jcpe1783-sup-0003-appendixS3
advertisement
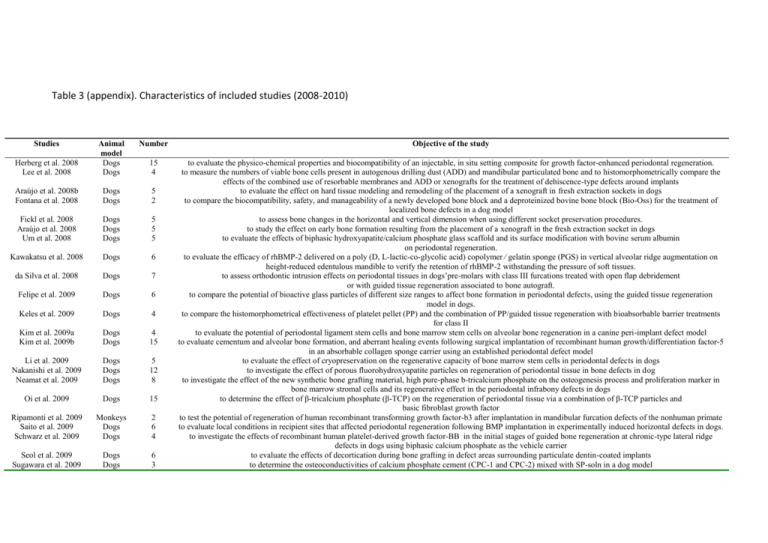
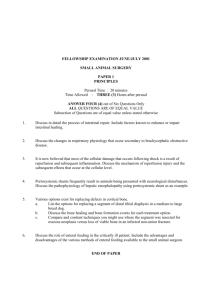
Table 3 (appendix). Characteristics of included studies (2008-2010) Studies Number Objective of the study Herberg et al. 2008 Lee et al. 2008 Animal model Dogs Dogs 15 4 Araújo et al. 2008b Fontana et al. 2008 Dogs Dogs 5 2 Fickl et al. 2008 Araújo et al. 2008 Um et al. 2008 Dogs Dogs Dogs 5 5 5 Kawakatsu et al. 2008 Dogs 6 da Silva et al. 2008 Dogs 7 Felipe et al. 2009 Dogs 6 Keles et al. 2009 Dogs 4 Kim et al. 2009a Kim et al. 2009b Dogs Dogs 4 15 Li et al. 2009 Nakanishi et al. 2009 Neamat et al. 2009 Dogs Dogs Dogs 5 12 8 Oi et al. 2009 Dogs 15 Ripamonti et al. 2009 Saito et al. 2009 Schwarz et al. 2009 Monkeys Dogs Dogs 2 6 4 Seol et al. 2009 Sugawara et al. 2009 Dogs Dogs 6 3 to evaluate the physico-chemical properties and biocompatibility of an injectable, in situ setting composite for growth factor-enhanced periodontal regeneration. to measure the numbers of viable bone cells present in autogenous drilling dust (ADD) and mandibular particulated bone and to histomorphometrically compare the effects of the combined use of resorbable membranes and ADD or xenografts for the treatment of dehiscence-type defects around implants to evaluate the effect on hard tissue modeling and remodeling of the placement of a xenograft in fresh extraction sockets in dogs to compare the biocompatibility, safety, and manageability of a newly developed bone block and a deproteinized bovine bone block (Bio-Oss) for the treatment of localized bone defects in a dog model to assess bone changes in the horizontal and vertical dimension when using different socket preservation procedures. to study the effect on early bone formation resulting from the placement of a xenograft in the fresh extraction socket in dogs to evaluate the effects of biphasic hydroxyapatite/calcium phosphate glass scaffold and its surface modification with bovine serum albumin on periodontal regeneration. to evaluate the efficacy of rhBMP-2 delivered on a poly (D, L-lactic-co-glycolic acid) copolymer ⁄ gelatin sponge (PGS) in vertical alveolar ridge augmentation on height-reduced edentulous mandible to verify the retention of rhBMP-2 withstanding the pressure of soft tissues. to assess orthodontic intrusion effects on periodontal tissues in dogs’pre-molars with class III furcations treated with open flap debridement or with guided tissue regeneration associated to bone autograft. to compare the potential of bioactive glass particles of different size ranges to affect bone formation in periodontal defects, using the guided tissue regeneration model in dogs. to compare the histomorphometrical effectiveness of platelet pellet (PP) and the combination of PP/guided tissue regeneration with bioabsorbable barrier treatments for class II to evaluate the potential of periodontal ligament stem cells and bone marrow stem cells on alveolar bone regeneration in a canine peri-implant defect model to evaluate cementum and alveolar bone formation, and aberrant healing events following surgical implantation of recombinant human growth/differentiation factor-5 in an absorbable collagen sponge carrier using an established periodontal defect model to evaluate the effect of cryopreservation on the regenerative capacity of bone marrow stem cells in periodontal defects in dogs to investigate the effect of porous fluorohydroxyapatite particles on regeneration of periodontal tissue in bone defects in dog to investigate the effect of the new synthetic bone grafting material, high pure-phase b-tricalcium phosphate on the osteogenesis process and proliferation marker in bone marrow stromal cells and its regenerative effect in the periodontal infrabony defects in dogs to determine the effect of β-tricalcium phosphate (β-TCP) on the regeneration of periodontal tissue via a combination of β-TCP particles and basic fibroblast growth factor to test the potential of regeneration of human recombinant transforming growth factor-b3 after implantation in mandibular furcation defects of the nonhuman primate to evaluate local conditions in recipient sites that affected periodontal regeneration following BMP implantation in experimentally induced horizontal defects in dogs. to investigate the effects of recombinant human platelet-derived growth factor-BB in the initial stages of guided bone regeneration at chronic-type lateral ridge defects in dogs using biphasic calcium phosphate as the vehicle carrier to evaluate the effects of decortication during bone grafting in defect areas surrounding particulate dentin-coated implants to determine the