Oral Drug Therapy Guidelines in Surgical Patients
advertisement

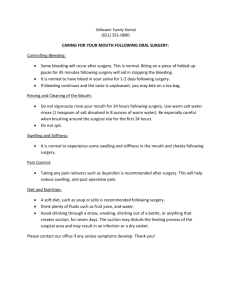
ORAL DRUG THERAPY GUIDELINES IN SURGICAL PATIENTS At the pre-operative assessment it is important that a full medication history is taken prior to any procedure, including herbal, homeopathic and topical medications. The pre-assessment nurse practitioner, pharmacist or doctor, as applicable, must inform the patient which medicines should be stopped and which medicines should be continued. For the medicines that are to be stopped, patients must be told how long before the day of surgery the medicines should be stopped and when they are likely to be restarted. If a patient requires emergency surgery then the surgical team should liaise with the anaesthetist to discuss which drugs should and should not be stopped prior to surgery and when to restart any discontinued drugs. A patient may be ‘Nil-by-mouth’ for several reasons, e.g. non-functional gut, lack of swallowing reflex, patient unconscious or prior to surgery. Nausea or vomiting may also inhibit the use of oral medicines. Surgery is not an indication to stop the majority of medications a patient may be taking on admission. Where there is a need for medication to continue because the oral route is inappropriate consideration should be given to alternative routes or products. The table below aims to clarify those drugs which should be continued and those that should be stopped prior to surgery with suggested alternative routes when the oral route is unsuitable. Please also consult Pharmacy for guidance on the administration of drugs through enteral feeding tubes for alternatives to solid oral dosage forms for patients unable to swallow their medication. When changing the route of administration of a drug care should be taken to ensure that the appropriate dose and frequency is prescribed, as these may not be the same as for the oral route. Patients are at risk of aspirating their stomach contents during general anaesthesia. They are therefore usually prevented from eating at least 6 hours pre-surgery and can drink only water between 6 and 2 hours pre-operatively. Water leaves the stomach within 2 hours of ingestion and therefore, medicines can be given up to 2 hours before surgery with water. General rule of thumb: do not stop analgesia, anti-epileptics, bronchodilators, corticosteroids, antidepressants, antipsychotics, benzodiazepines, Parkinsons disease medicines, cardiovascular drugs, glaucoma drugs, thyroid or anti-thyroid drugs and peptic ulcer drugs prior to surgery. Stop all herbal medicines 2 weeks prior to surgery. The table below is not exhaustive, although most drug groups not included in the table can be omitted pre/peri-operatively. If in doubt contact an anaesthetist or the ward pharmacist for further advice. Please note that recommendations for stopping for major surgery may differ to those for minor surgery Key to table Drugs that are usually stopped Benefits of stopping need to be weighed against risks. Depends on Consultant surgeon / anaesthetist preference and surgery type Drugs that must be continued to prevent relapse of the treated condition or to avoid the effects of drug withdrawal Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 1 of 26 BNF Class / Drug group (examples) Risk Use pre-op. when NBM Alternative post-op if unable to take po medication 1. GASTRO-INTESTINAL 1.1 Antacids Reduce risk of acid aspiration. (e.g. co-magaldrox, GavisconR) Continue 1.2 Antispasmodics, motility stimulants (e.g. mebeverine) Increased risk of ileus. Discontinue during periods of NBM post operatively- prolonged periods of NBM increase the risk of paralytic ileus 1.3.1 H2 receptor antagonists (e.g. ranitidine) Reduce risk of acid aspiration. Continue i.v. ranitidine 50mg tds 1.3.5 Proton pump inhibitors (e.g. omeprazole) Reduce risk of acid aspiration. NB: lansoprazole may increase action of vecuronium Continue i.v. proton-pump inhibitor 1.6 Laxatives Note contra-indications Fybogel - intestinal obstruction and colonic atony Docusate - abdominal pain , nausea, vomiting or intestinal obstruction Senna - undiagnosed acute or persistent abdominal symptoms Macrogols – intestinal perforation/obstruction, paralytic ileus, severe inflammatory conditions of the intestinal tract Continue but note contra-indications Omit if laxative action is undesirable Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 2 of 26 Management NB increased risk of C. difficile associated with PPI’s BNF Class / Drug group (examples) Risk Use pre-op. when NBM Alternative post-op if unable to take po medication Management 2. CARDIOVASCULAR 2.1 Digoxin Increased toxicity with suxamethonium Arrhythmias Continue. 2.2 Diuretics -thiazide and loop (e.g. bendroflumethiazide, furosemide) Diuretics - potassium sparing (e.g. amiloride, spironolactone) Arrhythmias Prolonged N/M block Hypokalaemia may provoke paralytic ileus Tissue damage Reduced kidney perfusion Hyperkalaemia 2.3 Antiarrhythmics To prevent relapse of arrhythmia For diuretics the ESC guidelines recommend: Hypertensive patients discontinue low dose diuretics on the day of surgery and resume orally when possible. Heart failure patients continue up to the day of surgery, resume iv perioperatively and continue orally when possible. Electrolyte disturbances be corrected before surgery Continue i.v.digoxin. Convert po to iv dose using conversion factor (0.65 tablets, 0.80 elixir), e.g digoxin 125micrograms tablet 100micrograms elixir 80 micrograms i.v. i.v. diuretics (max rate for furosemide = 4mg/min) Monitor digoxin level and K+. Level checked 6-8hrs after dose. Add potassium to fluids where needed. Monitor U+E’s Use i.v. alternative within same class with ECG monitoring ECG monitoring. Monitor U+E’s. Hypokalaemia can predispose to digoxin toxicity Some antiarrhythmics prolong the duration of action of non depolarising neuromuscular blockers 2.4 Beta blockers (e.g. atenolol, propranolol) Hypotension Bradycardia Bronchospasm Continue- improves c/v stability. Betablockers should not be discontinued abruptly in the peri-operative period. Rebound if withdrawn. In post-thyroidectomy, dose may be gradually tapered to zero. Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 3 of 26 Give alternative i.v. beta-blocker (rarely needed) or GTN patch if patient symptomatic Monitor BP, fluids,U+E’s Omit if bradycardic Monitor BP and pulse BNF Class / Drug group (examples) Risk Use pre-op. when NBM Alternative post-op if unable to take po medication 2.5.1 Vasodilators (e.g. hydralazine) Reflex tachycardia Hypotension. Continue 2.5.2 Central-acting antihypertensives (e.g. clonidine, methyldopa) 2.5.4 Alpha blockers (e.g. doxazosin) Hypotension Rebound hypertension if withdrawnhypertensive crisis with one missed dose. Continue. Hypotension Continue- improves c/v stability. However, if for urinary retention and the patient is catheterised may withhold if at risk of hypotension. GTN patch or, if BP remains high, alternative i.v. antihypertensive agent If prescribed for hypertension ONLY, they may be held on the morning of surgery. Longer acting drugs may need omitting on the day before and day of surgery. GTN patch or, if BP remains high, alternative i.v. antihypertensive agent / i.v. diuretic. If Prescribed for heart failure +/or MI continue as per the European Society of Cardiology guidelines and discuss with the anaesthetist. Some ACE inhibitors absorbed s/l, e.g. captopril 2.5.5.1 ACE inhibitors (e.g. short-acting :captopril long-acting: lisinopril) 2.5.5.2 Angiotensin II antagonists (e.g. losartan) Hypotension (risk increases if volume depleted, be aware if substantial fluid shifts or bleeding is anticipated). Perioperative ACEI’s carry a risk of hypotension under anaesthesia, in particular following induction and concomitant beta-blocker use. Renal failure Reduced cerebral blood flow i.v. alternatives available