ROSEAU AREA HOSPITAL & HOMES, INC.
advertisement

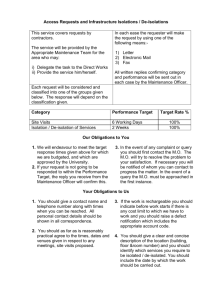
LIFECARE MEDICAL CENTER – Guideline ----------------------------------------------------------------------------------------------------------------------------DEPARTMENT: Home Care SUBJECT: Guidelines for Frequency of Visits for Palliative Care Clients ----------------------------------------------------------------------------------------------------------------------------PREPARED BY: APPROVED BY: PURPOSE: It is the intent of LifeCare Medical Center to see all clients/patients/residents that are referred for palliative care. The following is a guideline for service delivery for clients/residents/patients in varied care settings serviced by LifeCare Medical Center. Referrals for consultation or visits by the palliative care teams can be made by physicians, acute care, homecare/hospice, family members, or the client. The team consists of a nurse, social worker, spiritual care leader, and aid. The role of the RN will include completion of a comprehensive assessment on client; ongoing assessment and monitoring of symptoms; symptom management; recommendations to physician for medical interventions utilizing the Symptom Management Guidelines; medication set-up, teaching and assessment of effectiveness; disease management teaching; assess for need of aide; aide supervision; referral for durable medical equipment; assess for need of rehab services and determination if needed in home or as an outpatient; coordinate obtaining needed supplies for client and family; in coordination with the social worker assess for need for referral to community resources and to assess need/frequency of family conferences. Initial assessment will be done within 48 hours of receipt of referral or physician ordered start of care date. The SW will complete an assessment of social and emotional factors related to client’s illness, need of care, response to treatment and adjustment to care; counseling for long-range planning and decision making; community resource planning and promotion of community centered services; provision of medical social services to family members on a short-term basis if the basis of the service is necessary to resolve a clear and direct impediment to the effective treatment of the client’s medical condition or his/her rate of recovery; short-term therapy with goal oriented interventions directed toward management of a terminal illness; a social history; assess the availability of the caregiver and how the caregiver is coping. Assess the client’s perception of his/her pain; assess client’s affect/mood; assess and discuss life goals and goals client wishes to complete before end of life; assist with Health Care Directives/POLST/wills; identification of any ethnic/cultural considerations. Specified physician orders are required for care related to the client’s illness if problem resolution is associated with high risk indicators endangering the client’s mental and physical health including: abuse/neglect, inadequate food/medical supplies and high risk of suicide potential. In collaboration with the RN will assess the need for family conference. Completion of the initial assessment will be completed within 2 business days of start of care. The Chaplain will complete an assessment of the client’s spiritual needs and the client’s meaning of life. A referral to coordinate ongoing spiritual care with the client’s community spiritual care leader will be made when there is a community spiritual care leader involved with the client and/or family. Charting guidelines are attached. A copy of all documentation will be made and kept on file in the home care office for all clients served. All others will have a hard chart in the home care office. A master list of all clients will be compiled and kept in the homecare office. 1 Nursing home residents: 1. Whenever possible on the initial visit, a joint visit will be done with the RN and SW. Comprehensive assessments will be completed by the RN, SW, and Chaplain. 2. An interdisciplinary family conference may be offered, set up and completed by the palliative care team. 3. The RN may do 1 to 2 visits as deemed appropriate in follow up to the comprehensive assessment and recommendations for symptom management. 4. The SW may do 1 to 2 visits as deemed appropriate in follow up to the comprehensive assessment. 5. Total time for palliative team consult should be approximately 20 hours in total for all disciplines. Acute care patients: 1. A onetime consultative visit will be made by the RN, SW and Chaplain to assess symptom management and address short term planning needs of the patient and family/support system. 2. Consultative visits can be requested by discipline however the physician must first have informed the patient of the palliative status prior to the consultative visit. 3. Upon completion of the consultative visit(s) team members will document recommendations for symptom management; disease management and results of the assessment in the progress notes in the acute care medical record. 