Audrey_Ertel_Ohio_COT_abstract
advertisement
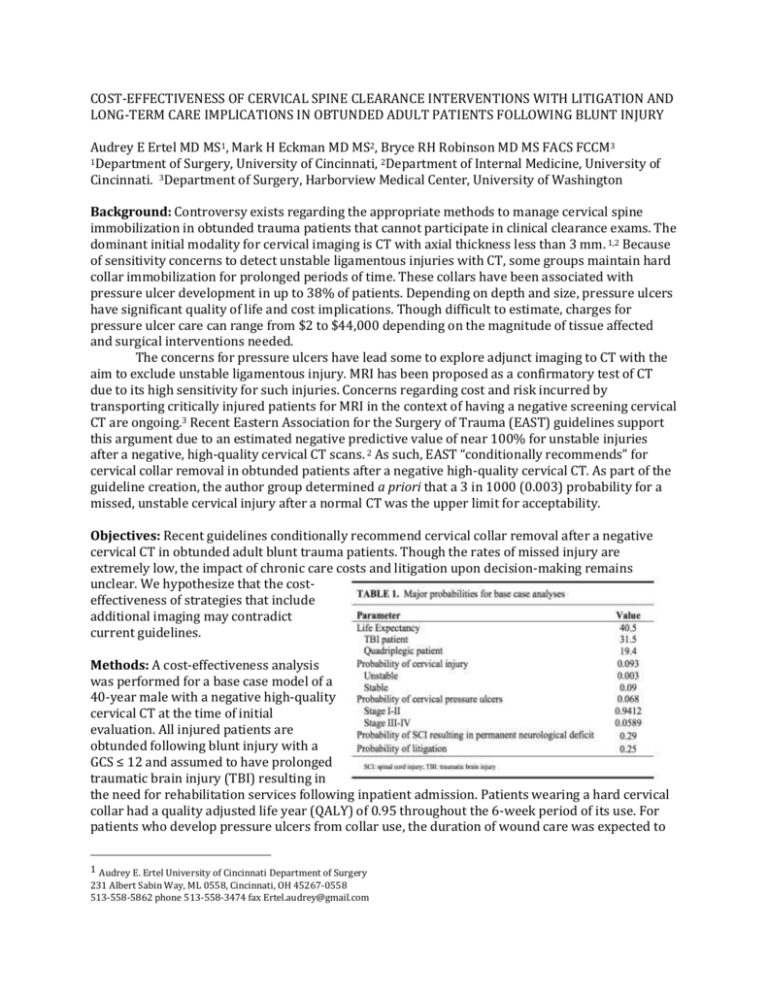
COST-EFFECTIVENESS OF CERVICAL SPINE CLEARANCE INTERVENTIONS WITH LITIGATION AND LONG-TERM CARE IMPLICATIONS IN OBTUNDED ADULT PATIENTS FOLLOWING BLUNT INJURY Audrey E Ertel MD MS1, Mark H Eckman MD MS2, Bryce RH Robinson MD MS FACS FCCM3 1Department of Surgery, University of Cincinnati, 2Department of Internal Medicine, University of Cincinnati. 3Department of Surgery, Harborview Medical Center, University of Washington Background: Controversy exists regarding the appropriate methods to manage cervical spine immobilization in obtunded trauma patients that cannot participate in clinical clearance exams. The dominant initial modality for cervical imaging is CT with axial thickness less than 3 mm. 1,2 Because of sensitivity concerns to detect unstable ligamentous injuries with CT, some groups maintain hard collar immobilization for prolonged periods of time. These collars have been associated with pressure ulcer development in up to 38% of patients. Depending on depth and size, pressure ulcers have significant quality of life and cost implications. Though difficult to estimate, charges for pressure ulcer care can range from $2 to $44,000 depending on the magnitude of tissue affected and surgical interventions needed. The concerns for pressure ulcers have lead some to explore adjunct imaging to CT with the aim to exclude unstable ligamentous injury. MRI has been proposed as a confirmatory test of CT due to its high sensitivity for such injuries. Concerns regarding cost and risk incurred by transporting critically injured patients for MRI in the context of having a negative screening cervical CT are ongoing.3 Recent Eastern Association for the Surgery of Trauma (EAST) guidelines support this argument due to an estimated negative predictive value of near 100% for unstable injuries after a negative, high-quality cervical CT scans. 2 As such, EAST “conditionally recommends” for cervical collar removal in obtunded patients after a negative high-quality cervical CT. As part of the guideline creation, the author group determined a priori that a 3 in 1000 (0.003) probability for a missed, unstable cervical injury after a normal CT was the upper limit for acceptability. Objectives: Recent guidelines conditionally recommend cervical collar removal after a negative cervical CT in obtunded adult blunt trauma patients. Though the rates of missed injury are extremely low, the impact of chronic care costs and litigation upon decision-making remains unclear. We hypothesize that the costeffectiveness of strategies that include additional imaging may contradict current guidelines. Methods: A cost-effectiveness analysis was performed for a base case model of a 40-year male with a negative high-quality cervical CT at the time of initial evaluation. All injured patients are obtunded following blunt injury with a GCS ≤ 12 and assumed to have prolonged traumatic brain injury (TBI) resulting in the need for rehabilitation services following inpatient admission. Patients wearing a hard cervical collar had a quality adjusted life year (QALY) of 0.95 throughout the 6-week period of its use. For patients who develop pressure ulcers from collar use, the duration of wound care was expected to 1 Audrey E. Ertel University of Cincinnati Department of Surgery 