CARE OF SPECIMENS Purposes of Specimen Collection 1
advertisement
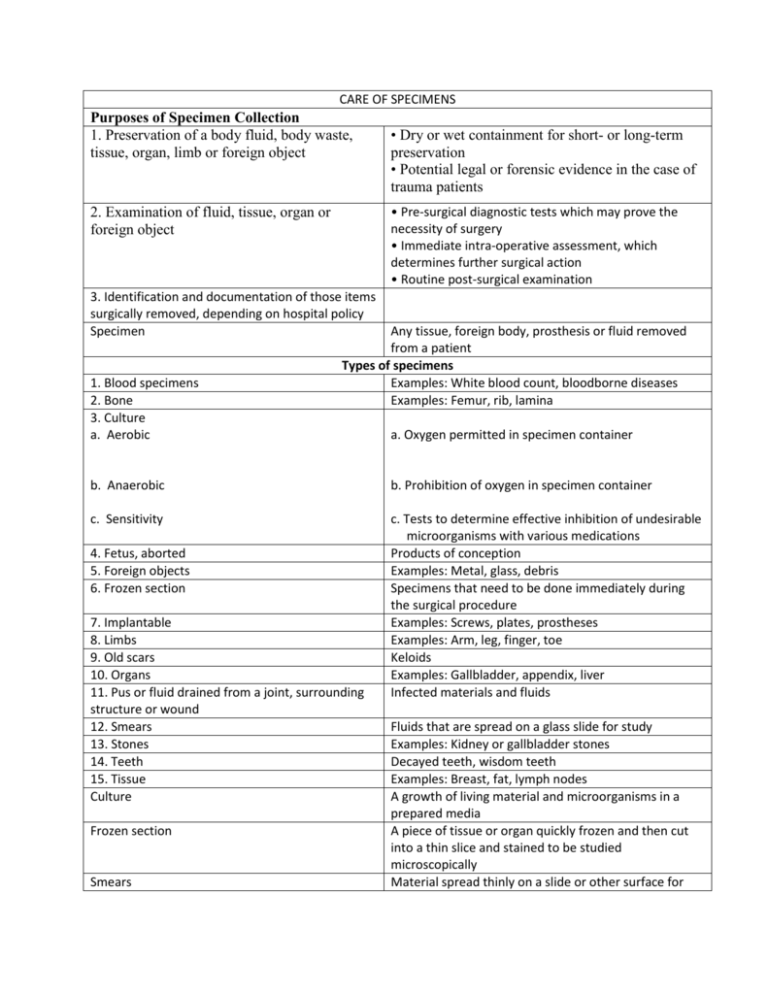
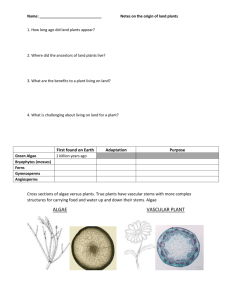
CARE OF SPECIMENS Purposes of Specimen Collection 1. Preservation of a body fluid, body waste, tissue, organ, limb or foreign object • Dry or wet containment for short- or long-term preservation • Potential legal or forensic evidence in the case of trauma patients • Pre-surgical diagnostic tests which may prove the necessity of surgery • Immediate intra-operative assessment, which determines further surgical action • Routine post-surgical examination 2. Examination of fluid, tissue, organ or foreign object 3. Identification and documentation of those items surgically removed, depending on hospital policy Specimen 1. Blood specimens 2. Bone 3. Culture a. Aerobic Any tissue, foreign body, prosthesis or fluid removed from a patient Types of specimens Examples: White blood count, bloodborne diseases Examples: Femur, rib, lamina a. Oxygen permitted in specimen container b. Anaerobic b. Prohibition of oxygen in specimen container c. Sensitivity c. Tests to determine effective inhibition of undesirable microorganisms with various medications Products of conception Examples: Metal, glass, debris Specimens that need to be done immediately during the surgical procedure Examples: Screws, plates, prostheses Examples: Arm, leg, finger, toe Keloids Examples: Gallbladder, appendix, liver Infected materials and fluids 4. Fetus, aborted 5. Foreign objects 6. Frozen section 7. Implantable 8. Limbs 9. Old scars 10. Organs 11. Pus or fluid drained from a joint, surrounding structure or wound 12. Smears 13. Stones 14. Teeth 15. Tissue Culture Frozen section Smears Fluids that are spread on a glass slide for study Examples: Kidney or gallbladder stones Decayed teeth, wisdom teeth Examples: Breast, fat, lymph nodes A growth of living material and microorganisms in a prepared media A piece of tissue or organ quickly frozen and then cut into a thin slice and stained to be studied microscopically Material spread thinly on a slide or other surface for microscopic study Guidelines for Care and Handling 1. All tissues, exudates and foreign objects removed from a patient must be sent to the pathology department for legal documentation. 2. Proper care of each specimen is the responsibility of the total nursing team, and especially the surgical technologist while the specimen is in his/her possession. 3. The care of specimens is regulated by hospital policy and rulings from the Joint Commission on Accreditation of Healthcare Organizations (JCAHO). 4. Preservation and identification of surgical specimens are crucial. The container housing the specimen will be labeled with appropriate patient information. A pathology requisition form will also accompany the specimen to the lab. 5. Handling of specimens should be kept to a minimum. 6. Pathologic tissue specimens should not be allowed to dry out. Saline or a solution of aqueous formaldehyde (10% formalin) is used until processed in the lab. 7. Never place formalin on stones or teeth. Pathology The study of diseases Formalin An aqueous solution of 37% formaldehyde with methanol added; commonly used as a preservative on specimens Standard Precautions 1. Handle all specimens using standard precautions. 2. Place all specimens of blood, body fluids, and tissues in a container to prevent leaking during transport to the lab. 3. Ensure the outside of the container is clean. 4. Wear non-sterile gloves to disinfect the outside of the culture tube or specimen container as it is handed from the sterile field. 5. Avoid contamination of the outside of the container with blood or body fluids. 