osteoconductivities of calcium phosphate cement (CPC-1 and CPC-2) mixed with SP-soln in a dog model Zhang et al. 2009 Dogs 6 Araújo & Lindhe 2009 Borges et al. 2009 Dogs 5 Dogs 7 Jung et al. 2009 Dogs 11 Parlar et al. 2009 Dogs 9 Roriz et al. 2009 Dogs 6 Morris et al. 2009 Chang et al. 2009 Dogs Dogs 7 4 Rothamel et al. 2009 Weng et al. 2009 Dogs Dogs 6 5 Iwata et al. 2009 Podaropoulos et al. 2009 Camarini et al. 2009 Simion et al. 2009 Dogs Dogs 4 4 Dogs Dogs 4 12 Manfrin Arnez et al. 2009 Sato et al. 2009 Simon et al. 2009 Gutta et al. 2009 Dogs 10 Dogs Dogs Dogs 6 4 4 Haze et al. 2009 Dogs 6 Wang et al. 2009 Alhezaimi et al. 2009 Santos et al. 2010 Dogs Dogs Dogs 6 5 6 Decker et al. 2010 Dogs 12 Jiang et al. 2010 Kwon et al. 2010 Dogs Dogs 4 5 to evaluate chitosan/collagen scaffolds combined with adenoviruses expressing either bone morphogenetic protein 7 (BMP-7), platelet-derived growth factor B (PDGF-B), or a combination of both BMP-7 and PDGF-B in bone defects around dental implant model in the dog to evaluate the more long-term effect on hard tissue formation and the amount of ridge augmentation that can occur by the placement of a xenogeneic graft in extraction sockets of dogs to evaluate the effectiveness of the acellular dermal matrix as a membrane for guided bone regeneration, in comparison with a bioabsorbable membrane to evaluate the soft-tissue reaction of a synthetic polyethylene glycol hydrogel used as a barrier membrane for guided bone regeneration compared with a collagen membrane and to test whether or not the application of this in situ formed membrane will result in a similar amount of bone regeneration as the use of a collagen membrane to evaluate the effects of various decontamination techniques and implant surface configurations on re-osseointegration of contaminated dental implants (with collage barrier) to evaluate the efficacy of a bioactive glass–ceramic and a bioactive glass placed in dental sockets in the maintenance of alveolar ridge and in the osseointegration of Ti implants to evaluate the potential of locally injected simvastatin (methylcellulose gel) in human-sized periodontal defects to compare the osseointegration of immediate implants in dogs in infection-free sites and in sites with periradicular lesions which were removed by simulated periradicular surgery to compare histologically the healing following vertical ridge augmentation using screwable, xenogenous deproteinized blocks or autologous bone blocks in dogs to evaluate guided bone regeneration in peri-implant defects following implantation of ß-tricalcium phosphate with and without osteoinductive recombinant human growth/differentiation factor-5. to examine multi-layered sheets of periodontal ligament (PDL)-derived cells for periodontal regeneration to histomorphometricaly compare the osteogenic potential of β-tricalcium phosphate alone or in a calcium sulfate matrix to evaluate the effectiveness of platelet-rich plasma in the process of new bone formation when associated with biomaterials to evaluate the efficacy of purified recombinant human platelet-derived growth factor, combined with a novel equine hydroxyapatite and collagen bone block, in providing vertical bone regeneration in critical-size defects simulating localized mandibular alveolar bone atrophy to evaluate the osteogenic potential of angiogenic latex proteins for improved bone formation and osseointegration of dental implants to evaluate histologically the effectiveness of the calcium phosphate cement for ridge augmentation of surgically created defects in the maxilla in beagle dogs to determine if extraction sites treated with platelet-rich fibrin matrix (PRFM) exhibit enhanced healing compared to sites treated with non-viable materials to identify the optimal pore size of barrier membranes for successful alveolar ridge reconstruction procedures, to determine if cortical perforations have any effect on bone regeneration, and to reiterate that bone graft containment is an important parameter for successful regeneration to find out whether the recombinant human amelogenin protein, which comprises 90% of the extracellular enamel matrix proteins, could alone bring about the regeneration of the tooth supporting tissues (periodontium) after induction of experimental periodontitis in the dog to evaluate porous b-tricalcium phosphate (b-TCP) combined with autologous osteoblasts to augment edentulous alveolar ridge in a canine model to evaluate histologically and histometrically the healing process in dehiscence-type defects treated by enamel matrix derivative to evaluate soft and hard tissue reactions to two different