6.10 KHA_Proposal detail Standards Committee
advertisement

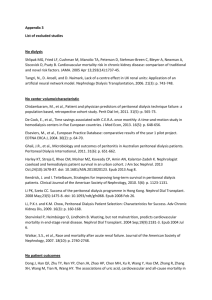
Additional Information Kidney Health Australia, The Home Dialysis Advisory Committee and the NSW Renal Services Network of the NSW Agency for Clinical Innovation (ACI) committee are all independently, but consultatively acting to ensure that home dialysis, both home haemodialysis (HHD) and home peritoneal dialysis (APD) are accessible and effective treatment options within Australia and NZ. Kidney Health Australia (KHA) is the peak body for those in Australia with kidney disease. Their mission related to home dialysis, is to remove any barriers that prevent all of those with kidney failure having the opportunity for home dialysis. Kidney Health New Zealand has the same function within New Zealand. The Home Dialysis advisory committee (HDAC) is an official national (Australia and NZ) committee comprising renal specialist doctors, renal nurses, allied health, and importantly consumer representation. This committee reports to the Dialysis, Nephrology and Transplant committee. It also actively pursues the removal of barriers to home dialysis, and has a strong education focus. The NSW Agency for Clinical Innovation (ACI) committee has a high priority to develop flexible, evidence-based patient-focused models of care. This includes determining any barriers to this care. Goals and Objectives The goal is to ensure that standard regulation is appropriate compared to the level of risk and the functionality of the machines related to home dialysis therapies. Net benefit of standard revision to the community About Home Dialysis Kidney failure requires treatment with either transplant or dialysis to prevent death. Home dialysis was introduced in the 1960s with the aim of reducing the inconvenience of travelling to a hospital or dialysis centre and increasing autonomy of patients. Home dialysis, either home haemodialysis (HHD) or automated peritoneal dialysis (APD) are the only feasible option for people living in rural or remote locations unless they wish to relocate closer to a satellite centre or renal unit. It is imperative that home dialysis remains a viable option for dialysis. The current standard has requirements that are a disincentive for home dialysis. Peritoneal dialysis is a daily treatment. It involves intermittent filling and emptying of the peritoneal cavity with fluid that can remove the wastes and fluids that build up during kidney failure. Automated peritoneal dialysis uses overnight treatment, controlled by the dialysis machine. Haemodialysis is the direct cleansing of the blood by a dialyser on a haemodialysis machine. It is completed at minimum, three times a week for 4 hour treatments. This treatment can be done at a specialised centre or within the home. Haemodialysis in the home can now use standard machines or portable new technology. 30% of patients are trained and supported to manage their own dialysis at home. The average time at home is 2-4years. Automated Peritoneal Dialysis Home Haemodialysis (standard) Nxstage – new technology Social and Community impact Home Dialysis is the preferred choice of health professionals because the advantages include: • ability for those on automated peritoneal dialysis and portable home haemodialysis to travel. • • • • • longer survival times decreased risk of exposure to hospital infections improved quality of life enhanced opportunities for rehabilitation and return to employment greater independence and flexibility to perform dialysis at a time that suits the individual with CKD and their families/carers • no time and cost issues associated with transport to dialysis Public Health and Safety Evidence suggests that the current standard may not be adhered to because of both financial factors and staff time factors that would be required for the current standard of automated peritoneal dialysis installation. If the standard is refined to an appropriate level there is commitment from health departments to adhere to the standard. Environmental impact Standard haemodialysis regimes at a satellite centre involve travel to 3 appointments every week. The average travel costs were estimated as $24 per week in 2009. National results – metropolitan National results – regional National results – mean 100% Proportion of respondents (%) 90% 80% 70% 60% 50% 40.0% 38.8% 37.4% 38.4% 40% 27.4% 30% 26.5% 23.7% 15.8% 20% 20.3% 13.4% 11.4% 6.8% 10% 0% 0–10 11–20 21–30 > 30 Round trip distance travelled to dialysis (km) Economic Impact Cost of Dialysis International costing data for dialysis programs in high income countries generally arrive at the same conclusion, that in-centre or hospital haemodialysis is the most expensive form of dialysis1. The costs associated with dialysis treatment per person per year are: • • • • $79,072 $65,315 $53,112 $49,137 Hospital Satellite Home – Peritoneal dialysis (PD) Home – Haemodialysis (HHD)2 The savings to the commonwealth are from $12 000- $30 000 per annum per patient managing their treatment at home rather than in a hospital or satellite Additional to health department costs, those funded by the patients are one identified barrier to home dialysis, and this includes machine installation, ongoing water and electricity costs and other miscellaneous costs. AS/NZS 3003 installation requirements are estimated to be between $800-$1200 per patient for HHD, and would be similar per patient for PD. This may be paid by the patient or by the health department depending on the jurisdiction of the patient. Therefore it is important to ensure the cost is justified. 1 Kidney Health Australia, 2006, The Economic Impact of End-Stage Kidney Disease in Australia, p. 78. 2 Kidney Health Australia, 2010, The Economic Impact of End-Stage Kidney Disease in Australia, Projections to 2020, p. 27. Need for the proposed work Please identify and provide evidence of the problem to be addressed, the goals and objectives of the proposed Standard(s), and demonstrate that it is justified and implementation is likely. Machines affected by standard, section 5.2.1/2 There are two machine options for home dialysis: automated peritoneal dialysis and home haemodialysis. The machine suppliers for automated peritoneal dialysis include Fresenius Medical Care, and Baxter Healthcare. Both are classified home care medical electrical equipment having Type B parts and are therefore subject to AS/NZS:3003, section 5.2.1or2. The current machine suppliers for home haemodialysis include Fresenius Medical Care and Gambro Pty Ltd. Nxstage is a new generation portable haemodialysis machine which indicates a requirement for compliance with section 5.2.1 although the parts are classified Type BF. Both Fresenius Medical Care and Baxter Healthcare are currently developing new portable home haemodialysis technologies, which are anticipated to be on trial in Australia within 2 years. AS/ANZ:3003 Evaluation related to Home Dialysis Within the renal profession, KHA, the HDAC, the NSW renal ACI there is growing concern that the mandatory requirements within this standard may be unnecessarily prohibitive to patients choosing to go home. Therefore advice to confirm or refute this has been sought from experts in the industry, both electrical experts, dialysis technicians and dialysis nurses, lawyers and the Ministry of Health in NSW. It is of note that for HHD many of these standards have been partially implemented since 2003, but the same had not applied for APD, indeed no one was initially aware it even implicated APD. In depth analysis of the standard has occurred, particularly to seek the interpretation of the rationale for the separate electrical circuit requirement 5.2.1(c) and 5.2.2.2(b). Electricians have advised that these points intend to prevent power failure to the machine, caused by a power issue elsewhere in the home. Expert home dialysis nurses, and Fresenius and Baxter clinical experts, have agreed that this is not a safety essential for a number of reasons: • • • • Both HHD and PD machines have battery back-up, which allows the patient adequate time to disconnect themselves from the machine all HHD and PD patients are taught how to disconnect if there was complete power failure the majority of patient dialyse accompanied at home HHD and PD machines do not maintain life in the way that a ventilator or oxygen therapy might and treatment can be safely delayed to the following day. Additionally advice indicates that for those living in a unit, or an old property the installation of a separate circuit may be cost-prohibitive or practically impossible to achieve. This will lead health services to limit these treatment options to those whose properties can easily be adapted. Importantly as a patient on APD, these therapies already has a high treatment burden and the flexibility of using the machine in multiple places has always been one area of freedom. In pursuing information about the development and the consultation process related to this standard it appears the consulted renal industry expert was not aware of all implications of the standard, and also did not consult widely for opinion about the standard. It has also become clear that other key players in the development were not aware that the standard now implicated APD machines. Additionally the new generation of HHD machines entering the market, currently Nxstage are planned to be portable and were not known about during guideline development. Current Industry practice In 2003 AS/ANZ 3003 standard incorporated home haemodialysis machines, but was not classified as mandatory. A number of dialysis units adopted this