6. Always wash hands after removing gloves that have been worn to handle specimens. Proper Care and Handling 1. Cultures — Send to the laboratory immediately before cultures dry. • General guidelines — Obtain under sterile conditions. The tips of the swabs must not be contaminated by any other source. — Always label the culture tube and complete the laboratory form including the source of the specimen • Anaerobic — Always check the color of the solution in the bottom of the tube when taking an anaerobic culture. Discard if it is pink, because this means oxygen is present in the tube. Exposure to room air can kill anaerobes in just a few minutes. — Replace the swab in the tube as quickly as possible after taking an anaerobic culture to prevent air from entering the culture tube. • Aerobic — Take smears and fluids to the lab as soon as possible to be processed correctly. 2. Frozen sections • Fill out pathology requisition form as completely as possible. — Include the operating room intercom number/phone number on the specimen card so the pathologist can report the results to the surgeon. — Alert the pathologist if the patient is under a local anesthetic so the report can be shown to the surgeon rather than using the intercom, which could be 3. Foreign objects Fixative 4. Stones or teeth 5. Amputated limbs 1. Receive the specimen heard by the patient. • Place the specimen in a labeled container without formalin. It will be handcarried to the pathology department by a member of the OR staff • Always give the specimen to a designated staff member in the pathology department. Never just set it on the shelf or cart. Dispose of or preserve foreign bodies according to hospital policy and keep a record for legal reasons. Forensic materials—Foreign bodies may have legal significance and may be claimed as evidence by the police. — Do not leave these specimens unattended at any time. — Hospital policy will dictate who should be given forensic evidence, i.e., medical examiner or pathologist. — Handle hard objects by hand, not with an instrument, since this might alter the object. — Place in specimen container. - Use only paper or glass to package evidence. Plastic encourages any item containing moisture to grow bacteria, degrading DNA evidence. - Fixative is not needed for metal or glass objects, including bullets, knives and bottle shards. — Record on operative record the recipient of the object and the time. — Document the specimen transfer tor the protection of hospital personnel. Always follow hospital policy, which is written according to individual laws. A substance used to harden and preserve specimens • Place in dry container and label. • Always send to the lab for gross examination prior to returning to the surgeon or patient. • Verify the patient has signed a consent form for disposal of the limb. • Remove all drapes and instruments from the limb. • Avoid placing an amputated limb in view of the patient, particularly if the patient has received a spinal or epidural anesthetic. • Attach patient label and pathology requisition form to the limb and take to tab. • Never leave an amputated limb lying on a specimen cart. • Wrap amputated extremities in a plastic bag before storing in the lab refrigerator. • The patient may request that the amputated extremity be sent to a mortuary for preservation for burial with his or her body after death. This request must be noted on the pathology requisition form. Always follow the hospital policy in regard to amputated limbs. Receiving a Pathologic Specimen • Make a sterile basin or medicine glass available to receive the specimen. • Never put a specimen on a sponge, because this may confuse sponge count. • If the specimen is attached to a clamp, place the specimen in a container, then remove clamp. Place the container with the specimen on the sterile back table. Always ask the surgeon how the specimen is to be labeled. • Make certain that clamping does not crush small specimens, because this makes tissue identification very difficult. • Specimens from endoscopic procedures may be retrieved in endo-bags or specimen retrieval bags. Remove the specimen from these plastic pouches before sending the specimen to the laboratory. 