hydroxyapatites HAs (synthetic HA and natural HA) and bioactive glass implanted into the sockets immediately after extraction to evaluate the effect of implants fully or partially coated with rhBMP-2 and vacuum-dried using an industrial process on local bone formation and resident bone remodeling to evaluate the healing of class III furcation defects following transplantation of autogenous periosteal cells combined with b-tricalcium phosphate to evaluate periodontal wound healing/regeneration following an established clinical (benchmark) protocol including surgical implantation of recombinant human growth/differentiation factor-5 in comparison with that following implantation of recombinant human platelet-derived growth factor-BB combined with a particulate b-tricalcium phosphate biomaterial Lee et al. 2010 Dogs 5 Nunez et al. 2010 Shirakata et al. 2010 Stavropoulos & Wikesjö 2010 Suaid et al. 2010 Dogs Dogs Dogs 4 4 3 Dogs 6 Valderrama et al. 2010 Dogs 6 Wang et al. 2010 Yamashita et al. 2010 Dogs Monkeys 12 5 Yan et al. 2010 Dogs 6 Schwarz et al. 2010c Kwon et al. 2010b Lee et al. 2010b Dogs Dogs Dogs 12 5 15 Thoma et al. 2010 Dogs 5 Yamauchi et al. 2010 Dogs 5 Schwarz et al. 2010a Dogs 5 Usui et al. 2010 Schwarz et al. 2010b Dogs Dogs 8 4 Faria et al. 2010 Dogs 5 to evaluate the bone formation effect of amorphous calcium phosphate glass cement (CPGC) in a system of CaO-CaF2-P2O5-MgOZnO and to determine the influence of CPGC on periodontal regeneration in 1-wall intrabony defects in the mandibles of beagle dogs by comparing CPGC performance with that of biphasic calcium phosphate to investigate the effects of low concentrations of 17b-estradiol on human cementoblast proliferation and its possible regenerative potential in vivo to evaluate the effect of a basic fibroblast growth factor candidate treatment on periodontal healing in two-wall intrabony defects in dogs to evaluate the influence of defect dimensions on periodontal wound healing/regeneration in intrabony defects following implantation of a deproteinized bovine bone/collagen matrix under provisions for guided tissue regeneration to verify the regenerative potential of particulate anorganic bone matrix–synthetic peptide-15 in class III furcation defects associated or not with expanded polytetrafluoroethylene membranes. to test whether or not the presence of integrin-receptor–binding arginineglycine-aspartic acid improves the performance of the polyethylene glycol matrix supplemented with cys-PTH 1-34 when applied in acute defects around dental implants placed in the dog mandible at early healing time points (2 and 4 weeks) to evaluate the healing of surgically created alveolar bone dehiscences in beagle dogs following treatment with and without porous biphasic calcium phosphate to evaluate the periodontal regeneration achieved with the use of a synthetic anabolic peptide combined with either beta-tricalcium phosphate or an absorbable collagen spongeas the carrier to evaluate the quality and quantity of regenerated bone in periodontal regeneration, following topical application of recombinant human bone morphogenetic protein-2 and recombinant human beta nerve growth factor to furcation class III defects to evaluate the impact of guided bone regeneration and defect dimension on wound healing at chemically modified titanium implant surfaces to evaluate the effect of a novel recombinant human GDF-5 construct intended for onlay and inlay indications on periodontal wound healing/regeneration. to evaluate periodontal wound healing/regeneration following the application of rhGDF-5 on a particulate b-tricalcium phosphate carrier using an established defect model to test whether or not rhBMP-2/ACS combinations with allografts or a mesh enhance the amount of bone regeneration when performing lateral ridge augmentation procedures in the mandible to evaluate local tissue reaction around the b-tricalcium phosphate (b-TCP) block and compared results with b-TCP block grafting and periosteal expansion osteogenesis to histologically evaluate and compare a new prototype collagen type I/III-containing equine and a bovine derived cancellous bone block in a dog model to test the hypothesis that inorganic polyphosphate estimulates osteoblastic differentiation and polyphosphate metabolism for bone formation to evaluate (i) the effects of rhPDGF-BB on localized ridge augmentation using a natural bone mineral (NBM), and (ii) the influence of a collagen membrane (CM) on factor activity to investigate the healing, integration, and maintenance of autogenous onlay bone grafts and implant osseointegration either loaded in the early or the delayed stages