Supplemental methodology: Supplemental Figure 1 and legend
advertisement

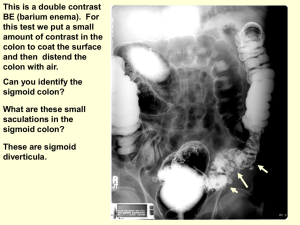
Supplemental methodology: Supplemental Figure 1 and legend Flow diagram illustrating workflow process: Phase one (left): surgical mobilisation of the colon and mesocolon was recorded, edited, audio included, and a three dimensional model of the mesenteric organ was rendered using Blender ©. An accompanying detailed text commentary was generated (see below in supplementary methods “surgical mobilisation”). 2.5 dimension illustrations were extracted from the model and utilised to demonstrate the sites of sample harvest. Phase two (right): Samples were harvested pre and post-mobilisation from sites indicated in Figure 1 (see manuscript). These were prepared as described, stained as indicated, then interpreted via consensus by KC, FQ, PD and JCC. Sample Processing: To stain with H&E sections were first dewaxed with xylene, and then bathed in a series of ethanol solutions of decreasing concentration. Staining was then performed with Mayer’s haematoxylin for 6 minutes, a rinse in running water for 4 minutes and counterstaining with eosin for 2 minutes. Following staining, specimens were then dehydrated through a series of ethanol solutions of increasing concentration, and cleared with xylene prior to mounting media and a cover slide being applied. To apply Masson’s Trichrome with Gomori’s Aldehyde Fuchsin, specimens were brought to water via xylene and a series of ethanol solutions of decreasing concentration. Specimens were then oxidised in equal parts 0.5% KMnO4/0.5% H2SO4 for 2 minutes, then rinsed in tap water and bleach in 2% Sodium Metabisulphite for another 2 minutes, before being washed in water 30 seconds, followed by 70% ethanol for 1 minute. Following this, specimens were sequentially stained in Gomori’s Aldehyde Fuchsin for 1 min, Celestine blue for 4 minutes, and Mayer’s Haemalum for 4 minutes, with appropriate rinses. Next, specimens were differentiated in acid alcohol for 20 seconds, and then rinsed with running tap water for 4 minutes before being stained in Masson’s Cytoplasmic Stain for one minute. After this step they were rinsed briefly in water and differentiated in 1% dodeca-Molybdophosphoric Acid for 2 minutes. Next they were rinsed in water and counterstained in fastgreen or light green for 1 min. Finally, specimens were differentiated in 1% acetic acid, dehydrated through a series of ethanol solutions of increasing concentration, and then cleared with xylene. Following this, mounting media and a cover slide were applied. Samples for immunohistochemisty were initially dewaxed in xylene and then brought to TBS through a series of ethanol solutions of decreasing concentration. 3x 5 minutes rinses in TBS were then carried out. Samples were then incubated in 3% H2O2/methanol for 30 minutes, followed by a further 3 rinses in TBS. Antigen retrieval step was then carried out; slides were placed in a sodium citrate buffer, in a water steamer, for 20 minutes, followed by a further 3x 5 minute rinses in TBS. Samples were then blocked with 5% goat serum solution for 2 hours, at room temperature. The primary antibody was then applied, (a 1:200 dilution of podoplanin in the blocking solution), with slides incubating overnight at 4oC. The following day slides were rinsed 3x 5 minutes in TBS prior to the secondary antibody being applied for 30 minutes. Slides were again rinsed in TBS for 3x minute cycles. Following this the slides are developed with AEC chromogen for up to 30 minutes. Once satisfactory staining has been confirmed by brief light microscopy, slides were rinsed in running water for 5 minutes, before being counterstained with 20% Mayer’s haematoxylin for 30 seconds. Finally slides were rinsed, wiped carefully and coverslipped using an aqueous mounting media. Surgical mobilisation: Surgical mobilisation: In one cadaver, the entire colon and mesocolon were surgically mobilised as previously described.2 A video recording of the entire process is also included in the supplementary methodology. Figures 2A-D (see over) are axial views of the mesocolon (A) and mesosigmoid (B-D) that depict the relationship with the underlying connective tissue fascia and retroperitoneum. These schematic representations thus depict the structures forming the planes that are utilised during surgical mobilisation. Similar anatomic relationships occur on the right side and thus are not included in this image. Figure 2B demonstrates the mesosigmoid just distal to the junction with the descending (left) colon. Figure 2C demonstrates the mesosigmoid at approximately the mid-point of the sigmoid colon. Figure 2D demonstrates the mesosigmoid and sigmoid just proximal to the junction with the rectum Figure 3A-E (left) are schematic and colored illustrations of (A) the entire mesocolon, (B) the right mesocolon and contiguity with the small intestinal mesentery, (C) the hepatic flexure with the colonic component conceptually removed, (D) the splenic flexure with the colonic component conceptually removed and (E) the left mesocolon with the sigmoid colon removed. In each the grey area represents connective tissue present between the colon/mesocolon and the retroperitoneum. This is the connective tissue that must be separated in mesofascial separation in order to achieve mobilisation. In B-E the hepatocolic and splenocolic condensations, and greater omentum, are not included in order to simplify the illustration. As part of flexural mobilisation these “ligaments” (i.e. condensations of greater omentum) must be divided to provide access to the plane required for mobilisation of the colonic and mesenteric components of the flexures. Ileocaecal junction and right colon/mesocolon: In brief, the peritoneal fold inferolateral to the ileocaecal mesenteric confluence was sharply divided in a process that was continued proximally along the root of the small intestinal mesentery. This exposed the interface between fascia and overlying mesentery/mesocolon from duodenal to ileocaecal level. By separating the mesentery/mesocolon from the fascia and thus retroperitoneum (i.e. mesofascial separation) the entire small intestinal mesentery was fully mobilised. Next, the right-sided lateral peritoneal fold was sharply divided exposing the interface between right mesocolon and underlying fascia. In separating both these structures (i.e. mesofascial separation), the right mesocolon was now fully mobilised and observed as contiguous with the small intestinal mesentery. Hepatic flexure and transverse mesocolon: The hepatocolic ligament (a lateral condensation of the greater omentum) was sharply divided thereby exposing the cephalad surface of the hepatic mesenteric confluence. Continuing this process medially across the transverse colon, the greater omentum was fully separated from the transverse mesocolon and the latter could now be observed as being contiguous with the hepatic mesenteric confluence. Using mesofascial separation the mesenteric confluence was then separated from the second part of the duodenum and the head of the pancreas as far medially as the origin of the transverse mesocolon (i.e. at the origin of the middle colic artery). Without disrupting the middle colic adipovascular pedicle, mesofascial separation continued laterally along the body and tail of pancreas towards the splenocolic ligament (also a lateral condensation of the greater omentum) which was then sharply divided. Splenic flexure and left colon/mesocolon: Next, the left lateral peritoneal fold was sharply divided exposing the interface between left mesocolon and underlying fascia. These were separated to mobilise the left mesocolon off the retroperitoneum. By extending this process towards the splenic flexure, and onto the splenocolic ligament, the splenic mesenteric confluence (i.e. the splenic flexure) was now fully mobilised. The left mesocolon could then be fully medialised. Sigmoid and mesosigmoid: The lateral peritoneal fold associated with the apposed mesosigmoid (i.e. at the junction of both apposed and mobile components of the mesosigmoid) was sharply divided exposing the interface between apposed mesosigmoid and underlying fascia (mesofascial separation). Both were again separated and the apposed mesosigmoid was fully medialised. To aid this, the upper mesorectum was separated from associated fascia. This completed the mesocolic mobilisation in the mesofascial plane and the mesocolon was evident as a contiguous structure from small intestinal mesentery to mesorectal level. Slide review: This was conducted by consensus rather than via independent observations. This process involved slide review by four investigators (KC, FQ, PD and JCC). We felt this approach was necessary as both FQ and PD are both anatomists trained in the traditional mode of mesocolic and mesenteric appraisal (i.e. that the mesocolon is fragmented rather than contiguous). KC is a surgical trainee whilst JCC is a practicing colorectal and general surgeon. Thus both KC and JCC appraised the mesocolon as contiguous (in keeping with the surgical approach to the same). Prior to review, both FQ and PD were appraised of mesocolic contiguity from small bowel mesenteric to mesorectal level. This was demonstrated to both via surgical mobilisation of the mesenteric organ from duodenum to rectal level. Supplementary results: Figure 4 A-G: Schematic colored illustrations of the mesosigmoid and intersigmoidal fossa. 4(A) represents the sigmoid colon and mesocolon in the undisturbed state. The dotted line represents the lateral border of the apposed mesosigmoid. 4(B) Here the mobile sigmoid has been partially deflected medially to demonstrate the peritoneal adhesions (i.e. congenital attachments) between the lateral surface of the mesosigmoid and the peritoneum of the left iliac fossa. Once these are divided then the sigmoid can be fully deflected medially and the true intersigmoidal fossa becomes apparent as indicated. Figures 4D-G represent axial views of the sigmoid and mesosigmoid as one progresses distally from the descending colon to the junction with the rectum. The levels correspond to the lines a-d depicted in Figure 4A. The intersigmoid fossa is depicted in each illustration. Supplementary Figure 5: (A) Photomicrograph (Massom`s Trichrome) of fascia and retroperitoneum following mobilisation of the ascending mesocolon. The superficial layers of the fascia were fragmented whilst in deeper layers lamellae of collagen remained intact. (B) Photomicrograph (haematoxylin and eosin, (H&E)) demonstrating the mesothelial monolayer evident between connective tissue and retroperitoneum (Scale 100 µm). (C) Photomicrograph (H&E) demonstrating the underlying fascia, mesothelial monolayer and retroperitoneum following mobilisation of the descending mesocolon. Superficial layers of the connective tissue were fragmented whilst deeper layers remained contiguous. Scale 100 µm. Figure 6: Immunohistochemical evaluation of lymphatic channels as identified using podoplanin. (A) Positive control taken from tonsil tissue and counterstained with eosin. (B) Podoplanin positivity (arrow) in submesothelial connective tissue in ascending mesocolon. (C) Podoplanin immunopositivity in vessel located within Toldt`s fascia (further example shown in inset). (D) Podoplanin positivity within a fibrous connective tissue septum within the transverse mesocolon. Acknowledgements: The authors would like to acknowledge Mr Joe Pangrace in the Medical Illustration Department of the Cleveland Clinic (Ohio) for the schematic illustrations provided in the supplementary methodology and results.