231 Albert Sabin Way, ML 0558, Cincinnati, OH 45267-0558 513-558-5862 phone 513-558-3474 fax Ertel.audrey@gmail.com be 3 months for stage I-II ulcers after a single operative debridement and 6 months for stage III-IV ulcers with patients undergoing a total of 3 operative debridements. The major probabilities for the base case analysis are demonstrated in Table 1. Strategies compared included: adjunct imaging with cervical MRI, collar maintenance for 6 weeks, or removal. The probability for collar pressure ulcer formation, spine injury, imaging costs, acute and chronic care, and litigation were obtained from published and Medicare data. Outcomes were expressed as 2014 US dollars and qualityadjusted life-years (QALYs). Finally, we estimated the probability of medical malpractice claims to be filed in the setting of an iatrogenic permanent spinal cord injury from collar removal at .25 for each occurrence. Those claims that progress to litigation were assumed to result in complete payout of the total claim amount. mCER ($/QALY) mCER ($/QALY) Results: The base case analysis evaluated the cost-effectiveness of three separate strategies for cervical spine management of a 40 year-old, obtunded, trauma patient following emergency department evaluation with a negative high-quality cervical CT scan. Quality-adjusted life expectancy (effectiveness) was similar for all three cervical spine strategies with adjunct MRI imaging having the highest value of 20.003, followed by removal of cervical collar of 19.995, and lastly, application of hard cervical collar of 19.989 quality-adjusted life years. Additionally, the difference in cost between adjuvant Figure 1 MRI imaging ($361,167.98) was $800,000 $178.44 less than application of cervical collar ($361,345.42) and was $700,000 $660.99 less than removal of cervical $600,000 collar ($361,828.97). Due to the fact $500,000 that adjunct imaging with MRI had $400,000 higher efficacy as well as lower cost, this strategy dominated all other $300,000 alternative strategies when evaluating $200,000 the base case scenario. These results $100,000 suggest that the appropriate $0 management for an obtunded patient 0 0.0001 0.0002 0.0003 0.0004 0.0005 0.0006 0.0007 following blunt injury with a negative Probability of Missed Unstable C-spine Injury high-quality cervical CT would be to perform adjunct cervical imaging with MRI. Figure 2 A main focus of our analysis was on the influence of the upper $175,000 acceptable limit for missed unstable $150,000 cervical spine injuries upon the cost$125,000 effectiveness of MRI. Previous 6 guidelines set this value at 0.003. $100,000 Sensitivity analyses were performed $75,000 upon this metric (Fig 1). With a $50,000 probability of missed cervical injury under 0.00001 the most effective and $25,000 least expensive strategy was removal $0 of the collar. Taking the cost$0 $500 $1,000 $1,500 $2,000 $2,500 effectiveness threshold of < $50,000 Cost of MRI per QALY, at a probability of missed injury of 0.0006, a miss probability 6- mCER ($/QALY) fold less than what was previously Figure 3 accepted, adjunct imaging with MRI was $25,000 found to be below this threshold (0.0005 = $59,213; 0.0006 = $30,215) as $20,000 compared with removal of the collar. Cost associated with MRI was also $15,000 explored as a function of cost$10,000 effectiveness. Adjunctive