Interhospital Conference Case 4 Parathyroid Carcinoma (PCA
advertisement

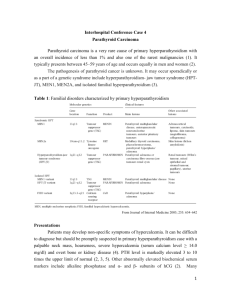
Interhospital Conference Case 4 Parathyroid Carcinoma (PCA) Parathyroid carcinoma is an uncommon cause of PTH-dependent hypercalcemia. In most series, this entity accounts for < 1% of patients with primary hyperparathyroidism. The disease may be somewhat more common in Japan than in Western countries, accounting for 5% of patients with primary hyperparathyroidism (1). Familial hyperparathyroidism Carcinoma has been reported in association with familial hyperparathyroidism, particularly in the autosomal dominant form with isolated hyperparathyroidism that is not part of the multiple endocrine neoplasia type I (MEN1) In addition, a greatly increased risk of parathyroid carcinoma is associated with the hereditary hyperparathyroidism-jaw tumor syndrome(1), recently localized to chromosome 1q21-q31(2). Incidence increased to 15% in this group of patient. In 2002, gene encoded parafibromin protein was identified and named HRPT2 gene. Various mutations in this gene can cause the syndrome. Recently its name was changed to CDC73 (cell division cycle protein 73) gene. More than half of patients with HPT-JT have germ line mutation of this gene. But somatic mutation can also be identified in sporadic case (3). Clinical features The clinical features of parathyroid carcinoma are due primarily to the effects of excessive secretion of PTH by the functioning tumor rather than to infiltration of vital organs by tumor mass. Thus, signs and symptoms of hypercalcemia often dominate the clinical picture, with contributions from typical hyperparathyroid bone disease and features of renal involvement, such as nephrolithiasis or nephrocalcinosis. The challenge to the clinician rests upon differentiating between hyperparathyroidism due to parathyroid carcinoma and that due to its much more common benign counterpart. The serum calcium level of most patients with parathyroid carcinoma is much higher, generally above 14 mg/dL or 3–4mg/dL above the upper limit of normal. Moreover, this more severe hypercalcemia is almost invariably associated with the typical signs and symptoms of hypercalcemia. The most frequent complaints are fatigue, weakness, weight loss, anorexia, nausea, vomiting, polyuria, and polydipsia. A palpable neck mass has been reported in 30–76% of patients with parathyroid carcinoma. This important clinical finding constitutes another striking difference between benign and malignant parathyroid disease, as a palpable neck mass is distinctly unusual in primary hyperparathyroidism. In addition, recurrent laryngeal nerve palsy in a patient with primary hyperparathyroidism who has not had previous neck surgery is also very suggestive of parathyroid cancer(1). Natural history Parathyroid carcinoma is an indolent,slow progression with rather low malignant potential. It tends to recur locally at the operative site and spread to contiguous structures in the neck. Metastases occur late in the course of the disease with spread via both lymphatic and hematogenous routes. Cervical nodes (30%) and lung (40%) are involved most commonly, followed by liver (10%). Occasional involvement of bone, pleura, pericardium, and pancreas has been reported (1). Diagnosis PCA is characterized by very high levels of PTH, which ultimately result in severe hypercalcemia. In addition, high alkaline phosphatase, hypophosphatemia, and hyperchloremic metabolic acidosis have also been observed in PCA patients (4). Imaging of PCA Ultrasound: A hypo-echoic soft tissue mass with irregular, poorly defined border and sign of invasion of adjacent structures (5). CT scan: Use to differentiate abnormal parathyroid tissues from lymph nodes and normal thyroid tissue ,and invasion into adjacent tissue(5). MIBI scintigraphy: (sensitive 91%) Use to assess the presence and localization of PCA but may failed to localize mediastinal and pulmonary recurrence(5). FDG PET/CT: Very sensitive tool to evaluate extension of disease at initial staging. Identification of suspected tumor recurrence, evaluation of residual disease after primary treatment. Loss of sensitivity and specificity in some conditions (i.e. small lesions and early stage)(6). Pathology Grossly large masses adherent to adjacent structures, capsular invasion (criteria as thyroid), growth into adjacent tissues ,and