What is chromosome screening with approved sex
advertisement
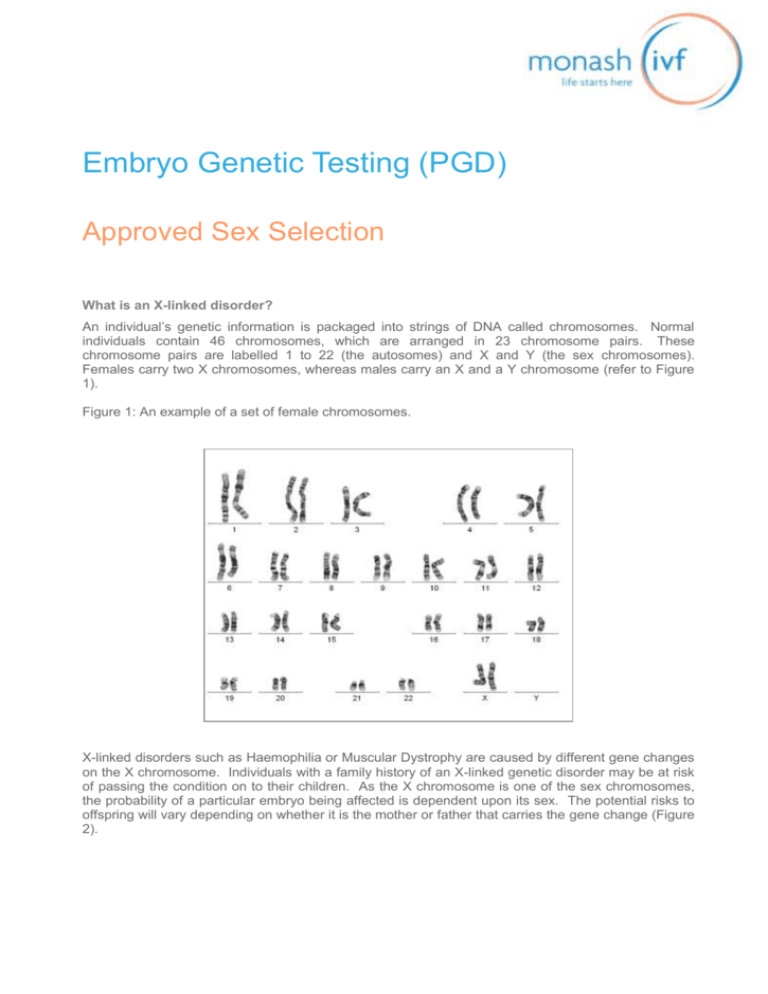
Embryo Genetic Testing (PGD) Approved Sex Selection What is an X-linked disorder? An individual’s genetic information is packaged into strings of DNA called chromosomes. Normal individuals contain 46 chromosomes, which are arranged in 23 chromosome pairs. These chromosome pairs are labelled 1 to 22 (the autosomes) and X and Y (the sex chromosomes). Females carry two X chromosomes, whereas males carry an X and a Y chromosome (refer to Figure 1). Figure 1: An example of a set of female chromosomes. X-linked disorders such as Haemophilia or Muscular Dystrophy are caused by different gene changes on the X chromosome. Individuals with a family history of an X-linked genetic disorder may be at risk of passing the condition on to their children. As the X chromosome is one of the sex chromosomes, the probability of a particular embryo being affected is dependent upon its sex. The potential risks to offspring will vary depending on whether it is the mother or father that carries the gene change (Figure 2). Figure 2: An example of the possible embryo outcomes if the female partner carries an X-linked disorder. The X chromosome carrying the gene change is indicated by Xa. Mother Father X Xa XY Carrier Normal Possible Embryo Outcomes Embryo 1 Embryo 2 Embryo 3 Embryo 4 XX XY Xa X Xa Y Normal Female Normal Male Carrier Female Affected Male What is chromosome screening with approved sex selection? Preimplantation Genetic Diagnosis (PGD) with sex selection is only approved in Australia if the testing is being performed to avoid the risk of transmitting a specific X-linked genetic disorder on to a child. PGD with approved sex selection can be used to screen IVF embryos to determine the sex of the embryo prior to implantation. In addition to screening for embryo sex, this testing will provide information regarding chromosome copy number. Some embryos can have an abnormal number of chromosomes (ie: missing or extra chromosome/s) due to errors in cell division in the developing egg, sperm or embryo. This is known as chromosomal aneuploidy. An aneuploid embryo will fail to implant, miscarry, or result in the birth of an affected child (eg: a child with Down syndrome). PGD testing with approved sex selection will simultaneously test for aneuploidy involving any chromosome. Only embryos of the desired sex that have the correct number of chromosomes will be selected for transfer to the uterus. This testing significantly increases the chance of having a healthy baby. It is well documented that the frequency of chromosomal abnormalities in embryos increases with maternal age. Therefore, older women will be less likely to obtain a “normal” embryo for transfer compared with younger women (refer to Figure 3). The number of embryo/s potentially available for transfer will be further decreased once the sex of the embryo is also considered. However, once a “normal” embryo of the desired sex is identified for transfer, the pregnancy rate in older women is not significantly different from that of younger women. Figure 3: Percentage of ‘normal’ embryos on Day 3 versus Day 5 of embryo development (irrespective of sex). 80 “Normal” embryos (%) 70 60 50 Day 3 40 Day 5 30 20 10 0 27 29 31 33 35 37 Maternal Age 39 41 43 45 How is chromosome screening with approved sex selection done? Step 1: Genetic counselling in PGD clinic Prior to the commencement of an IVF cycle, the couple attend an appointment with a clinical geneticist and/or genetic counsellor. During this appointment the couple will be provided with information relating to PGD and will have an opportunity to have any questions answered. This appointment is free of charge and enables couples to decide if PGD is the right option for them. Step 2: IVF and Embryo biopsy All couples undergoing PGD with approved sex selection must undertake an IVF cycle to stimulate the woman’s ovaries to produce a number of eggs. These eggs are collected and fertilised using the male partner’s sperm. The resulting embryos are cultured in the laboratory and their growth is monitored on a daily basis. Embryo biopsy (sampling cell/s from the embryo for genetic testing) can be performed at two different stages during an embryo’s development: 1. Day 3 embryo biopsy is performed 3 