File
advertisement

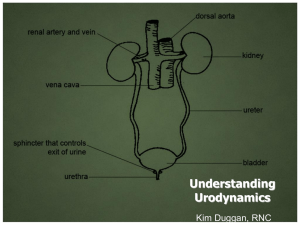
MICTURITION The bladder is composed of bands of interlaced smooth muscle( detrusor). The innervation of the body of the bladder is different from that of the bladder neck. The body is rich in beta adrenergic receptors. These receptors are stimulated by the sympathetic component of the autonomic nervous system (ANS). Beta stimulation, via fibers of the hypogastric nerve, suppress contraction of the detrusor. Conversely, parasympathetic stimulation, by fibers in the pelvic nerve, cause the detrusor to contract. Sympathetic stimulation is predominant during bladder filling, and the parasympathetic causes emptying. IN SHORT, The sympathetic nervous system predominates during the storage phase. Alpha adrenergic receptors in the base and neck of the bladder increase muscle tone. Simultaneously beta-adrenergic receptors in the body of the bladder depress detrusor tone. Two sphincters control the bladder outlet. The internal sphincter is composed of smooth muscle like the detrusor and extends into the bladder neck. Like the detrusor, the internal sphincter is controlled by the ANS and is normally closed. The primary receptors in the bladder neck are alphaadrenergic. Sympathetic stimulation of these alpha receptors, via fibers in the hypogastric nerve, contributes to urinary continence. Effect of sympathetic stimulation: relaxation of detrusor muscle; contraction of trigone and internal sphincter resulting in retention of urine. The external sphincter is histologically different from the detrusor and internal sphincter. It is striated muscle. Like skeletal muscle, it's under voluntary control. It receives its innervation from the pudendal nerve, arising from the ventral horns of the sacral cord. During micturition, supraspinal centers block stimulation by the hypogastric and pudendal nerves. This relaxes the internal and external sphincters and removes the sympathetic inhibition of the parasympathetic receptors. The result is unobstructed passage of urine when the detrusor contracts. The ureters pass between the layers of the detrusor and enter the bladder through the trigone. The ureters propel urine into the bladder. The bladder passively expands to accept urine. As the bladder expands and intravesicular pressure increases, the ureters are compressed between the layers of muscle, creating a valve mechanism. This valve mechanism limits the backflow of urine. The normal adult bladder can hold about 500 cc of urine. After emptying, the bladder may still retain about 50 cc residual volume. At about 150 cc of volume, stretch receptors in the detrusor begin signaling the CNS via afferent nerves; at 400 cc we are "seeking" an appropriate toilet. Healthy subjects usually experience the first need to void at a bladder volume of 150 ml and the urge to void at 300 ml. Summary: Normally, we are able to control where and when we void. This is largely because the cerebrum is able to suppress the sacral micturition reflex. If the sacral reflex is unrestrained, parasympathetic stimulation via the pelvic nerve causes detrusor contraction. Detrusor contraction is suppressed by alpha and beta sympathetic stimulation via the hypogastric nerve. In response to afferent stimulation, the cerebrum becomes aware of the need to void. If it is appropriate, the cerebrum relaxes the external sphincter, blocks sympathetic inhibition, the bladder contracts and urine is expelled. CONSCIOUS CONTROL The ability to control urination is dependent upon intact communication between the cerebrum, pons, sacral cord and peripheral nerves. We become aware of the need to void when the urine volume is about 150cc. Ascending afferent fibers relay sensation to the pons and then to the cerebrum. The cerebrum determines if the surroundings and social conditions are appropriate to void. If it is appropriate to void, the cerebrum switches the pons to emptying mode, which inhibits sympathetic output and pudendal nerve stimulation of the external sphincter. When the sympathetic system is no longer stimulated the parasympathetic system is activated to have maximum effect. Detrusor contraction ensues. AUTONOMIC INNERVATION Sympathetic: hypogastric nerve L1, L2. Effect of stimulation: 1. Relaxation of detrusor muscle; contraction of 2. trigone and internal sphincter resulting in retention 3. of urine. Parasympathetic: nervi erigentes aka pelvic splanchnic nerves, aka pelvic nerves synapse Effect of stimulation: 1. Contraction of detrusor muscle; 2. relaxation of trigone and internal 3. sphincter resulting in emptying of 4. bladder. at inferior hypogastric ganglion SOMATIC INNERVATION Anterior horn cells S2,S3,S4. Pudendal nerve(pubic nerve). Parts innervated Prostatic urethra and external sphincter. Effect of stimulation Parts innervated are under higher control . NEUROGENIC BLADDER Neurogenic bladder is a urinary problem in which the bladder does not empty properly. Depending on the type of neurological disorder causing the problem, the bladder may empty spontaneously (incontinence) or may not