Patients with a recent MI or clinically unstable must be reviewed by an anaesthetist. Note substitution of shorter acting drugs (e.g. captopril) may allow more flexibility for patients with post-operative labile blood pressure. For patients on 2 medicines that affect the renin angiotensin-aldosterone system (e.g. ACEI+AIIRA or ACEI + aliskiren or AIIRA + aliskiren) discuss with the anaesthetist Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 4 of 26 Management Monitor BP and pulse Monitor BP Monitor BP If for urinary retention then should discontinue post TURP Monitor BP and U+E’s. Caution NSAIDS. Resume cautiously postoperatively as long as the patient is not hypotensive and has normal renal function. BNF Class / Drug group (examples) Risk Use pre-op. when NBM Alternative post-op if unable to take po medication Management For patients on combination products such as ACEI / AIIRA with diuretic or ACEI / AIIRA with calcium channel blocker discuss with the anaesthetist 2.5.5.3 Renin inhibitors (e.g. aliskiren) 2.6.1 Nitrates Hypotension can occur in patients with marked volume depletion. Hypotension Continue 2.6.2 Calcium antagonists Hypotension Bradycardia(verapamil) Additive effect with enflurane, halothane Continue --diltiazem, - verapamil -dihydropyridines (nifedipine, amlodipine) 2.6.3 K+ channel activators (e.g. nicorandil) Additive effect with isoflurane Hypotension Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Continue Topical, buccal, sublingual and iv forms available. GTN patch or, if BP remains high, alternative i.v. antihypertensive agent. Avoid sublingual nifedipine capsules (associated with increased risk of stroke) Monitor BP Alternative anti-anginals (see nitrates) Monitor BP Refer to Trust Oral Anticoagulant Guidelines LINK / Anticoagulation guidelines for Neuraxial procedures LINK 2.8 AnticoagulantsParenteral Heparin, LMWH, Fondaparinux (see SPC re dose, timing, duration etc) Vitamin K antagonists -Oral Anticoagulants (e.g. warfarin) Continue Haemorrhagic risk if continued. Risk of peri-operative thromboembolism if stopped Refer to Trust Oral Anticoagulant Guidelines. LINK Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 5 of 26 See oral anticoagulant guidelines Monitor BP and pulse For information regarding epidural analgesic infusions and anticoagulants see the CDDFT policy for the management of Epidural Analgesia Infusions INR, platelet counts (>5 days of heparin) Check BNF for interacting drugs. BNF Class / Drug group (examples) Direct thrombin inhibitors – Dabigatran Risk Haemorrhagic risk No antidote for rapid reversal in emergencies Refer also to Anticoagulation guidelines for Neuraxial procedures. LINK Use pre-op. when NBM Electives CrCl<50ml/min: stop 3 to 5 days pre-op* CrCl ≥50ml/min: stop 1 to 2 days pre-op *also consider the longer withholding period in all circumstances where complete haemostasis required regardless of CrCl (e.g. major surgery, spinal puncture, spinal/epidural catheter) Bridging not required Emergencies Delay at least 12 hours where possible. Balance risk/benefit if delay not feasible. Seek expert haematology advice Alternative post-op if unable to take po medication Before resuming ensure: CrCl>30ml/min >6hrs since epidural removal Haemostasis adequate Low bleeding risk resume 6 to 8hrs post-op High bleeding risk / major surgery resume ≥48hrs post-op consider reduced dose initially prescribe standard LMWH prophylaxis until drug restarted Management Normal/near-normal aPTT or thrombin time on morning of surgery; renal function (Cockcroft-Gault estimation of CrCl) When restarting, give 0-2 hours before next dose of LMWH would have been due. Direct factor Xa inhibitors - Rivaroxaban Refer also to Anticoagulation guidelines for Neuraxial procedures. LINK Haemorrhagic risk Prothrombin complex (Beriplex) may reverse in emergencies Electives CrCl<50ml/min: stop 3 to 5 days pre-op* CrCl ≥50ml/min: stop 1 to 2 days pre-op *also consider the longer withholding period in all circumstances where complete haemostasis required regardless of CrCl (e.g. major surgery, spinal puncture, spinal/epidural catheter) Bridging may be required in those receiving drug for recurrent VTE, particularly if surgery within 4 weeks of an event – seek haematology advice. Emergencies May be able to reverse with Beriplex. Seek expert haematology advice Prescribe standard LMWH prophylaxis until drug restarted Before resuming ensure: CrCl>30ml/min >6hrs since epidural removal Haemostasis adequate Low bleeding risk resume 6 to 8hrs post-op High bleeding risk / major surgery resume ≥48hrs post-op consider reduced dose initially prescribe standard LMWH prophylaxis until drug restarted When restarting, give 0-2 hours before next dose of LMWH due. Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 6 of 26 Normal/near-normal aPTT or thrombin time on morning of surgery; renal function (Cockcroft-Gault estimation of CrCl BNF Class / Drug group (examples) 2.9 Antiplatelets Risk -Aspirin Haemorrhagic risk. Depends on surgery and / or choice of anaesthesia, i.e. epidural -platelet P2Y12 receptor blockers (e.g. clopidogrel, prasugrel, ticagrelor and ticlopidine) Many patients take both aspirin and platelet P2Y12 receptor blocker therapy to prevent coronary stent thrombosis (which can be catastrophic). It is essential to consider: why the patient is on antiplatelet therapy* risk of thrombosis if stopped risk of bleeding if continued site and nature of surgery *Aspirin Primary prevention can stop; secondary prevention, may require further discussion with surgeon / anaesthetist. Dipyridamole Haemorrhagic risk when used in combination with aspirin, warfarin or clopidogrel Use pre-op. when NBM Aspirin should only be discontinued if the bleeding risk outweighs the potential cardiac benefit. If perioperative haemorrhage is a concern and the patient has not suffered a previous coronary syndrome, cerebrovascular event, angina or AF then aspirin (or clopidogrel if aspirin intolerant) will need to be stopped 7-10 days prior to surgery to reduce bleeding risk. Confirm with surgeons regarding local preferences. DUAL THERAPY should be continued for at least the minimum recommended duration*. If surgery cannot be delayed beyond this then contact the cardiologist and surgeon for advice. Seek advice in patients with severe IHD, history CVA/TIA or other high risk factors, e.g. cardiac stents, where may be safer to continue. *Drug-eluting stents : essential to continue dual therapy for ONE year ACS treated with bare metal stents or medically (stable patients) : preferable to continue dual therapy for 1 year but P2Y12 agents can be stopped after 3 months if high risk of bleeding and surgery cannot be delayed As above consider balance between bleeding risk and thrombotic risk. If used a sole agent, does not need to be stopped. Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 7 of 26 Alternative post-op if unable to take po medication Management Continuation may cause perioperative haemorrhage. Discontinuation may increase the risk of vascular complications. Can restart immediately post-op. providing risk of bleeding no longer significant. The 2008 ACCP guidelines on antithrombotic therapy recommend resuming aspirin approximately 24 hours (or the next morning) after surgery when there is adequate haemostasis. Clopidogrel is a contraindication for patients receiving an epidural. BNF Class / Drug group (examples) Risk Use pre-op. when NBM Alternative post-op if unable to take po medication Management If stopping hold 48hrs pre-op and restart post-op. providing risk of bleeding no longer significant Check if on Asasantin retard (dipyridamole and aspirin combination)-if yes seek advice 2.12 Lipid-regulating drugs Statins Myopathy and rhabdomyolysis (numerous factors increase risk e.g. impaired renal function after major surgery, multiple drug use during anaesthesia) Niacin and fibric acid derivatives Myopathy and rhabdomyolysis (risk increases in combination with statins) Bile squestrants May interfere with absorption of medications required perioperatively Ezetimibe The risks (or benefits) of ezetimibe in the perioperative period are unknown Some manufacturers advise stopping a few days prior to major elective surgery and when any major medical or surgical condition supervenes. However, there is evidence that statins afford cardioprotection therefore continue but check CK post-op and monitor for signs of muscle toxicity Statins with a long half life/extended release formulations such as rosuvastatin, atorvastatin and fluvastatin bridge the period immediately after surgery when oral intake is not feasible. Check CK Stop evening before surgery i.v. available. Check levels pre-operatively. Theophylline level Continue Nebulised therapy if unable to use inhalers post-op NB: post op analgesia and post op pain may mask signs of myopathy. Discontinuation of niacin and fibric acid derivatives, bile sequestrants and ezetimibe is likely to be safe since these agents are given for the goal of long term reduction in vascular morbidity 3. RESPIRATORY Theophylline Inhaled bronchodilator therapy Narrow therapeutic range leading to increased risk of toxicity. Check for interacting drugs. 4. CNS Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 8 of 26 BNF Class / Drug group (examples) Risk 4.1 Benzodiazepines (e.g. diazepam, temazepam) 4.1 Hypnotics (e.g. Zopiclone, zolpidem) 4.2 Antipsychotics (e.g. haloperidol, clozapine, olanzapine) Tolerance Additive effects Withdrawal syndrome Additive effects Withdrawal syndrome Sedation Arrhythmias 4.2.3 Lithium Prolongs N/M blockade Toxicity 4.3.1 TCAs (e.g. amitriptyline, doselupin) 4.3.2 MAOIs -‘old type’, e.g. phenelzine - ‘new’ type, e.g. moclobemide Increase effect of exogenous catecholamines e.g. adrenaline resulting in arrhythmias, hypotension Hypertension, hyperthermia, convulsions, coma with opioids esp. pethidine, and sympathomimetics. Can be fatal. 4.3.3 SSRIs (e.g. citalopram, fluoxetine) Interactions may cause Serotonin syndrome (agitation, coma, tachycardia, hypertension, fever, myoclonus), eg pethidine, pentazocine, tramadol Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Use pre-op. when NBM Alternative post-op if unable to take po medication Management Continue i.v. and rectal forms if necessary. May need lower/higher doses for sedation Continue i.v. and rectal alternatives Continue (anti-emetic effect useful). Clozapine – recommended that it is withheld for 12 hours pre-op. After surgery patient receives his/her next dose at usual time. If withheld for more than 48 hours need to re-titrate. Not essential to stop, but requires close monitoring of fluids and electrolytes. If discontinued stop 24 hours before major operations restart with next post op dose. Check Lithium levels pre-op. i.v. alternatives available May need lower/higher doses for sedation U+E’s, FBC (clozapine) Continue. Avoid pro-arrhythmic anaesthetic agents. Use reduced doses of sympathomimetic agents. Avoid interacting drugs during anaesthesia. Discuss with anaesthetist. Otherwise need to stop old type 2 weeks before surgery. Newer reversible MAOIs are reversible after 24-48 hours. Psychiatric advice must be sought before stopping. Avoid use of interacting drugs, e.g. pethidine, dopamine, ephedrine, phenylephrine Continue- Fluoxetine has an extended halflive so can be omitted for 24-48 hours. Discontinuation of some SSRIs can precipitate withdrawal syndrome (especially paroxetine and venlafaxine), therefore withholding not advised. Extended half-lives so can be omitted for few days. Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 9 of 26 Haloperidol +/- lorazepam in some cases Check Lithium levels preassessment, monitor fluids and U+E’s. Avoid NSAIDs. Care with drug interactions Liquids available Caution when initiating interacting agents BNF Class / Drug group (examples) 4.3.4 Antidepressants, Other (e.g. mirtazapine, duloxetine) 4.4 Psychostimulants (methylphenidate) 4.5.1 Anti-obesity drugs acting on the GI tract (Orlistat) 4.7.2 Opioids Risk Use pre-op. when NBM Alternative post-op if unable to take po medication Management Continue Hypertension, arrhythmias, reduced seizure threshold Withhold on day of surgery Involuntary bowel movement during admission/ under anaesthesia Stop when NBM Hypotension, respiratory depression Continue, anaesthetist and pain team must be informed especially in patients on substance misuse program. Consult specialist psychiatrist Other routes available including topical, IV, Liquids, SL Consult pain team upon admission for management of acute on chronic pain Continue Phenytoin –liquid/ i.v. Phenobarbitone - i.v. Carbamazepine – rectal (125mg pr 100mg po) Sodium valproate - i.v. Care with converting to different forms with variying bioavailabilities. May need increased doses of induction agents and opiates. Phenytoin levels pre and post - op. -Continue L-dopa (sinemet/ madopar) as abrupt withdrawal can lead to neuroleptic malignant syndrome. -Dopamine agonists (pramipexole/ ropinerole) should be continued with -NG L-Dopa- can convert Sinemet/Madopar to Madopar Dispersible AntiemeticsDomperidone PR or NG before parkinsons meds, if required. Avoid Consider referral to pain team at preassessment for patients on buprenorphine as may need switching by primary care prior to admission. See also LINK 4.8. Anticonvulsants Induce hepatic enzymes(phenytoin, barbiturates, carbamazepine) Anaesthetics may depress hepatic drug elimination. Resistance to non-depolarising muscle relaxants. 4.9 Anti-parkinsonian drugs Neuroleptic malignant syndrome, Arrhythmias, Hypertension (L-dopa) Symptoms exacerbated by some antiemetics. Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 10 of 26 BNF Class / Drug group (examples) Risk Selegiline/ rasagiline + pethidine can cause hyperpyrexia and CNS toxicity 4.10 Alcohol & nicotine e.g. acamprosate, disulfiram, varenicline Abrupt withdrawal of varenicline leads to risk of relapse, depression, insomnia Use pre-op. when NBM Alternative post-op if unable to take po medication agreement of anaesthetist, or converted by Movement disorder team to a rotigotine patch. Rotigotine Patch should be continued. - Entacapone/ tolcapone/ selegiline/ rasagiline/ zelapar/ amantadine may be safely omitted until able to swallow. If selegeline to continue, use ‘safe anaesthetic technique’. If stopped may need to increase L-dopa dose. -Apomorphine available but needs specialist supervision and advice for use. -Rotigotine patches also available – seek specialist advice. -If NBM prolonged discuss with Specialist Parkinson’s team-See Appendix 3: ‘Acute Management of Parkinson’s disease patients with compromised swallow or nil by mouth’ for detailed conversions and information. Continue, avoid medication that contains alcohol as may precipitate reaction with disulfiram Continue drugs for smoking cessation 4.11 Drugs for dementia, (e.g. donepezil, rivastigmine, galantamine) Increased muscle relaxation produced by suxamethonium resulting in prolonged neuromuscular blockade Continue but inform anaesthetist If suxamethonium to be used, donepezil advised to be stopped 2-3/52 pre-op but can lead to deterioration in mental function which will not recover. Therefore best to avoid suxamethonium and withhold max. 24 hrs pre-op. Rivastigmine + galantamine can be withheld max. 24 hrs pre-op 5. ANTIBIOTICS, ANTIVIRALS & ANTIFUNGALS 5.1 / 5.2 Antibiotics & antifungals 5.3 Antivirals used for HIV Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Consult Microbiology Continue Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 11 of 26 Restart immediately post-op otherwise may lead to decline in patient’s mental function Management metoclopramide and prochlorperazine Discuss with Specialist Parkinson’s team BNF Class / Drug group (examples) Risk Use pre-op. when NBM Alternative post-op if unable to take po medication Management depends on usual insulin regime. Consult Diabetes Specialist Team for specific advice. Continue taking as normal prior to admission. Once NBM then omit dose (pioglitazone may be continued). Recommence once normal eating resumed. If patient anticipated to have long starvation period (i.e. 2 or more missed meals), switch to VRII to achieve and maintain normoglycaemia. Long-acting insulin may be continued. Contact Diabetes team for further advice.www.diabetes.nhs.uk/our_work_are Management 6. ENDOCRINE 6.1.1 Insulin Increased risk of post-op infection. Altered requirements 6.1 Oral hypoglycaemics (e.g. gliclazide, rosiglitazone, metformin, repaglinide, sitagliptin, exenetide) Peri-operative hypoglycaemia Lactic acidosis (metformin) 6.2.1 Levothyroxine Impaired stress reaction if hypothyroid 6.2.2 Anti-thyroid drugs (e.g. carbimazole) 6.3 Corticosteroids i.e. long-term steroids at doses >5mg/day prednisolone (or equivalent) or received same within last 3 months. Also high dose inhaled steroids (eg beclometasone doses over 1mg or equivalent. 6.4 Hormone replacement therapy + SERMS(Raloxifene) Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number www.diabetes.nhs.uk/our_work_areas/inpatient_care/ as/inpatient_care/ Continue. May discontinue therapy for several days due to long half-life. If NBM prolonged, convert to liothyronine (levothyroxine 100micrograms liothyronine inj 20micrograms) TFTs to ensure dose adequate. Increase dose to cover surgery. Dose depends on usual steroid dose, duration and indication Minor surgery 25mg iv hydrocortisone Moderate surgery 25mg iv hydrocortisone at induction then 6hrly for 24hrs Major surgery 25mg iv hydrocortisone at induction then 6hrly for 48 to 72hrs Restart after discharge as for COC. Ensure adequate thrombo-prophylaxis prescribed Continue Hypotension Impaired stress reaction Delayed wound healing Altered immune function Risk of bleeding with NSAIDs. Continue usual dose on morning of surgery. Additional steroid cover, duration and type of surgery will determine risk, discuss with consultant. Doses equivalent to >5mg prednisolone daily cause HPA axis suppression and will require glucocorticoid coverage. Slight increased risk of DVT/PE but risks not established (see OCP/HRT protocol – appendix 2) Can be continued safely if benefits outweigh risks. If to discontinue then need to stop 4 weeks prior to surgery. Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 12 of 26 BNF Class / Drug group (examples) 6.4.1.2 High dose progestogens ( eg used for menstrual disorders) 6.6.2 Bisphosphonates (alendronic acid, risedronate) Risk Use pre-op. when NBM Alternative post-op if unable to take po medication Increased risk of DVT/PE in major surgery Discontinue 4 weeks prior to major surgery. Oesophageal irritation Omit on morning of surgery, If due on morning of surgery advise patient to take day before. Restart with first menses that occur at least 2 weeks after discharge providing patient fully mobile Recommence when patient is able to sit upright and is drinking free fluids. Management 7. OBSTETRICS, GYNAECEOLOGY AND URINARY-TRACT DISORDERS 7.3 Combined oral contraceptive (COC) (oestrogen containing) VTE and Hormonal Contraception RCOG guideline 2010 7.3 Progestogen only contraceptives (includes injectables, IUD & implants) 7.4.2 Drugs for urinary frequency (oxybutynin, solifenacin) 7.4.5 Drugs for erectile dysfunction (sildenafil, tadenafil) Increased risk of DVT/PE in major surgery or following any other surgery which involves prolonged periods of immobility (see OCP/HRT protocol- appendix 2) No added risk of thrombo-embolic risk (see OCP/HRT protocol appendix 2) Discontinue 4 weeks prior to major surgery where immobilisation is expected and all lower limb surgery. Restart with first menses that occur at least 2 weeks after discharge providing patient is fully mobilised However, consider risks of unplanned pregnancy. Progestogen-only pill is suitable alternative. Continue Continue Mild transient hypotension due to vasodilator properties Discontinue 24 hour before surgery except for pulmonary hypertension. Ensure anaesthetist aware 8./ 9. MALIGNANT DISEASE / BLOOD 8.1 Antineoplastic drugs 8.3.4 Tamoxifen Discuss with specialist Increased risk of DVT/PE in major surgery Anovulatory infertility– discontinue 4-6 weeks prior to major surgery. Women with history of breast cancer – continue Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 13 of 26 If discontinued, restart at least 4 weeks post-operatively providing patient fully mobile If decision is to continue ensure adequate thromboprophylaxis BNF Class / Drug group (examples) Risk 9.1 Iron Use pre-op. when NBM Alternative post-op if unable to take po medication Management Continue except for colonoscopy- stop 7 days pre-op 10. MUSCULO-SKELETAL / JOINT DISEASE 10.1.1 NSAIDS GI haemorrhage Impaired wound healing Renal impairment 10.1.3 DMARDS and immunosuppressants Impaired wound healing Renal impairment If haemorrhage likely to be a risk then stop: - short-acting drugs e.g diclofenac , ibuprofen, stop 1 day pre-op - long-acting e.g. piroxicam stop 3 days pre-op - COX 2 inhibitors e.g. celecoxib, etoricoxib, discontinue morning of op Some some evidence that use of Ibuprofen pre-op reduces pain post-op. Benefit verses risk to be considered by specialist in each case Methotrexate Elderly/frail/co-morbidities/RI : stop ONE week pre-op. Can continue in otherwise healthy individuals. pr preps available U+E’s Restart as soon as possible once wound healed and providing renal function stable. U+E’s. Caution with NSAIDs. Sulfasalazine / Azathioprine Withold day of surgery Hydroxochloroquine / Lefluonimide Continue as normal 10.1.3 Cytokine inhibitors e.g Adalimumab, Inflixamab, Anakinra, Etanercept Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Increase risk of infection Impaired wound healing NB: if using for any other condition, e.g. haematological or post-transplantation, then the advice of the relevant specialist must be obtained Withold prior to major surgical procedures. Risk/ benefits must be discussed with specialist. Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 14 of 26 Treatment may be restarted once wound healing is satisfactory and no sign of infection. BNF Class / Drug group (examples) Risk Use pre-op. when NBM Alternative post-op if unable to take po medication General guidance stop 3-5 x half life (T1/2): Adalimumab stop at 45 days Etanercept stop 9 days Infliximab stop 24 days 10.2 Neuromuscular Disordersanticholinesterases e.g. neostigmine, pyridostigmine Respiratory complications, cholinergic crisis Discuss with anaesthetist- manage according to severity of disease and type of surgery 11. TOPICAL EYE PREPS Steroids, pilocarpine, beta-blockers (timolol) Bradycardia due to systemic absorption (beta- blockers) Continue Flu like symptoms Advise patients to avoid having vaccination within 7 days pre-op 14 VACCINES Flu vaccine Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 15 of 26 IV pyridostigmine available. Dose adjustment required Management References Actavis Pharma. Bisphosphonates prior to surgery. Personal communication accessed 27th July 2012 Ang-Lee MK, Moss J, Yuan CS. Herbal medicines and perioperative care. JAMA 2001; 286(2): 208-216 Anon. Drugs in the peri-operative period: 2 – Corticosteroids and therapy for diabetes mellitus. Drug Therapeutic Bull 1999; 37: 68-70 Anon. Drugs in the peri-operative period: 3 – Hormonal contraceptives and hormone replacement therapy. Drug Therapeutic Bull 1999; 37: 78-80 Anon. Drugs in the peri-operative period: 4 – Cardiovascular drugs. Drug Therapeutic Bull 1999; 37: 89-92 Anon. Drugs in the peri-operative period: Stopping or continuing drugs around surgery. Drug Therapeutic Bull 1999; 37: 2-74 Anon. Surgery and long-term medication. Drug Therapeutic