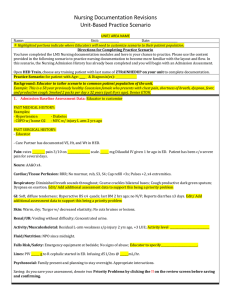
Unit Practice Template Key
advertisement

Nursing Documentation Revisions Unit-Based Practice Scenario UNIT/ AREA NAME Name: ____________________ Unit: ______________ Date: ___________________ Highlighted portions indicate where Educators will need to customize scenario to their patient population. Directions for Completing Practice Scenario You have completed the LMS Nursing documentation modules and here is your chance to practice. Please use the content provided in the following scenario to practice nursing documentation to become more familiar with the layout and flow. In this scenario, the Nursing Admission History has already been completed and you will begin with an Admission Assessment. Open HED Train, choose any training patient with last name of ZTRAINHEDUP on your unit to complete documentation. Practice Scenario: for patient with Age: ____ & Diagnosis(es): _______________ Background: Educator to tailor scenario to common patient population of the unit. Example: This is a 58 year previously healthy Caucasian female who presents with chest pain, shortness of breath, dyspnea, fever, and productive cough. Smoked 2 packs per day x 32 years (quit 8 yrs ago). Denies ETOH. 1. Admission Baseline Assessment Data: Educator to customize PAST MEDICAL HISTORY: Examples: - Hypertension - Diabetes - COPD w/ home O2 - MVC w/ injury L arm 2 yrs ago PAST SURGICAL HISTORY: - Educator - Care Partner has documented VS, Ht, and Wt in HED. Pain: rates _________ pain 3/10 on ________________ scale. ______ mg Dilaudid IV given 1 hr ago in ED. Patient has been c/o severe pain for several days. ( Pain will automatically be listed as a problem when pain score documented) Neuro: AA&O x4. (WNL) Cardiac/Tissue Perfusion: RRR; No murmur, rub, S3, S4; Cap refill <3s; Pulses +2, x4 extremities. (WNL) Respiratory: Diminished breath sounds throughout; Course crackles bilateral bases; Cough productive dark green sputum; Dyspnea on exertion. Edit/ Add additional assessment data to support this being a priority problem (Problem identified) GI: Soft, diffuse tenderness; Hyperactive BS x4 quads; last BM 2 hrs ago; no N/V; Reports diarrhea x3 days. Edit/ Add additional assessment data to support this being a priority problem (Problem identified) Skin: Warm, dry; Turgor w/ decreased elasticity; No cuts bruises or lesions. . (WNL) Renal/UR: Voiding without difficulty; Concentrated urine. . (WNL) Activity/Musculoskeletal: Residual L-arm weakness s/p injury 2 yrs ago, +3 LUE; Educator to specify - Activity level ____________________________ . (WEL) Fluid/Nutrition: NPO since midnight. Falls Risk/Safety: Emergency equipment at bedside; No signs of abuse; Educator to specify__________________________.(WNL) Lines: PIV ______ g to R cephalic started in ED. Infusing d51/2ns @ ______mL/hr. Psychosocial: Family present and planning to stay overnight. Appropriate interactions. (WNL) Saving: As you save your assessment, denote two Priority Problems by clicking the !! on the review screen before saving and confirming. Nursing Documentation Revisions Unit-Based Practice Scenario 2. Plan (Hint: PLAN tab) 1. Select a goal for each of the priority problems ( pain, GI &Resp) 2. Educator to complete :Specify Priority Problems for Pain, GI & Respiratory and goals (One goal should be from dropdown menu while second goal should be noted as “Other” and annotate) 3. Education & Nursing Interventions: Document the following (Hint: Education & Interventions tab) Care Contact: Educator to complete: preferred language and learning mode, Name, role & phone # Education Session: patient and Care contact 1, were given handouts,and verbalized understanding of VUMC general & unit specific education and education re: meds for pain management. Interventions Educator to complete: Add to items below to fit unit based scenario Pain control care : medication & positioning Strict Intake & Output O2 placed ______________ Incentive spirometer Other interventions per educator 4. Re-Assessment: You have just performed a focused re-assessment. Document the following: Re-assessment to denote unchanged except. There would not typically be data in all of these categories. Please select 1-2 areas for documentation of assessment changes specific to your patient. Pain: per educator Cardiac/Tissue Perfusion: Tachycardic, HR 135. Notification of the Provider: document that Dr Smith was notified of the HR of 135. Reports that they will come see pt and will enter orders for EKG. Hint: Communication/ Event Note Respiratory: Breath sounds inspiratory wheeze & rhonci noted throughout; Dyspnea at rest. GI: per educator 5. End of Shift: It is now the end of your shift. Document the following: Response to Care/Recommendations (Hint: PLAN tab) Goal attainment – address goals set at beginning of shift o Pain goal: per educator o Resp goal per educator o GI goal per educator Question: Since there will be several weeks before all units have transitioned to the new tabs and documentation model, if your unit has gone live but a patient transfer to you from a NON IMPLEMENTED unit, what will be the best way to view the documentation from the sending unit? (Remember, documentation will not be shared between the old and the new tabs) Answer: Click on Chart in the top tool bar and select the appropriate tab – or click on the drop down for tabs and select the appropriate tab. Upon completion, please sign and return to Nursing Educator by Signature: DATE . Date: