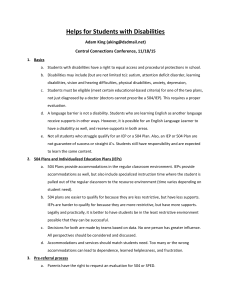
Introduction: Reducing the Use of Restrictive Practices
advertisement

DRAFT Proposed National Framework for Reducing the Use of Restrictive Practices in the Disability Service Sector (the ‘Proposed National Framework’) Consultation Version – May 2013 Introduction: Reducing the Use of Restrictive Practices People with disability who display behaviours that are challenging while in the care of disability service providers may be subjected to restrictive practices that involve restraint (including physical, mechanical or chemical) or seclusion. There is currently no national approach to addressing the use and reduction of restrictive practices by service providers for people with disability across a range of disability service sector settings including institutional and community based care. Whilst present day Disability Acts in jurisdictions indicate principles relating to freedom from abuse; minimum practice standards related to restrictive practices and respective reviews and monitoring are not explicitly identified in every state and territory. Restrictive practices, used in disability services in Australia have been reviewed by the Commonwealth, States and Territories in relation to the National Disability Agreement and relevant legislation, and recommendations have been made for a national framework. Some jurisdictions already have in place or are implementing advanced, comprehensive strategies and are already achieving a reduction in the use of restrictive practices. Reducing and eliminating the use of restrictive practices is consistent with the United Nations Convention on the Rights of Persons with Disabilities and its intent to protect the rights, freedoms and inherent dignity of people with disabilities. As a signatory to the convention, Australia has international obligations to promote, protect and ensure the full and equal enjoyment of all human rights and fundamental freedoms for all people with disability, and to promote respect for their inherent dignity. The commencement of DisabilityCare Australia (formerly known as the National Disability Insurance Scheme) will significantly change the way disability support is funded and accessed. DisabiltyCare Australia will be developing and implementing a quality assurance and safeguards system which will address restrictive practices and protection for participants. In the interim, DisabilityCare Australia will draw on existing State and Territory legislation and/or contractual arrangements with service providers to ensure appropriate restrictive practice laws and policies are observed1. The future development of an NDIS quality assurance and safeguards system will be assisted and informed by the nationally agreed elements of this proposed National Framework. 1 The NDIS legislation and rules recognise that there will be circumstances where the Agency should make a decision that a support must be provided by a qualified person or organisation that meets certain quality and practice standards. This will be the case where any restrictive practices are thought to be necessary to supporting the Participant. This means that in developing the participant statement of supports, the Agency planners will include appropriate supports for the development or implementation of a behavioural management plan in the DisabilityCare Participant plan of supports. DRAFT DRAFT Clients of disability services should be active participants in decisions that affect their lives, support and care. Recognising an individual’s rights is paramount, whereby restrictive practices represents a deprivation of those rights and freedom. There are many relevant stakeholders in the use and reduction of restrictive practices - the client and his or her family, advocates, guardians or significant others, staff at all levels in the disability service sector, and relevant government agencies. Disability services are sometimes challenged to provide safe and therapeutic services for clients who have complex high support needs, as well as providing the safest possible work environment for staff. It has been recognised internationally and domestically that restrictive practices can be significantly reduced and in many cases, eliminated. The proposed National Framework outlines change processes which require leadership and commitment from officials and staff at all levels of organisations and provides the opportunity to demonstrate excellence in delivering safer, quality disability services throughout Australia that are based on evidencebased best practice. This proposed National Framework is an interim step that delivers leadership toward reduction of the use of restrictive practices, which will then be incorporated into the NDIS quality assurance and safeguards that is to be negotiated as part of the full scheme implementation of the NDIS. The timing of launch sites prior to the development of a full NDIS quality assurance and safeguards system will mean that DisabilityCare Australia will be required to assume responsibility for some individuals subject to these practices in some jurisdictions as part of the launch of the NDIS. Detailed negotiations will occur between DisabilityCare Australia, the jurisdiction and the service provider in preparation for transition of these individuals to DisabilityCare Australia. This will ensure DisabilityCare Australia incorporates appropriate supports that aligns to this Framework into that person’s plan. Commonwealth, State and Territory parties who will continue to be responsible for quality assurance systems in the interim may also explore the possibility of amending their regulatory frameworks to accompany this initiative. Further consideration will also be given to options regarding a national or nationally-consistent regulatory framework. DRAFT DRAFT Definitions A nationally agreed set of definitions will guide legislation and policy development, and will facilitate greater inter-jurisdictional collaboration on a national strategy to reduce and safely eliminate restrictive interventions. Therefore, it is proposed that the following definitions will be used where applicable by jurisdictions for implementation, reporting and evaluating progress against the proposed restrictive practices framework. 1. Restrictive intervention A “restrictive intervention” is defined as any intervention and or practice that has the effect of restricting the rights or freedom of movement of a person with disability. 2. Seclusion “Seclusion” means the isolation of a person with disability in a room or physical space at any hours of the day or night where voluntary exit is prevented. 