days after fertilization, when the embryo is at the cleavage stage and is typically composed of 6 to 8 cells. Embryos that have developed to at least 5 cells on Day 3 are suitable for biopsy. A hole is drilled in the outer shell of the embryo and 1 or 2 cells are removed for genetic analysis (refer to Figure 4). Figure 4: Day 3 embryo biopsy 2. Day 5/6 embryo biopsy is performed 5 or 6 days after fertilization. By this time, the embryo should have developed to the blastocyst stage, and should be comprised of an inner cell mass (which will go on to form the fetus) and trophectoderm cells (which will go on to form the placenta). Embryos need to have a clear inner cell mass and a suitable number of healthy trophectoderm cells to be considered suitable for biopsy. Approximately 5 trophectoderm cells are removed for genetic analysis (Refer to Figure 5). Figure 5: Day 5/6 embryo biopsy In the majority of cases, Monash IVF recommends Day 5/6 biopsy. This is due to the following reasons: Randomised control trials have shown that Day 5/6 biopsy is better for the embryo compared with Day 3 biopsy (Scott et al, 2013). The embryo has more cells on Day 5/6 of development (~100 to 150 cells) compared with Day 3 of development (~6 to 8 cells). This means: - More cells can be biopsied for genetic testing on Day 5/6 of development compared with Day 3 of development (ie: approximately 5 cells versus 1-2 cells, respectively). The availability of more cells improves the accuracy of the PGD test results. - Despite biopsying more cells from Day 5/6 embryos, a smaller percentage of cells is removed from the embryo following a Day 5/6 biopsy compared with a Day 3 biopsy (ie: we are removing approximately 5/100 (5%) cells on Day 5/6, compared with 1/6 (17%) cells on Day 3). Day 5/6 embryos are more likely to be chromosomally normal then Day 3 embryos (as some of the embryos that are abnormal on Day 3 do not have the developmental capacity to grow to Day 5/6 in culture). Therefore, growing the embryos to Day 5/6 before performing the PGD testing provides an element of natural selection. Day 5/6 embryo biopsy enables the patient to confirm that their embryos are capable of developing to an advanced stage in culture before proceeding with PGD testing. The alternative is to perform PGD testing on Day 3 with the knowledge that the embryos may not continue to develop and therefore may not be suitable for transfer from an Embryology perspective. Step 3: Genetic testing The biopsied cells are transferred to a small test tube for genetic testing. Monash IVF currently offers approved sex selection using two different test types, called Array-CGH and SNP array testing. More information on each of these test types is included below: 1. Array-CGH (performed using 24Sure technology) In this procedure, the DNA from the embryonic cells is multiplied thousands of times (to generate enough DNA for testing) and is then fluorescently labelled. Once labelled, the DNA sample is placed on a microarray platform. This microarray platform consists of a matrix of thousands of different DNA probes which are specific to each chromosome. The fluorescently labelled DNA from the embryo biopsy sample binds to the DNA probes on the microarray platform. By comparing the fluorescent intensity of the embryo biopsy sample with that of a control male and control female sample, it is possible to determine the sex of the embryo as well as the copy number of each chromosome in the biopsied cell/s (Figure 6). Figure 6: Array-CGH procedure + Test cell/s Test DNA 46,XY (male) Control DNA 46,XX (female) Control DNA Loss of fluorescence relative to controls indicates the embryo is missing a chromosome Same fluorescence as controls indicates the embryo has the normal number of chromosomes Gain of fluorescence relative to controls indicates the embryo has an extra chromosome 2. SNP array testing (performed using “parental support”) In this procedure, the DNA from the embryonic cells is multiplied thousands of times (to generate enough DNA for testing) and is placed on a microarray platform. This microarray platform contains probes for over 300,000 different DNA sites. The DNA from the embryo biopsy sample binds to the DNA probes on the microarray platform. Following binding, it is possible to “read” the DNA code at each of these DNA sites. By screening a blood sample from each partner in parallel with the embryonic cells, it is possible to determine which chromosome/s the embryo inherited from each parent (Figure 7). In addition to determining the sex of the embryo and chromosome copy number, this testing is capable of identifying the source of any additional or missing chromosomes (ie: maternal or paternal origin). This information may be useful to assist the patient with future reproductive decision making. Figure 7: PGD testing method using SNP arrays. + Test cell/s DNA from male partner Test DNA DNA from female partner A T G C T T A T G C A T A T G C A T A T G C G C A T G C G G A T G C C C A T G C A T A T G C T A A T G C A T A T G C C A A T G C A C A T G C A A A T G C G G A T G C C G A T G C C G Chromosomes inherited by embryo Step 4: Embryo transfer Because of the time taken to perform the genetic testing, the embryos must be frozen following biopsy. Final results are usually available 2 to 3 weeks after biopsy. If available, one or two normal embryos can be thawed for use in a frozen embryo transfer cycle. A PGD scientist/Embryologist will discuss the PGD results with the patient prior to transfer. The patient’s IVF nurse will organise a pregnancy test to be performed on Day 16 of the frozen embryo transfer cycle. This process should increase the chance of an unaffected pregnancy and significantly reduce the risk of miscarriage. Surplus normal embryos of the desired sex will remain in storage. These embryos may be used in a subsequent cycle. Chromosomally abnormal embryos will be removed from storage and allowed to succumb. What type of chromosome screening is best for me? There are differences in the testing capabilities of array-CGH compared with SNP arrays. SNP array testing (with parental support) has the diagnostic advantage of being capable of detecting a wider range of chromosome abnormalities than array-CGH (Table 1). However, as array-CGH is charged on a per embryo basis, this testing may appeal to patients with small embryo numbers who would otherwise elect not to proceed with 24 chromosome screening. Genetic counselling is an important step to help patients understand the differences between these two types, so that they make an informed decision regarding which test type is best in their case. The PGD testing option that is performed will be decided by the patient in consultation with their IVF specialist and Genetic Counsellor. Table 1: Detection capabilities of array-CGH compared with SNP arrays. Array-CGH SNP arrays Determine embryo sex Screen 24 chromosomes Some Some x Determine the parental origin of chromosome abnormalities x Confirm genetic parentage x Detect extraneous DNA contamination x Criterion Detect haploidy (a missing set of all chromosomes, which results in implantation failure) Detect triploidy (an extra set of all chromosomes, which results in implantation failure or miscarriage) Detect uniparental disomy (the presence of two copies of a given chromosome from one parent and none from the other. This can result in particular genetic syndromes or medical, cognitive or physical disabilities). Why choose Monash IVF for PGD? Monash IVF has offered PGD as a clinical service since 1996 and is one of the few centres in Australia that specialises in this area of reproductive medicine. In 1996 we were proud to report the birth of Australia’s first PGD babies and since then we have performed over 3,000 PGD cycles with proven high success rates. Our specialised genetics team contains highly qualified experts in PGD, ensuring the best quality of care for patients. The genetics team at Monash IVF is responsible for providing a specialised PGD service not only to our own patients, but also to patients undergoing IVF cycles at fourteen different IVF clinics throughout Australia and New Zealand. While the main PGD laboratory is located in Clayton, Melbourne, Australia, embryo biopsy can be performed away from the genetics laboratory and the embryonic cells sent by courier to Clayton. Centralising the genetic testing enables patients to access the highest levels of expertise without having to leave their home state. Where can I get more information? If you would like further information regarding the PGD program at Monash IVF, please feel free to contact a member of the Genetics team on +61 3 9543 2833.