empty at all (retention with overflow leakage). DIFFERENT CLASSIFICATIONS OF NEUROGENIC BLADDER DYSFUNCTION I. ABOVE OR BELOW PONTINE MICTURITION CENTER / SACRAL CORD LESIONS WITH OR WITHOUT DAMAGE TO DETRUSOR NUCLEUS / LOWER MOTOR NEURON BLADDER 1. lesions above the pontine micturition center (e.g., stroke or brain tumor) producing an uninhibited bladder, 2. lesions between the pontine micturition center and sacral spinal cord (e.g., traumatic spinal cord injury or multiple sclerosis involving cervicothoracic spinal cord) producing an upper motor neuron bladder, 3. sacral cord lesions that damage the detrusor nucleus but spare the pudendal nucleus producing a mixed type A bladder, 4. sacral cord lesions that spare the detrusor nucleus but damage the pudendal nucleus producing a mixed type B bladder, 5. lower motor neuron bladder from sacral cord or sacral nerve root injuries. UNINHIBITED NEUROGENIC BLADDER DYSFUNCTION reduced awareness of bladder fullness and a low capacity bladder due to reduction of inhibition of the pontine micturition center (PMC) by cortical and subcortical structure damage. Urinary incontinence may occur with brain lesions occurring above the pontine micturition center, especially with bilateral lesions. Since the PMC is intact, the normal opposition of detrusor and internal/external sphincter tonus is maintained so there are no high bladder pressures developed that can lead to upper urinary tract damage. UPPER MOTOR NEURON NEUROGENIC BLADDER characterized by detrusor-sphincter dyssynergia (DSD) - simultaneous detrusor and urinary sphincter contraction producing high pressures in the bladder leading to vesicoureteral reflux that can produce renal damage. bladder and sphincters spastic, especially if lesions are above T10 level (above the sympathetic autonomic nervous system innervation of the bladder). bladder capacity is usually reduced due to the high detrusor tonus If detrusor pressure exceeds internal/external urinary sphincter pressure in the proximal urethra, then incontinence may occur. MIXED TYPE A NEUROGENIC BLADDER (the more common of the mixed type bladders) detrusor nucleus damage renders the detrusor flaccid (also referred to as detrusor areflexia intact pudendal nucleus is spastic producing a hypertonic external urinary sphincter. bladder is large and has low pressure, so the spastic external sphincter produces urinary retention. detrusor pressure is low so upper urinary tract damage from vesicoureteral reflux does not occur, and incontinence is uncommon. MIXED TYPE B NEUROGENIC BLADDER characterized by a flaccid external urinary sphincter due to the pudendal nucleus lesion bladder is spastic due to the disinhibited detrusor nucleus. bladder capacity is low but vesicular pressures are usually not elevated since there is little outflow resistance. This leads to problems with incontinence, however. LOWER MOTOR NEURON NEUROGENIC BLADDER the sacral micturition centers or related peripheral nerves are damaged though the thoracic sympathetic nervous system outflow to the lower urinary tract is intact. bladder capacity is large since detrusor tone is low (detrusor areflexia) and internal urinary sphincter innervation is intact. Despite the low detrusor pressure, overflow urinary incontinence and urinary tract infections are not uncommon. II. SPASTIC / FLACCID / UNINHIBITED III. FLACCID OR SPASTIC BLADDER (based on above or below T12) Spinal cord injury T12 or above- reflex, automatic or spastic bladder - automatic, involuntary control of the bladder so when the bladder fills above a certain level it contracts and urine flows out automatically Spinal cord injury below T12- atonic, flaccid bladder - bladder has no muscle tone and doesn't contract to empty automatically. Instead, it continues to fill and small amounts of urine may eventually dribble out. MICTURITION - storage of urine to micturition depends on intensity of afferent input (stretching of bladder wall, increased intravesical pressure) DURING URINE STORAGE (no micturition occurs) low level of afferent activity causes - efferent input via somatic pudendal nerve (S2-4) to urethral sphincter – contraction efferent input via hypogastric nerve (sympathetics T11-L1) to bladder neck – contraction inhibition of detrusor muscle via hypogastric nerve --- relaxation MICTURITION: (events) - high level of afferent activity causes signals via pelvic nerve up to brainstem and cortex, initiating the voiding mechanism pontine micturition center causes inhibition of pudendal nerve – relaxation of urethral sphincter inhibition of hypogastric nerve --- relaxation of bladder neck efferent input to pelvic nerve (parasympathetics) – detrusor contraction summary: MICTURITION REFLEX 1. Stretch of bladder wall 2. Increase afferent activity in sensory neurons 3. Increase parasympathetic activity 4. Increase detrusor muscle contraction 5. Inhibition of pudendal nerve 6. Results in skeletal muscle relaxing 7. Urine voided Detrusor External Sphincter Dyssynergia - contraction of bladder and external sphincter at the same time - caused