Bull 1984 ; 22(19) : 73-76 Anon. Surgery patients at risk for herb-anaesthesia interactions. Lancet 1999 ; 354 :1362 Anon. Use of herbal medicines could pose risk to patients undergoing surgery. Pharm J 2001; 267: 79 Auerbach AD, Goldman L. Beta-blockers and reduction of cardiac events in noncardiac surgery: scientific review. JAMA 2002 ; 287 (11) : 1435-1444. Burger W, Chemnitimus JM, Kneissl GD, Rucker G. Low dose aspirin for secondary prevention – cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation- review and meta-analysis. Journal of internal Medicine 2005 ;257: 399-414 Cardone, A et al. Perioperative evaluation of Myesthenia Gravis. Ann. Ital. Chir. 2007; 78: 359-365 Carpenter MT, West SG, Vogelgesang SA, Casey Jones DE. Postoperative joint infections in rheumatoid arthritis patients on methotrexate therapy. Orthopedics 1996; 19(3):207-10 Castanheira L, Fresco P, Macedo AF. Guidelines for the management of chronic medication in the perioperative period: systematic review and formal consensus. Journal of Clinical Pharmacy and Therapeutics (2011) 36, 446–467 Chakravarty K,McDonald H, Pullar T et al. BSR/BHPR guideline for disease modifying anti-rheumatic drug (DMARD) terapy in consultation with the British Association of Dermatologists 2008. www.rheumatology.org.uk/resources/guidelines (last accessed April 2013) Ding T, Leckingham J, Luqmaru R et al. BSR and BHPR rheumatoid arthritis guidelines on safety of anti-TNF therapies 2010. www.rheumatology.org.uk/resources/guidelines (last accessed April 2013) Douketis JD, Berger PB, Dunn AS, et al. The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence Based Clinical Practice Guidelines (8th Edition). Chest 2008;133:299S Duthie DJR, Montgomery JN, Spence AA, Nimmo WS. Concurrent drug therapy in patients undergoing surgery. Anaesthesia 1987 ; 42 : 305-306 European Society of Cardiology (ESC) guidelines for pre-operative cardiac risk assessment and peri-operative cardiac management in non-cardiac surgery. European Heart Journal (2009) 30, 2769-2812. Fleisher LA, Beckman JA, Brown KA. ACC/AHA 2007 Guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery. Circulation 2007; 116; 418-499 Fugh-Berman A. Herb-drug interactions. Lancet 2000 ; 355 :134-138 Kennedy JM, van Rij AM, Spears GF, Pettigrew RA, Tucker IG. Polypharmacy in a general surgical unit and consequences of drug withdrawal. Br J Clin Pharmacol 2000; 49(4): 353-62 Goh L, Jewell T, Laversuch C, Samant A. Should anti-TNF therapy be discontinued in rheumatoid arthritis patients undergoing elective orthopaedic surgery? A systematic review of the evidence. Rheumatol Int 2012; 32 (1):5-13. Merli, GJ, Bell, RD. Perioperative care of the surgical patient with neurologic disease. www.uptodate.com 2012 Miller J, Warren A. Nil-by-mouth needs defining. Hosp Pharm Prac 1994 ; 4(2) :53-54 Muluk V, Macpherson DS. Perioperative Medication Management. www.uptodate.com 2012 Mushtaq S, Goodman S, Scanzello C. Peri-operative management of Biologic Agents used in the treatment of Rheumatoid Arthritis. American Journal of Therapeutics 2011; 18(5):426-434 NHS Diabetes. Management of Adults with Diabetes undergoing surgery and elective procedures: improving standards. April 2011 www.diabetes.nhs.uk/our_work_areas/inpatient_care/ Nielsen JD, Holm-Nielsen A, Jespersen J, Vinther CC, Settgast IW, Gram J. The effect of low-dose acetylsalicylic acid on bleeding after transurethral prostatectomy- a prospective, randomized, double-blind, placebo-controlled study. Scand J Urol Nephrol 2000; 34(3):194-198 RCN Rheumatology Biologics Working Party. Assessing, managing and monitoring biologic therapies for inflammatory arthritis. Guidance for Rheumatology practitioners 2nd edition 2009. Rispler DT, Sara J. The impact of complementary and alternative treatment modalities on the care of orthopaedic patients. J Am Acad Orthop Surg 2011; 19(10):634-643 Rosenman DJ, McDonald FS, Ebbert JO, et al. Clinical consequence of withholding versus administering renin-angiotensinaldosterone system antagonists in the preoperative period. J Hosp Med 2008; 3:319 Royal College of Obstetricians and Gynaecologists Guideline No 40 Venous Thromboembolism and Hormonal Contraception.July 2010 Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Page 16 of 26 Salem M, Tainish RE, Bromberg J, Loriaux DL, Chernow B. Perioperative glucocorticoid coverage. A reassessment 42 years after emergence of a problem. Ann Surg 1994; 219 : 416-425 Schouten O, Hoeks SE, Gijs MJM et al. Effect of statin withdrawal on frequency of cardiac events after vascular surgery. American Journal of Cardiology 2007; 100(2): 316-320 Scottish Intercollegiate Guideline Network (SIGN) Guidelines. Prophylaxis of Venous Thromboembolism. Guideline 62, October 2002. Sear JW, Higham H. Issues in the perioperative manangement of the elderly patient with cardiovascular disease. Drugs and Ageing 2002; 19(6) : 429-451 Shammash JB, Trost JC, Gold JM, et al. Perioperativebeta-blocker withdrawal and mortality in vascular surgical patients. Am Heart J 2001;141:148 SPC Dabigatran. Accessed Oct 2012. SPC Rivaroxaban. Accessed Oct 2012 Stafford Smith M, Muir H, Hall R. Perioperative management of drug therapy : clinical considerations. Drugs 1996; 51(2) : 238259 Steuer A, Keat AC. Perioperative use of methotrexate- a survey of clinical practice in UK. Br J Rheum 1997; 36: 1009-1011 Straube S, Derry S, McQuay H and Moore R :Effect of pre-operative Cox 2 Selective NSAIDS (Coxibs) on post-operative outcomes: A systematic review of Randomized studies. Acta Anaestesiol Scand 2005:49:601-613 Thromboembolic Risk Factors (THRIFT) Consensus Group. Risk of prophylaxis for venous thromboembolism in hospital patients. BMJ 1992 ; 305 :567-574 Wijeysundera DN, BeattieWS. Calcium channel blockersfor reducing cardiac morbidity after non cardiac surgery: a metaanalysis. Anesth Analg 2003; 97:634 Wysokinski WE, McBane RD. Periprocedural Bridging Mangement of Anticoagulation. Circulation 2012;126: 486-90. The following guidelines were consulted: Royal Cornwall Hospitals NHS Trust. Pre-Operative Assessment Guidelines. November 2010 Whittington Hospital NHS Trust. Nil by mouth perioperative medicine use guideline. January 2012. Worcestershire Acute Hospitals NHS Trust. Nil by mouth and peri-operative medicines use guideline. Accessed on 12.09.12 This policy refers to the following CDDFT policies and procedures: County Durham and Darlington Foundation NHS Trust. Oral Anticoagulation with warfarin- adult patient management guidelines. January 2013. County Durham and Darlington Foundation NHS Trust. http://intranet/sites/policiesandprocedures/Published%20Documents/Oral%20anticoagulation%20with%20warfarin%20%20adult%20patient%20management%20guidelines.pdf County Durham and Darlington Foundation NHS Trust. Anticoagulation guidelines for Neuraxial procedures (2010) http://intranet/Directorates/CCG/SD/Anaes/Joint%20Dept%20Guidelines/Regional/Anticoagulation%20and%20Neuraxial%20CDDFT.pdf Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 17 of 26 Appendix 1: Herbal and homeopathic medicines The use of herbal and homeopathic medications in the UK is becoming increasingly popular. It is vital that these medications are listed during the medicines reconciliation process as many may interfere with or have an effect on surgical procedures. The following list is intended as a guide only, however it is advised that ALL herbal/ homeopathic medicines be stopped TWO WEEKS prior to elective surgery Medication Risk 5-HTP Agnus Castus Has serotinergic properties; treat as an SSRI. Caution with pethidine use. Pro-oestrogenic; could increase thrombus risk. Dopamine agonist; Treat as haloperidol clozapine or sulpiride Clinical evidence of hypotensive effects. Clinical research suggests hypoglycaemic effects Immunomodulating properties; Possible increased risk of infection and poor wound healing. Prooestrogenic; could