2. Select method for • Moist retaining optimal specimen Place a small amount of sterile saline on the specimen to keep it from drying integrity out. Keep specimens moist, but do not soak in the saline solution. • Dry Do not place saline on specimens to be sent for fresh tissue or frozen sections. 3. Intra-operative handling • Minimize handling of tissue specimens. • Some surgeons will want to mark the borders or margins (edges) of specimens with sutures known as "tags" for ease in identification by the pathologist. • If multiple specimens are expected, have several specimen containers available to receive the specimens and to avoid possible mislabeling. • Keep the specimen basin on the field until you are certain all tissue has been removed or all contaminated items are in it. 4. Note anomalies, location, • Keep each specimen separate. orientation or surgeon's • If you are unsure, ask the surgeon to identify the specimen. "tags" and reflect this • Place each specimen in a separate container and properly label the type of information when labeling tissue and area or location of its removal. 5. Handing a specimen from • Hand off the specimen to the circulator one at a time for correct the sterile field identification. Be sure to clearly communicate the origin of the specimen. • Hand a specimen from the field in a basin, on a wrapper, or on a towel. Specimen Preparation and Labeling 1. Selection of a container— • Container types Specimens should be placed Containers for storing specimens may be made of plastic, glass, or waxed in a specimen container to cardboard. ensure safety. —- Sterile — Nonsterile — Procedure-specific — Cytological specimen collectors such as Lukens are used to hold secretions as they are obtained. — Small specimens such as stones • Select a specimen container that is large enough for the specimen to be easily removed in the laboratory, since tissues enlarge or swell in formalin. • If the outside of the specimen container is contaminated with blood or body fluids, wipe the container with a tuberculocidal disinfectant. • Decontaminate the outside of specimen containers touched by sterile team members before sending to the lab. • Remove all instruments, sponges and/or needles from the specimen before sending it out of the room. 2. Proper preservation of the Use formalin in most instances, with the specimen following exceptions: never place on stones, teeth, limbs, or tissue scheduled for cultures or frozen sections • Formalin • Saline • Dry 3. Labeling of a container • Label each specimen separately. • Label each container with the patient's name, identification number and type of Specimen. • Ensure label is accurate. Incorrectly labeled specimens can result in an error in diagnosis, which may have critical implications for the patient or patients. • Attach the appropriate patient name label and pathology requisition form to the specimen container. 4. Transport and processing • Place the closed, labeled container in a plastic bag Of an additional of specimen container for transport to the lab. • Ensure the specimen is accompanied by a pathology requisition form that specifies the type of lab test requested by the surgeon. • Transfer directly to the lab or refrigerate non-critical specimens. • Handle and transport with care. The loss of a tissue or biopsy specimen could result in additional surgical procedures to obtain another specimen 5. Decontamination Wash hands after handling the specimen to avoid contamination Pathology Requisition Form 1. Date 6. Specimen description 2. Patient name lid medical record number 7. Preoperative and postoperative diagnosis 3. Patient's date of birth, age, and sex 8. Log number 4. Surgeon 9. Requested lab study 5. Attending/admitting physician