metastases. Thick intratumoral fibrous bands is good indicator of malignancy but not pathognomonic. Diffuse nuclear enlargement with macronucleoli suggests malignancy (5). Management Surgical Surgery is the only effective and curative treatment. It should be performed as “en bloc” tumor resection with ipsilateral thyroidectomy to avoid any capsular rupture. After an “en bloc” removal of PCA, a drop of > 50% iPTH from baseline was predictive at least 6 months of normocalcemia(5). Adjuvant therapy PCA is not a radiosensitive tumor. Radiation therapy in PCA remains controversial (5). Chemotherapy Attempts to control tumor burden with chemotherapy have been disappointing and data limit to scattered case reports (1). Management of hypercalcemia (medication) When PCA become widely disseminated and surgical resection is no longer effective, goal at this point is to control the hypercalcemia. Bisphosphonates 1)Pamidronate : Transiently effective in lowering serum calcium(1) 2) Zoledronic acid: More potent than pamidronate in treating hypercalcemia of malignancy, would also be effective for hypercalcemia due to parathyroid carcinoma (7). Calcimimetics Drug that reduces PTH secretion by increasing the sensitivity of the calcium-sensing receptor. Cinacalcet, Sensipar®, a longer-acting calcimimetic drug, is available for the treatment of hypercalcemia in parathyroid cancer. In a 16-week open-label study of 29 patients with inoperable parathyroid carcinoma, cinacalcet (dose titrated to achieve calcium ≤10 mg/dL or up to 90 mg four times daily) successfully reduced serum calcium concentration by at least 1 mg/dL in 62% of patients. Mean PTH levels decreased but not significantly. Adverse events (nausea, vomiting, headache, dehydration) were common and resulted in discontinuation in five patients (8). Anti-Parathyroid Hormone Immunotherapy: Breaking normal immune tolerance to PTH using human and bovine PTH-like immunogenic fragments to stimulate the production antibody that would cross-react with human PTH,PTH immunization can improve clinical, hormonal, and biochemical measures and antitumor effect in patients with metastatic PCA(9). Prognosis No one characteristic can predict the outcome of PCA. Early recognition and complete resection at the time of the initial surgery carry best prognosis. Average time surgery to first recurrence is 3yrs (up to 20 yr have been reported).Once tumor has recurred; complete cure is unlikely, although prolonged survival is still common under these circumstances with palliative surgery. Five-year survival rates vary from 40–86% and 10-yr survival to be approximately 49 % (1). Reference 1. Shane E 2001 Clinical review 122: parathyroid carcinoma. J Clin Endocrinol Metab 86:485–493 2. Szabo J, Heath B, Hill VM, et al. 1995 Hereditary hyperparathyroidism-jaw tumor syndrome: the endocrine tumor gene HRPT2 maps to chromosome1q21–q31. Am J Hum Genet. 56:944 –950. 3. Shattuck TM, Välimäki S, Obara T, Gaz RD, Clark OH, Shoback D et al. Somatic and germ-line mutations of the HRPT2 gene in sporadic parathyroid carcinoma. N Engl J Med. 2003;349(18):1722. 4. Abdelgadir Adam M, Untch BR, Olson JA Jr. Parathyroid Carcinoma: Current Understanding and New Insights into Gene Expression and Intraoperative Parathyroid Hormone Kinetics Oncologist. 2010;15(1):61-72. 5. Antoine Digonnet, Adelaïde Carlier, Guy Andry. et.al Parathyroid Carcinoma: A Review with Three Illustrative Cases .Journal of Cancer 2011; 2: 532-537 6. Laura Evangelista, Nadia Sorgato, Francesca Torresan,et al. FDG-PET/CT and parathyroid carcinoma: Review of literature and illustrative case series World J Clin Oncol 2011 October 10; 2(10): 348-354 7. P. Major, A. Lortholary, J. Hon, E. Abdi,et.al. Zoledronic Acid Is Superior to Pamidronate in the Treatment of Hypercalcemia of Malignancy: A Pooled Analysis of Two Randomized, Controlled Clinical Trials. Journal of Clinical Oncology, Vol 19, No 2 (January 15), 2001: pp 558-567 8. S. J. Silverberg, M. R. Rubin, C. Faiman et al. Cinacalcet Hydrochloride Reduces the Serum Calcium Concentration in Inoperable Parathyroid Carcinoma J Clin Endocrinol Metab 2007;92(10):3803–3808. 9. D. BETEA, A. R. BRADWELL, T. C. HARVEY et al. Hormonal and Biochemical Normalization and Tumor Shrinkage Induced by AntiParathyroid Hormone Immunotherapy in a Patient with Metastatic Parathyroid Carcinoma J Clin Endocrinol Metab 2004; 89(7):3413–3420