increase thrombus risk. Clinical research suggests hypoglycaemic effects Clinical research suggests hypoglycaemic effects Clinical research suggests hypoglycaemic effects Preliminary evidence of hypotensive effects Pro-oestrogenic; could increase thrombus risk. Sympathomimetic; can cause hypertension, tachycardia and arrhythmias Anticholinesterase action; bradycardia, hypotension, bronchoconstriction. Clinical evidence of hypotensive effects Clinical evidence of hypotensive effects Clinical research suggests hypoglycaemic effects Mineralocorticoid effect; could increase blood pressure Antiplatelet effect; increases bleeding risk Clinical research suggests hypoglycaemic effects Stimulant. Structurally related to phenylephrine, it can predispose the patient to stroke, myocardial infarction, arrhythmia from tachycardia and hypertension. May interact with MAOIs. Omit a minimum of 24hours pre-op. Pro-oestrogenic; could increase thrombus risk Large quantities of caffeine in black tea can have antiplatelet effects; increased bleeding risk Agrimony Alfalfa Aloes/Aloe vera Alpha-lipoic acid Andrographis Aniseed Arnica Asafoetida Avens Banaba Bayberry Bilberry Bitter melon Bitter orange Black Cohosh Black tea (concentrated tablets) Blue Cohosh Boldo Boneset Broom Burdock Butterbur Calamus Calendula Capsicum Cat's Claw Celery Centaury Chamomile Chondroitin Clove Coenzyme Q10 Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Theoretical hypertensive effects Anticoagulation effect; increased risk of bleeding. Can potentiate the effects of warfarin. Immunomodulating properties; Possible increased risk of infection and poor wound healing Hypertensive; potential to raise blood pressure Potential cardiac depressant activity Clinical research suggests hypoglycaemic effects Clinical evidence of hypotensive effects Clinical evidence of hypotensive effects. Theoretical catecholamine activity. Potentiates barbiturate sleeping time Immunomodulating properties; Possible increased risk of infection and poor wound healing Sympathomimetic; can cause hypertension, tachycardia and arrhythmias Antiplatelet effect; increases bleeding risk. Clinical evidence of hypotensive effects Immunomodulating properties; Possible increased risk of infection and poor wound healing Clinical research suggests hypoglycaemic effects Sedatives effect Sedative effect Immunomodulating properties; Possible increased risk of infection and poor wound healing. Mild sedative effects; could potentiate anaesthetics Anticoagulation effect; increased risk of bleeding. Can potentiate the effects of warfarin. Chondroitin also affects blood sugar control Antiplatelet effect; increases bleeding risk Clinical research suggesting modest hypotensive effects Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 18 of 26 Cola nut Coltsfoot Corn Silk Couchgrass Cowslip Damiana Dandelion Danshen Devil's Claw Dong quai Drosera Echinacea Elecampane Ephedra Epimedium Eucalyptus Fenugreek Feverfew Fucus Fumitory Garlic Ginger Ginkgo Ginseng (American, Eleutherococcus and Panax) Glucomannan Glucosamine Golden Seal Greater Celandine Green tea (concentrated) Guarana Gymnema Hawthorn Hops Horehound Horse chestnut Horseradish Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Stimulant. Increased risk of tachycardia and hypertension. Vasopressor activity causes hypertension Clinical evidence of hypotensive effects. Clinical research suggests hypoglycaemic effects Sedative effect Initially causes hypotension, then later hypertension Clinical research suggests hypoglycaemic effects Clinical research suggests hypoglycaemic effects Anticoagulation effect; increased risk of bleeding. Can potentiate the effects of warfarin Clinical research suggests hypoglycaemic effects. Clinical evidence of hypotensive effects Anticoagulation effect; increased risk of bleeding. Can potentiate the effects of warfarin Immunomodulating properties; Possible increased risk of infection and poor wound healing Possible increased risk of infection and poor wound healing Clinical research suggests hypoglycaemic effects. Sedative effect. Clinical evidence of hypotensive effects Stimulant: Is a source of ephedrine, pseudoephedrine, and phenylpropanolamine. Can cause tachycardia and hypertension with spontaneous adverse events including stroke, myocardial infarction,QT interval prolongation and arrhythmia. Also known to inhibit complement pathway Preliminary evidence of hypotensive effects Clinical research suggests hypoglycaemic effects Anticholinesterase action; bradycardia, hypotension, bronchoconstriction. Anticoagulation effect; increased risk of bleeding. Can potentiate the effects of warfarin. Clinical research suggests hypoglycaemic effects Antiplatelet effect; increases bleeding risk Anticoagulation effect; increased risk of bleeding. Potential hypotensive effects, Both hyper- and hypothyroidism reported with continued use Clinical evidence of hypotensive effects Antiplatelet effect; increases bleeding risk. Also have hypotensive properties. Clinical research suggests hypoglycaemic effects Antiplatelet effect; increases bleeding risk. Clinical research suggests hypoglycaemic effects. Also has hypotensive properties Pro-oestrogenic; could increase thrombus risk. MAOI activity. Antiplatelet effect; increases bleeding risk Immunomodulating properties; Possible increased risk of infection and poor wound healing. Has erratic blood glucose control in patients reporting both hyper- and hypoglycaemic control CNS depressant and stimulant Pro-oestrogenic; could increase thrombus risk Antiplatelet effects; increases bleeding risk Also has erratic blood pressure altering properties, causing both hyper- and hypo-tension in patients. MAOI potentiation, suspected phenelzine interaction Clinical research suggesting hypoglycaemic effects Anticoagulation effect; increased risk of bleeding. Can potentiate the effects of warfarin and can also affect blood sugar control Potential hypotensive effects, Heparin antagonist, Sedative effect Immunomodulating properties; Possible increased risk of infection and poor wound healing Large quantities of caffeine in green tea can have antiplatelet effects; increased bleeding risk.It can also be a stimulant in large quantities. Antiplatelet effects; increases bleeding risk. Also a known stimulant; increases risk of tachycardia, hypertension and arrhythmias. Clinical research suggests hypoglycaemic effects Clinical evidence of hypotensive effects.CNS depressant; potentiates barbiturate sleeping time Mild sedative effects ( usually used in combination with other sedative products). Could potentiate anaesthetics. White Vasodilator properties; lowers blood pressure Active constituents thought to have antiplatelet activity; increases bleeding risk.Clinical evidence of hypotensive effects Clinical evidence of hypotensive effects. Peroxidase stimulates synthesis of arachidonic acid metabolites Both hyper- and hypo thyroidism reported with continued use Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 19 of 26 Hydrocotyl Jamaica Java Tea Juniper Kava L-arginine Lavender Lemon balm Liquorice L-tryptophan Marshmallow Maté Melatonin Mistletoe Motherwort Myrrh Nettle Parsley Passionflower Plantain Pleurisy Root Pokeroot Policosanol Prickly Ash Prickly pear cactus Red Clover Resveratrol Rosemary Sage SAMe Saw Palmetto Scullcap Senega Shepherd's Purse Squill Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Hyperglycaemic effect and Sedative effect Dogwood Sedative effect Clinical evidence of hypotensive effects. Clinical research suggests hypoglycaemic effects Clinical evidence of hypotensive effects. Clinical research suggests hypoglycaemic effects Additive effects with benzodiazepines increasing sedation; also linked to numerous reports of hepatotoxicity Possible dopamine antagonist effects. Treat as haloperidol clozapine or sulpiride. Clinical research suggesting modest