standard, but a number independently assessed the risks and determined that they would only implement certain aspects of the standard. AS/NZS 3003 became mandatory in 2011, and at this point the introduction of the standard for all haemodialysis and automated peritoneal dialysis was identified. Industry confusion however and indeed standard board confusion led to a delay in confirming that APD machines were now indeed subject to the standard. During meetings it also became apparent that there are barriers to the full implementation. It has been established that all home dialysis for both haemodialysis and peritoneal dialysis machines are protected by an RCD or LPD device, and health departments will continue this practice. The measures that prevent patient electrocution are not in dispute and all experts consulted agreed that many points are considered safe practice. Expert electricians and technicians have however raised other concerns that may also require future clarification. Current Standard proposal for change: Priority 1: It is proposed that the current standard, section 5.2.2 be modified to allow simple installation of automated peritoneal dialysis with a leakage protection device rather than a dedicated circuit. Priority 2: It is proposed that portable technology home haemodialysis machines are subject to the regulations of other home care installations 5.2.2 rather than home haemodialysis 5.1.1. Priority 3: It is proposed that ultimately home haemodialysis installations 5.2.1 be assessed and updated to match modern dialysis technology and home-care practice to develop practical and achievable installation standards that are financially appropriate and fit with dialysis industry practice. Appendix 1. Copy of content of letter to machine providers. Baxter Healthcare and Fresenius medical care both provided agreement to the pursuance of this matter. Re: Electrical Installations – patient areas – AS/NZS 3003:2011 Kidney Health Australia, on behalf of the Home Dialysis Advisory Committee (HDAC) is preparing a submission to the standards board related to the April 2011 standard: electrical installations – patient areas. The intent is to request modification to the guideline in relation to the dedicated circuit for APD. Interpretation of this standard, section 5.2.1 regarding home haemodialysis determines the requirements for dedicated circuits, the use of residual current devices, and the specific use and marking of all sockets within three metres of the dialysis machine. As home haemodialysis was regulated in AS/NZS 3003:2003 these recommendations appear to be standard practice in most jurisdictions. The HDAC are accepting of this part of the standard is preparing documentation to ensure all units are aware that this regulation is now mandatory rather than optional. Guideline section 5.2.2 considers machines other than haemodialysis. This new section specifies the machines, which by classification are subject to the regulations. The affected machines require dedicated circuits and electricity modifications as above. Rationale for the regulation is a key issue. It is acknowledged that the use of residual current devices has an important role in the prevention of accidental electrocution, in the event of machine failure. The rationale for the dedicated circuit has been interpreted by industry specialists as being to prevent accidental power-loss to the machine, caused by electricity issues elsewhere on the property. Whilst this is known to be a more difficult issue for HHD, because of the more complex disconnection process, specialists and the HDAC agreed that it is an insignificant issue with an easy solution for PD. How the regulations pertain to the peritoneal dialysis machines is therefore issue the HDAC would like the standards board to review. Whilst it is understood that consultation regarding the new guideline occurred related to haemodialysis, it is thought that the consideration of the inclusion of peritoneal dialysis was not assessed. The HDAC and KHA also recognise that if a PD installation becomes prohibitive then this will impact on the uptake of home peritoneal dialysis. Prior to a submission however KHA and the HDAC need to confirm the classification of the peritoneal dialysis cyclers, used on the Australian market. It is understood that the Baxter Home-choice cycler is rated as Class 1 (uses an earthed mains connection) and the patient circuit is Type B (non-floating). If so this renders the machine subject to the classification. Please can Baxter Health-care confirm the classification of the sleep-safe cycler. KHA and the HDAC would appreciate any further comments relating to this standard and your support, or not, regarding their intent to request alterations to the standard. Please contact me for further clarification. Warm regards