by injury between brainstem and sacral cord Autonomic Dysreflexia, sweating and vasoconstriction below lesion - syndrome of exaggerated sympathetic activity in response to a noxious stimuli (distended bladder in a para or quadriplegic) below the lesion usually above T6, 7 - hypertension, reflex bradycardia - treatment: remove noxious stimulus (insert a catheter), parenteral ganglionic or alphablockers or chlorpromazine INCONTINENCE the involuntary passage of urine sufficiently severe to cause social or hygiene problems most frequent in the elderly Classification 1. Total: constant or periodic loss of urine without warning exstrophy of bladder epispadias vesico-vaginal fistulas ectopic ureteral orificas 2. Stress: urine loss with sudden increase in intra-abdominal pressure (e,g, coughing or sneezing) weakness of pelvic floor musculature (child bearing, (previous abdominal pelvic surgery) damage weakness of urethra or sphincter 3. Urge: urine loss due to uninhibited bladder contractions local bladder irritation (eg cystitis, stone, tumor) CNS disorder 4. Overflow: urine loss when intravesical pressure exceeds urethral pressure obstructive (eg Benign Prostatic Hypertrophy) hypotonic bladder detrusor –sphincter dyssynergia 5. Functional: urine loss caused by inability to reach toilet in time physical immobility MICTURITION REFLEX 1. as the bladder fills with urine, increased pressure stimulates the stretch receptors which stimulates the parasympathetic nerves 2. high level of afferent activity causes signals via pelvic nerve up to brainstem and cortex... 3. pontine micturition center causes inhibition of pudendal nerve – relaxation of urethral sphincter 4. inhibition of hypogastric nerve (sympathetic) --- relaxation of bladder neck 5. efferent input to pelvic nerve (parasympathetics) – detrusor contraction 6. When the detrusor muscle contracts, it pulls open the internal urethral sphincter (the muscle at the base of the bladder). (The internal urethral sphincter is closed when the detrusor muscle is relaxed. ) . ...message is sent to the brain that the bladder is becoming full, resulting in the urge to void. This initiates the voiding mechanism. 7. contraction of the detrusor muscle produces a change in the shape in this muscle, which opens this sphincter... Urine is released through the urethra summary: MICTURITION REFLEX 1. Stretch of bladder wall 2. Increase afferent activity in sensory neurons 3. Increase parasympathetic activity 4. Increase detrusor muscle contraction 5. Inhibition of pudendal nerve 6. Results in skeletal muscle relaxing 7. Urine voided INCONTINENCE the involuntary passage of urine sufficiently severe to cause social or hygiene problems most frequent in the elderly Classification : TOTAL, STRESS, URGE, OVERFLOW, FUNCTIONAL TOTAL: constant or periodic loss of urine without warning exstrophy of bladder epispadias vesico-vaginal fistulas ectopic ureteral orificas STRESS: urine loss with sudden increase in intra-abdominal pressure (e,g, coughing or sneezing) weakness of pelvic floor musculature (child bearing, (previous abdominal pelvic surgery) damage weakness of urethra or sphincter URGE: urine loss due to uninhibited bladder contractions local bladder irritation (eg cystitis, stone, tumor) CNS disorder OVERFLOW: urine loss when intravesical pressure exceeds urethral pressure obstructive (eg Benign Prostatic Hypertrophy) hypotonic bladder detrusor –sphincter dyssynergia FUNCTIONAL: urine loss caused by inability to reach toilet in time physical immobility PELVIC FLOOR Kegel exercise, consists of repeatedly contracting and relaxing the muscles that form part of the pelvic floor done to reduce urinary incontinence, reduce premature ejaculation as well as to increase the size and intensity of erections. RENAL FAILURE EFFECTS OF COMPLETE RENAL FAILURE ON THE BODY: 1. Effects of complete renal failure on the body: 2. Generalized edema resulting from water and salt retention 3. Hypertension resulting from water and salt retention 4. Uremia due to increase in urea and other nonprotein nitrogens (azotemia) 5. Acidosis resulting from failure to excrete normal acidic products 6. Anemia caused by decreased erythropoietin 7. Osteomalacia caused by decreased production of active vitamin D and by phosphate retention Treatment of Renal Failure by Dialysis with an Artificial Kidney Severe loss of kidney function - renal failure a threat to life and requires removal of toxic waste products and restoration of body fluid volume and composition toward normal. accomplished by dialysis with an artificial kidney. BASIC PRINCIPLES OF DIALYSIS Blood flows continually between two thin membranes of cellophane Outside the membrane is a dialyzing fluid membranes of cellophane - porous to allow constituents of plasma, except the plasma proteins, to diffuse in both directions—from plasma into the dialyzing fluid or from the dialyzing fluid back into the plasma. If a substance is greater in the plasma than in the dialyzing fluid, there will be transfer of the substance from the plasma to the dialyzing fluid.