4. A total of 3 hours each, will be available for nursing, social and spiritual care assessments. Client(s) residing in the community: own home, apartment, assisted living, etc. 1. Payment source will be assessed, could include- Medicare, Medical Assistance, County Waivers (AC, EW), VA, Private Insurance, private pay or sliding fee scale private pay or charity care. 2. A comprehensive assessment will be completed by RN, SW, and chaplain. Whenever possible a joint initial visit will be done by the RN and SW. 3. An interdisciplinary – family conference may be offered, set-up and completed by the palliative care team 4. A 60 day episode of care (485) will be completed following the comprehensive assessment 5. Services clients could receive during the initial 60 day episode include: a. Skilled nursing (SN) RN visits and assessments would be 1-2 times the first week, weekly for 3 weeks and then every other week for 3 weeks. The RN will determine the frequency of SN RN visits based on the client need; the need may be greater than above or less than above, based on nurse’s assessment. It is anticipated that each visit should be 2 hours or less for a total of 8 visits in a 60 day episode (14-16 hours in a 60 day episode). b. SW visits for assessment: weekly for 2 weeks then one more time during the initial 60 day episode (2 hours per visit/4 total visits/8 hours per client/episode). c. An initial Chaplain Assessment visit will be made, if no church affiliation: 1 more visit per 60 day episode (2 hours /visit; 2 total visits for a total of 4 hours/60 day episode). d. Aide services as needed not to exceed 2 visits per week for 9 weeks (18 visits; 2 hours each for a total of 36 hours/60 day episode). e. PT/OT/SLP: a onetime visit as deemed necessary from the initial comprehensive assessment or as deemed necessary during the 60 day episode of care by the RN (2 hours per visit). 6. Total (all disciplines) staff time could receive funded or non-funded would be 62 hours per initial 60 day episode. 2 Subsequent 60 day episode for client residing in community 1. SN RN visits every other week to monthly; 2 hours per visit; 2-5 visits per 60 day episode- 4 10 hours per episode 2. SW 2 visits per episode- 4 hours total 3. Chaplain – 1 visit per episode- 2 hours total 4. Aide services not to exceed 2 visits per week for 9 weeks at 2 hours per visit for a total 36 hours per 60 day episode 5. Ongoing rehab services will be provided under the Medicare benefit if the client continues to meet eligibility criteria. Home Care-Palliative Care Assessment and Charting Guidelines Assessment Guidelines for client in the community Comprehensive Assessment: Nurse Omaha and OASIS if skilled and homebound & Medicare or Medical Assistance pay source Focus on disease/condition that makes client palliative-disease teaching Medication review Symptom management-pain, nausea, diarrhea, constipation, sob, anxiety Physician orders for change in medications/new medications to treat symptoms Nursing interventions to treat symptoms; provide comfort Prevention of exacerbation-what’s the plan Prevent hospital and ER visits DME needs SW Social emotional well being of client and family Short term and long term planning Finances including helping client to find a pay source for home care-sliding fee, county programs, private pay DNR form/POLST Depression Screen Chaplain Spiritual assessment; meaning of life Referral to primary spiritual caregiver Charting Guideline-complete the following in the chart-electronic and paper Referral page Medication 485 Omaha OASIS –skilled and homebound 3 Pain Assessment Skin Assessment Depression screen-?SW complete Self Assessment tool of symptoms Diabetic Foot Care Care Plans Admit signature forms Champ Form DNR/POLST-SW complete Assessment Guidelines for client in acute care Comprehensive Assessment: Nurse Omaha Focus on disease/condition that makes client palliative-disease teaching Medication review Symptom management-pain, nausea, diarrhea, constipation, sob, anxiety Recommend Physician orders for change in medications/new medications to treat symptoms Recommend Nursing interventions to treat symptoms; provide comfort Prevention of exacerbation-what’s the plan Prevent hospital and ER visits DME needs SW Social emotional well being of client and family Short term and long term planning Finances including helping client to find a pay source for home care-sliding fee, county programs, private pay Depression Screen Chaplain Spiritual assessment; meaning of life Referral to primary spiritual caregiver Charting Guideline-complete the following in the chart-electronic and paper Referral page Medication-print from acute care chart Omaha Pain Assessment Skin Assessment Depression screen-SW complete Self Assessment tool of symptoms Diabetic Foot Care Care Plans Champ Form 4 Assessment Guidelines for client in the nursing home Comprehensive Assessment: Nurse Omaha Focus on disease/condition that makes client palliative-disease teaching Medication review Symptom management-pain, nausea, diarrhea, constipation, sob, anxiety Physician orders for change in medications/new medications to treat symptoms Nursing interventions to treat symptoms; provide comfort Prevention of exacerbation-what’s the plan Prevent hospital and ER visits DME needs SW Social emotional well being of client and family Short term and long term planning Finances including helping client to find a pay source for home care-sliding fee, county programs, private pay DNR form/POLST Depression Screen Chaplain Spiritual assessment; meaning of life Referral to primary spiritual caregiver Charting Guideline-complete the following in the chart-electronic and paper Referral page Medication Speed letter for physician orders for follow up visits Omaha Pain Assessment Skin Assessment Depression screen-?SW complete Self Assessment tool of symptoms Diabetic Foot Care Care Plans-if follow up visits Admit signature forms Champ Form DNR/POLST-SW complete PP-DRAFT/ Original Date: Reviewed: Revised: COPIES ROUTED TO: 5