3. Chemical restraint A “chemical restraint” means the use of medication or chemical substance for the primary purpose of influencing a person’s behaviour. It does not include the use of medication prescribed by a medical practitioner for the treatment of, or to enable treatment, of a diagnosed mental illness, a physical illness or physical condition. 4. Mechanical restraint A “mechanical restraint” means the use of a device2 to prevent, restrict or subdue a person’s movement or to influence a person’s behaviour but does not include the use of devices for therapeutic purposes.3 5. Physical restraint A “physical restraint” means the use or action of physical force to prevent, restrict or subdue movement of a person’s body, or part of their body, for the primary purpose of influencing a person’s behaviour. 6. Other restrictive interventions This includes “other” restrictive interventions to those defined above, such as those broadly defined as psycho-social restraints, environmental restraints or consequence-driven restrictive practices. 2 A device may include any mechanical material, appliance or equipment. Therapeutic purposes may include safe travel such as seat belts during transportation or arm splints as part of occupational therapy etc. 3 DRAFT DRAFT Key Guiding Principles The following key principles should guide planning, implementation and evaluation of the National Framework to Reduce the Use of Restrictive Practices in the Disability Service Sector. 1. Australia’s Human Rights and UN Convention on Rights of Persons with Disabilities obligations and National Disability Strategy commitments are met: a. People with disability have the same rights as all people to equality before the law and to equal protection under the law, without discrimination. b. Primary focus of services is to uphold human rights and the well-being, inclusion, safety and quality of life for people with disability. c. All effective measures will be taken to prevent people with disability from being subjected to cruel, inhuman or degrading treatment or punishment. 2. A National Approach: a. Safeguards should, over time, apply across Australia with comparable coverage to make sure people have access to the same protections regardless of where they live. b. All jurisdictions and levels of government have a duty of care to ensure that disability services meet high standards focussed on the best interests of people with disability. c. The Commonwealth and each State and Territory has its own legislative framework and most have a policy framework or statement around reducing restrictive practices. d. Practices, outcomes and reporting are currently diverse in creating a representative picture of the use and reduction in restrictive practices – a national framework aims to deliver a more integrated response between all governments, but does not change core governance arrangements. 3. Person-Centred Focus: a. Approaches will be individualised person-centred, proactive and enhance the quality of life for the person as their focus. b. To strive for the adoption of evidenced-based best practices that support and maximise the person’s decision making, choice and self-direction. c. People with disability, their families, and carers are the natural authorities for their own lives and are in the best place to communicate their choices and decisions and should be consulted in any behaviour support planning. d. Processes that recognise the person’s authority in decision making, choice and control should guide the design and provision of services. DRAFT DRAFT 4. Delivering Quality Outcomes and Safe Work Places: a. Policies, procedures and tools should safeguard the rights of people with disability, focussing on improving clients’ quality of life, reducing the use of restrictive practices and monitoring the use and reduction in restrictive practices. b. Protection against inhuman or degrading treatment – attention to personal dignity, privacy and self-respect as well as individual needs. c. Recognise that the use of restrictive practices may reflect a failure in the service system to understand the nature and function of the individual’s behaviour, and to respond appropriately to that behaviour. d. Review mechanisms are developed, maintained and utilised for: client de-briefing; review of restrictive practices used (incident reporting); assessment of appropriateness and alternatives; and for aggregated reporting on an organisational and service provider basis. 5. Accountability through documentation, benchmarking and evaluation working toward transparent and consistent reporting. a. Transparent reporting mechanisms to ensure accountability and involvement of stakeholders, and to allow for the analysis of trends to evaluate the effectiveness of the regulation, and recognise where there may be an increased reliance on the use of restrictive practices b. Ability to measure success through a national picture (or stocktake) of the use and reduction of restrictive practices. DRAFT DRAFT Core Strategies for a National Framework for Reducing of the Use of Restrictive Practices in the Disability Service Sector All jurisdictions should implement a set of key core strategies with their respective service providers by 2018 to reduce the use of restrictive interventions in disability services. The core strategies presented in this National Framework have been developed based on national and international evidence based practice in the fields of mental health and disability. The six core strategies are: 1. Person Centred Focus Including the perspectives of service users and carers during restrictive practice incident de-briefing, individualised care planning, staff education and training, and policy and practice development is a key element of restraint minimisation across sectors (Source Note: Azeem et al., 2011). Key implementation areas are: a. Development and regular review of individual behaviour support plans (including de-escalation and safety) in conjunction with service users and carers b. Development and use of appropriate behavioural and environmental risk assessment tools by service providers c. Development of evidence-based interventions such as teaching the use of replacement skills (skills the person can use to replace the behaviours of concern), based on the principles of positive behaviour support. 