hypotensive effects Mild sedative effects; additive effects with CNS depressants and anaesthetics. Clinical research suggesting sedative effects. Could potentiate anaesthetics Mineralocorticoid effect; could increase blood pressure. Pro-oestrogenic; could increase thrombus risk, Antiplatelet effect; increases bleeding risk. Also has a laxative effect similar to senna. Particularly important to withdraw prior to bowel surgery. Clinical research showing sedative effects; documented reports of additive effects with CNS depressants and anaesthetics. Also has serotinergic properties; treat as an SSRI. Caution with pethidine. Clinical research suggests hypoglycaemic effects Stimulant. Increased risk of tachycardia and hypertension Clinical research suggesting sedative effects; can potentiate anaesthetics. Seek anaesthetic advice if prescribed by a clinician (especially in children). Clinical evidence of hypotensive effects. Promotes coagulation and has Immunomodulating properties; Possible increased risk of infection and poor wound healing Oxytocic properties Clinical research suggests hypoglycaemic effects Clinical evidence of hypotensive effects. CNS depression, in vivo. Clinical research suggests hypoglycaemic effects, Anticholinesterase action; bradycardia, hypotension, bronchoconstriction. Sympathomimetic; can cause hypertension, tachycardia and arrhythmias Mild sedative effects; animal models suggest additive effects with CNS depressants Clinical evidence of hypotensive effects Sympathomimetic; can cause hypertension, tachycardia and arrhythmias. Pro-oestrogenic; could increase thrombus risk Clinical evidence of hypotensive effects Possible antiplatelet effect (based on anecdotal evidence). May increase bleeding risk Clinical evidence of hypotensive effects Clinical research suggesting hypoglycaemic effects Pro-oestrogenic; could increase thrombus risk Possible antiplatelet effect (based on in vitro data). May increase bleeding risk Hyperglycaemic effect Potential hypotensive effects Sedative effect. Clinical research suggests hypoglycaemic effects Has serotinergic properties; treat as an SSRI. Caution with pethidine use. Immuno -modulating properties; Possible increased risk of infection and poor wound healing. Both oestrogenic and anti-androgenic properties. Possible antiplatelet effect (based on anecdotal evidence). May increase bleeding risk Reputed action CNS depressant, Clinical research suggests hypoglycaemic effects Potentiates barbiturate sleeping time. Anticholinesterase action; bradycardia, hypotension, bronchoconstriction Clinical evidence of hypotensive effects Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 20 of 26 Appendix 2 : Guidelines on the use of Oral Contraceptives and Hormone Replacement Therapy in the Peri-operative Period Progesterone-only Preparations There is no evidence of increased risk of venous thromboembolism in the peri-operative period and these preparations should not be stopped. Combined Oral Contraceptives (COC) Minor surgery (excluding leg surgery) Women should continue taking the COC. Major Surgery or Leg Surgery There is known to be a small absolute risk of post-operative venous thromboembolism in COC users (estimated to be 0.96% for users compared with 0.5% for non-users). Whenever possible the surgeon should discuss the possible risk with the patient at least six weeks before elective surgery. The risk of thromboembolism should be balanced against the possibility of unwanted pregnancy if the pill were to be stopped without adequate alternative contraception If the patient states that she wishes to continue the COC, she should then receive the recommended thromboprophylaxis. If the patient does want to stop the COC, she should do so at least four weeks before surgery. There is no proven benefit in stopping nearer to surgery. The patient should be referred back to her GP or Family Planning Clinic to arrange alternative contraception. Whichever peri-operative approach is chosen, a careful record should be made in the case notes that potential advantages and disadvantages have been discussed with the woman. In any cases (trauma or elective) where the patient is admitted still taking the COC, it should be prescribed on the drug chart and NOT be discontinued. The patient should then receive the recommended thromboprophylaxis. Hormone Replacement Therapy (HRT) Taking HRT is likely to increase the risk of post-operative thromboembolism, but this additional risk has not been well quantified. In general, there appears to be no need to advise patients to discontinue HRT before surgery if there are no predisposing factors for thromboembolism , e.g. personal or family history of DVT or PE, severe varicose veins, obesity or prolonged bed-rest. If there are predisposing risk factors, it may be prudent to review the need for HRT as the risks may exceed the benefits. Any patient wishing to stop, should do so at least four weeks before surgery and be referred back to her GP. The possible increased risk should be explained to the patient and the decision documented. Patients continuing with HRT should have their medication prescribed on the drug chart and receive the recommended thromboprophylaxis. Such prophylaxis is unnecessary with minor surgery. In any cases (trauma or elective) where the patient is admitted still taking HRT, it should be prescribed on the drug chart and NOT be discontinued. The patient should then receive the recommended thromboprophylaxis. Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 21 of 26 Appendix 3 : Acute management of Parkinson’s Disease patients with compromised swallow or nil by mouth RISK OF DEATH IF MEDICATION IS OMITTED If timely Parkinson’s medication is not given this can lead to patients being unable to swallow (risk of aspiration), unable to speak, unable to move, increased risk of falls, increased care needs, pain and distress. At the worst it could develop into neuroleptic malignant syndrome, Parkinson’s Hyperpyrexia, Dopamine Agonist Withdrawl syndrome or even death. Introduction Parkinson’s disease is a progressive disabling neurological disorder, resulting from the degeneration of dopamine producing neurones in the substantia nigra. The cardinal signs being 1) Bradykinesia - slowness of movement 2) Rigidity - increased muscle tone, may be asymmetrical or limited to certain muscle groups 3) Tremor – 30% of patients have no evidence of tremor Parkinson’s disease is predominantly a movement disorder, but which also is associated with many other non-motor function such as anxiety disorders, depression, excessive daytime sleepiness, dementia, apathy etc. This document is a guide for those patients that are admitted to hospital and are either nil by mouth or unable to swallow. It can be used in the first 48 hours; however advice should be taken from the patient’s own specialist (Dr or Parkinsons Disease Nurse Specialist) as soon as possible. On presentation to services 1. Check drug history – the following sources can be used: Family/ carer Medication brought in Consultant or Movement Disorder Nurse Specialist team letter in notes Residential/nursing home GP Community pharmacist Community nurse 2. Doses must be checked carefully. 3. Timings of medication ARE VERY IMPORTANT - Regimes are individual, it is therefore essential to give at patient’s times not ward drug round times. 4. Obtain medication ASAP. This is classed as a critical medication and must be ordered as such. a. Acute areas/wards hold a standard stock of commonly used Parkinson’s medications; these include AMU and emergency drug cupboard. Also Ward 52 Rachel could you investigate b. Patient’s own supply of medication. Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 22 of 26 5. DO NOT STOP PARKINSON’S MEDICATION! 6. If on Duodopa, Apomorphine or Rotigotine patch, continue as prescribed. 