepithelial inflammatory reaction w/vascular dilation contributes to reddish appearance Speckled leukoerythroplakia – characteristics of both leukoplakia and erythroplakia Use of tobacco products most common risk factor for leukoplakia and erythroplakia HNSCCs – head and neck squamous cell carcinomas; 95% of cancers of head and neck; most common in mouth o Aggressive epithelial malignancy; 5-year survival if caught early 80%; if late 19% o Often diagnosed when disease already reached advanced stage o Frequent development of multiple primary tumors (3-7% per year) decreases survival; most common cause of death is complications due to new primary tumors o Higher risk in those who smoke and drink or abuse either by themselves o 50% of oropharyngeal cancers (particularly tonsils, base of tongue, and oropharynx) have oncogenic HPV Those w/HPV+ HNSCC do better than those w/HPVo Actinic radiation (sunlight) and pipe smoking are predisposing influences for cancer of lower lip o Chewing betel quid and paan in Indaia and Asia predisposes Betel quid part of witches’ brew; contains areca nut, slaked lime, and tobacco in betel leaf o Chronic irritation of mucosa can act as promoter of cancer o LOH in conjunction w/promoter hypermethylation results in inactivation of p16 (inhibitor of cyclindependent kinase) transition from normal to hyperplasia/hyperkeratosis; occurs before development of histologic atypia LOH w/mutation in p53 associated w/progression to dysplasia Amplification and overexpression of cyclin D1 gene constitutively activates cell cycle progression EFGR overexpressed in high percentage of HNSCC; successfully targeted in Tx o Early stages appear raised firm pearly plaques or irregular roughened or verrucous areas of mucosal thickening (mistaken for leukoplakia) o Enlarge, creating ulcerated protruding masses w/irregular indurated (rolled) borders o Begin as dysplastic lesions; can progress to full-thickness dysplasia (carcinoma in situ) before invading underlying CT stroma (invasion before carcinoma in situ sometimes) o Degree of histologic differentiation not correlated w/behavior o Common metastases = cervical lymph nodes, mediastinal lymph nodes, lungs, liver, and bones Odontologic Cysts and Tumors Epithelial-lined cysts common in jaws; most derived from remnants of odontogenic epithelium in jaws o Classified as inflammatory or developmental Dentigerous cyst – originates around crown of unerupted tooth; result of degeneration of dental follicle o Unilocular lesions; most often associated w/impacted widom tooth o Lined by thin layer of stratified squamous epithelium o Dense chronic inflammatory cell infiltrate in CT stroma o Complete removal of lesion curative; incomplete excision results in recurrence or (rarely) neoplastic transformation into ameloblastoma or squamous cell carcinoma Odontogenic keratocyst (OKC) – locally aggressive; high rate of recurrence (60%); occur most commonly in males in posterior mandible; well-defined unilocular or multilocular radiolucencies o Cyst lining has thin layer of parakeratinized or orthokeratinized stratified squamous epithelium w/prominent basal cell layer and corrugated appearance of epithelial surface o Tx requires aggressive and complete removal of lesion o Multiple OKCs can occur; evaluate these for nevoid basal cell carcinoma syndrome (Gorlin) related to mutations in tumor suppressor gene PTCH Periapical cyst – inflammatory lesion found at apex of teeth; develop as result of long-standing pulpitis caused by advanced carious lesions or trauma to tooth o May result in necrosis of pulpal tissue, which can traverse length of root and exit apex into surrounding alveolar bone, giving rise to periapical abscess o Lesion w/granulation tissue may develop o Persist as result of continued presence of bacteria or other offensive agents in area o Successful Tx necessitates complete removal of offending material and appropriate restoration of tooth or extraction Odontogenic tumors – group of lesions w/diverse histologic appearances and clinical behavior (some true neoplasms; some hamartomas) o Derived from odontogenic epithelium, ectomesenchyme, or both o Ameloblastoma – shows no ectomesenchymal differentiation; commonly cystic, slow growing, and locally invasive; indolent course in most cases o Odontoma – most common type of odontogenic tumor; arises from epithelium but shows extensive depositions of enamel and dentin; hamartomas cured by local excision