2. Leadership towards organisational change Leaders play an important role in facilitating processes, structures and resources for supporting change. The senior management of services must create a goal of reducing restrictive practices, and make it a high priority. Leaders must also support their staff through workforce development opportunities, the development of restraint and seclusion reduction tools, and implementation of rigorous evidence-based debriefing techniques to move away from the use of restrictive interventions (Source Note: Williams and Grossett, 2011). Key implementation areas are: a. Leaders at all levels commit to implement reduction in the use of restrictive practices b. Governments provide strategic direction to service providers c. Service providers form relevant governance structures and groups to provide organisational support mechanisms aimed at reducing restrictive practices. DRAFT DRAFT 3. Use of data to inform practice Mechanisms to trigger periodic review of restraint authorisations, client assessments and behaviour support plans are necessary to continuously assess the necessity of restrictive practices and possible restrictive practices alternatives. Data is also important to determine what factors are effective in reducing the use of restrictive interventions (Source Note: Webber et al., 2012). Key implementation areas are: a. Collection of data at a service unit and/or organisational level b. Identification of baseline data, ability to set improvement and performance targets, and to evidence how this will be used to reduce reliance on restrictive practices c. Development and maintenance of an auditing tool aimed at auditing when restrictive practices are used, the frequency with which they are used. The tool should have capacity to feed back into the support of clients, risk assessments and service review– preferably integrated with service provider staffing and management systems. 4. Workforce development There is good evidence to show that disability support staff who understand positive behaviour support, functional behaviour assessment as well as a focus on skills for trauma informed care, risk assessment, de-escalation, and restrictive intervention alternatives are able to provide good support and reduce their use of restrictive interventions to people who have complex needs. Key implementation areas are: a. Training and education for staff and managers, including on restraint reduction, risk assessment and positive behaviour support b. Service providers implement guidelines, processes and protocols for staff and managers c. Debriefing and support – continuous improvement for staff at all levels. 5. Use within services of restraint and seclusion reduction tools Restrictive practices reduction tools need to be based on core assessment and prevention approaches, the results of which need to be integrated into each individual’s support plan. These approaches would include: Proven assessment tools which screen for increased risk of violence, physical and emotional issues which counter-indicate restrictive interventions Emergency management plans Changes to the therapeutic environment Introduction to meaningful activities. (Source Note: Huckshorn, 2005). Key implementation areas are: a. Practice guides and reference material for staff, and managers b. Integration with service provider staffing and management systems. DRAFT DRAFT 6. Debriefing techniques Following an emergency use of a restrictive intervention, an immediate “post event” debriefing is completed on site led by the appropriate senior staff member on duty. The goal of this immediate debriefing is to ensure that everyone is safe, that satisfactory information is available to inform the later structured debriefing process and that the consumer subject to the restraint is safe and being appropriately monitored. Formal debriefing occurs one to several days after the event and includes all involved, the treatment team and relevant administrative staff. The structure of the formal debriefing should follow the steps taken in a root cause analysis. The consumer or their proxy must be involved in all stages of the debriefing process. (Source Note: Huckshorn, 2005). Key implementation areas are: a. Practice guides and reference material for staff at all levels. Measuring Performance/ Effectiveness Jurisdictional reporting on progress of the implementation of the National Framework will occur on a biennial basis. Monitoring of the National Framework for reducing the use of restrictive practices in the disability service sector will provide enhanced accountability, public transparency and a national picture and measurement of effectiveness. By 2018, all jurisdictions are encouraged to implement a data monitoring system that integrates with existing service delivery management systems. This work will initially focus on seeking agreement to achieve standardised data collection and reporting (including for voluntary reporting where commitments occur) in order to establish benchmarks and performance indicators that measure effectiveness in reducing restrictive practices over time. Milestones will be developed which take an incremental approach toward reaching data reporting capacity on the use of restrictive practices by services. Future opportunities may arise through the evaluation of the National Framework, for expansion of these six core strategies to be integrated into other mainstream service sectors that support people with disability such as in health, education and criminal justice. DRAFT DRAFT References Azeem, M.W., Aujla, A., Rammerth, M, Binsfeld, G., & Jones R.B. (2011). Effectiveness of six core strategies based on trauma informed care in reducing seclusions and restraints at a child and adolescent psychiatric hospital. Journal of Child and Adolescent Psychiatric Nursing 24, 11–15. Huckshorn, K.A. (2005). Six Core Strategies to Reduce the Use of Seclusion and Restraint Planning Tool. Alexandra, VA: National Technical Assistance Centre. Sanders, K. (2009). The effects of an action plan, staff training, management support and monitoring on restraint use and costs of work-related injuries. Journal of Applied Research in Intellectual Disabilities, 22, 216–220. Webber, L.S., Richardson, B., Lambrick, F., & Fester. (2012). The impact of the quality of behaviour support plans on the use of restraint and seclusion in disability services. International Journal of Positive Behavioural Support, 2 (2) 3-11. Williams, D.E., & Grossett, D.L. (2011). Reduction of restraint of people with intellectual disabilities: An organizational behavior management (OBM) approach Research in Developmental Disabilities 32, 2336–2339. DRAFT