1. Unable to swallow (includes nil by mouth) For patients who are unable to swallow or are nil by mouth, see appropriate section below: Consider: 1) Speech and language therapist (S.A.L.T.) - a.s.a.p 2) Nasogastric tube - (consent) 2. Advice regarding Levodopa products There is no conversion from Levodopa to a Dopamine Agonist. As a minimum a 2mg Rotigotine patch should be used if no NG tube in place. A review should then be done by the Specialist team as soon as possible. Medication which may be given via N.G tube as follows: Brand Name Sinemet Generic Name Co-careldopa Alternative Madopar Dispersible Madopar Co-beneldopa Madopar Dispersible Stalevo Levodopa/carbidopa/entacapone Madopar Dispersible Dose Convert ‘like to like’ as a minimum 3. Antiemetics Use Domperidone; this should be by suppository 30 mg bd or liquid 10 - 20mg tds via N.G. tube given prior to Parkinsons medication. This should be used for short term only, following MHRA recommendations. An alternative would be Cyclizine or Ondansetron. 4. Medication which may be safely omitted until able to swallow C.O.M.T. Inhibitors - Entacapone / Tolcapone M.A.O.B. Inhibitors - Selegiline/ Rasagiline / Zelapar Amantadine (Symmetrel) 5. Dopamine Agonist advice Brand Name Advice Rotigotine patch Continue Apomorphine s/c Continue. Use familiar pump if unsure of Apo-go pump. DO NOT STOP!! (injection or infusion) (24hr helpline: 08448801327) contact Movement Disorder Nurse team Pramipexole Maintain same dose, crush tablets ** Pramipexole PR Convert to standard dose Pramipexole TDS and crush as above (slow release) Ropinirole Maintain same dose, crush tablets ** Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 23 of 26 Ropinirole XL (slow release) Pergolide Cabergoline Bromocriptine Convert to standard dose Ropinirole TDS and crush as above Maintain same dose, crush tablets ** Maintain same dose, crush tablets ** Maintain same dose, crush tablets ** ** Unlicensed use. Crushing of tablets should only be considered for short term use, i.e. first 48 hours of admission until the patient can be reviewed by a specialist, for prolonged use or if crushing tablets blocks the N.G. tube see alternatives in this pathway. 6. Switch guidelines Only to be used under instruction from Movement Disorder Team. 01325743000 Suggested conversions for oral dopamine agonist doses to equivalent patch treatment Pramipexole* 88 mcgs BASE tds (125 mcgs SALT tds) Pramipexole PR* (slow release) 260 mcgs BASE od (375 mcgs SALT od) 180 mcgs BASE tds (250mcgs SALT tds) 350 mcgs BASE tds (500 mcgs SALT tds) 530 mcgs BASE tds (750 mcgs SALT tds) 700 mcgs BASE tds (1mg tds) 880mcg BASE tds (1.25mg SALT tds) 520 mcgs BASE od (750miCS SALT od) 1.05mg BASE od (1.5mg SALT od) 1.57mg BASE od (2.25mg SALT od) 2.1 mg BASE od (3mg SALT od) 2.62mg BASE od (3.75mg SALT od) Ropinirole Ropinirole XL (slow release) Rotigotine Patch Starter pack 2mg /24 hrs 1mg tds 4mg od 4mg/24 hrs 2mg tds 6mg od 6mg/24 hrs 3mg tds 8mg od 4mg tds 12mg od 8mg/24 hrs 10-12mg /24 hrs 14mg/24 hrs 6mg tds 16mg od *Pramipexole doses are expressed as base (salt). Less frequently used dopamine agonists. Now very rarely used but patient’s may still be admitted on these drugs. Contact Movement Disorder team as above for advice. Cabergoline Pergolide Change to Rotigotine Patch 0.5 mg od 125microgram tds 2mg od 1mg od 250microgram tds 4mg od 2mg od 500microgram tds 6mg od 3mg od 750microgram tds 8mg od 7. Apomorphine Apomorphine is a potent D1 and D2 dopamine agonist. It can only be administered by intermittent subcutaneous injections, or continuous subcutaneous infusion. Patient already on apomorphine: Continue on same dose, use alternative pump if necessary Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 24 of 26 Patient, Carer or family are well trained in the use of an APO-GO pump and are a good resource, if Movement disorder team are unavailable. (24hr helpline: 08448801327) or contact Movement Disorder Nurse Specialist Patient not already on apomorphine: Do not start without discussion with specialist consultant. It is important to give Domperidone 30mg suppository bd (minimum 24 hours prior to administering Apomorphine) and then continue, to avoid vomiting. If patient on levodopa 400 mg daily or above or Duodopa has been discontinued then commence Apomorphine 2mgs/hr over 12 hours (daytime). If on an oral Dopamine Agonist and Levodopa, and have symptoms of rigidity and/or tremor severe may need to consider increasing Apomorphine within first 12 hours to 3 mgs per hour over 12 hours (daytime). For patients with overnight symptoms, bolus doses may be given as per the current daytime rate via subcutaneous pen injector. Always monitor Blood pressure regularly- clinical decision. Change infusion line every 12 hours. Massage site prior insertion of needle and after removal. Use a different insertion/injection site each time (see information pack). Duodopa -continue as prescribed. For advice contact 24 hour helpline on 0800-458 4410 Movement Disorder Nurse Specialist team contact details: Alison Rose: 01325743000, Mobile 07980729862, Louise Cochrane: 01325743000, Mobile 07980726532, Liz Taylor: 01325743000, Mobile 07967202353 References: British National Formulary No: 62, 2011 Summary of Product Characteristics for individual products: www.medicines.org.uk This document has been adapted by Alison Rose, Movement Disorder Nurse Specialist, in June 2012. Acknowledgements Many thanks to the below: This document was originally produced by North West Parkinson’s Disease Nurse Specialist’s in collaboration with pharmacists with a specialist interest in P.D. It was then adapted for use by Sue Lord, Pharmacist, for Betsi Cadwaldr University Health Board. Date of production March 2011. Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 25 of 26 Appendix 4 : Summary of drugs requiring withdrawal prior to major surgery This sheet is intended as a summary of the guidelines for the management of drug therapy in the perioperative period. They relate to MAJOR surgery only. For further guidance please refer to the full guidance or contact Pharmacy. 4-6 weeks pre-op 2 weeks pre-op 1 week pre-op 4 – 6 days pre-op 2 days pre-op 12 – 24 hrs pre-op Day of op Author Care Group Approval Trust Approval Date of Approval Date of Review Protocol Number Combined oral contraceptive Hormone replacement therapy SERMs, e.g. raloxifene Tamoxifen / anastrazole if prescribed for primary prevention / anovulatory infertility. Continue in women with history of breast cancer. High dose progestogens Adalimumab Infliximab MAOIS depending on anaesthetic technique (except reversible MAOIs, i.e. moclobemide). Refer to anaesthetist and discuss with psychiatry if to be stopped. ALL herbal preparations Fish oil supplements Glucosamine Etanercept Aspirin (only if high bleeding risk) P2Y12 blockers (e.g. clopidogrel, ticagrelor). Check risk with cardiologist. Methotrexate. Check Consultant preference. Oral anticoagulants, e.g. warfarin, dabigatran, rivaroxaban. Refer to specific guidance. Metformin prior to angiograms / angioplasty Long-acting NSAIDs, e.g. piroxicam Ephedra Dipyridamole Lithium (or continue with close monitoring) Donepezil, rivastigmine, galantamine (inform anaesthetist) Reversible MAOIs (moclobemide) depending on anaesthetic technique. Drugs for erectile dysfunction Clozapine (12hrs pre-op) Theophyline (evening pre-op) Short-acting NSAIDs, e.g. diclofenac, ibuprofen (does not include COX 2 inhibitors , e.g.celecoxib) Antispasmodics , e.g. mebeverine Diuretics (ONLY if used for HYPERTENSION ALONE) ACEI/A2RAs (ONLY if used for HYPERTENSION ALONE) Sulfasalazine Azathioprine Methylphenidate Bisphosphonates COX 2 inhibitors , e.g.celecoxib Oral hypoglycaemics stop once NBM Orlistat once NBM Created by Lynne Harris 2008. Updated by Andrew Parker, Lynsey Stephenson & Michelle Thornton Review of existing guidance co-ordinated through email consultation Clinical Standards & Therapeutics Committee Page 26 of 26