imaging with MRI proves to be the most cost-effective $5,000 strategy until cost of MRI exceeds $450 (Fig 2). The strengths of adjunct MRI $0 imaging in our model is based largely on $0 $40,000 $80,000 $120,000 $160,000 $200,000 the relatively low cost of the test, $223.46 Lifetime Cost of Quadraplegic Patient per CMS reimbursements. Furthermore, only when the cost of MRI exceeds $1,050, does the cost per QALY for adjunctive MRI exceed $50K. The lifetime costs associated with caring for a patient with a TBI were estimated to be $299,785.50 compared with $936,438 for those patients who suffer a spinal cord injury resulting in quadriplegia. The lifetime cost of a quadriplegic patient, even when reduced to $0, would not cause the addition of MRI screening to exceed the cost-effectiveness threshold when compared to removal of the collar (Fig 3). Conclusion: The benefits of early cervical collar removal are easy to recognize. However, the negatives appear under appreciated by current analyses of the literature that fail to investigate its impact upon quality-adjusted life years and cost-effectiveness. The cost to society of these potentially preventable injuries needs to be incorporated into care recommendations. Within our model, quadriplegics have a reduced length (19.4 vs. 31.4 years) and quality of life (0.572 vs. 0.635 quality of life adjustment) though a dramatically higher cost for lifetime care ($940,000 vs. $300,000) when compared to obtunded patients with TBI. Sadly, the economics of practicing medicine in a litigious environment are part of daily practice. Health systems as well as practitioners would assume significant litigation risk by causing what some may argue is a life changing iatrogenic injury. Our model assumes that 25% of those that incur an injury proceed with ligation with a claim rate of 100% for $917,400. With both of these real world cost included in the analyses, the economics favor MRI. In fact, margin of cost-effectiveness ratio (mCER) values of < $50,000 favor the use of MRI until this test reaches a cost of approximately $1100, 460% greater than the current CMS reimbursement rate. Our preliminary work support the use of adjunct cervical MRI after completion of a negative high-quality screening CT in obtunded patients following blunt injury. Thorough evaluation of risk and benefit of current cervical care strategies necessitate the inclusion of analyses utilizing quality adjusted life years and cost-effectiveness. Future work needs to fill literature voids so that more complex and accurate decision models can be created in the hope to define the ideal cervical strategy for each patient but also for society as a whole. REFERENCES 1. Como JJ, Diaz JJ, Dunham CM, et al. Practice management guidelines for identification of cervical spine injuries following trauma: Update from the eastern association for the surgery of trauma practice management guidelines committee. J Trauma. 2009;67(3):651659. 2. Patel MB, Humble SS, Cullinane DC, et al. Cervical spine collar clearance in the obtunded adult blunt trauma patient: A systematic review and practice management guideline from the eastern association for the surgery of trauma. J Trauma Acute Care Surg. 2015;78(2):430-441. 3. Davis JW, Phreaner DL, Hoyt DB, Mackersie RC. The etiology of missed cervical spine injuries. J Trauma. 1993;34(3):342-346.