"OR Temperature: Maintaining Perioperative Normothermia to
advertisement

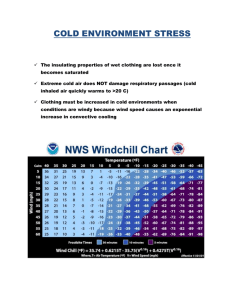
OR Temperature: Maintaining Perioperative Normothermia to Minimize the Risks of Adverse Events Related to Hypothermia. Hypothermia is the most frequent and significant perioperative temperature problem and is associated with many well-known complications. Data shows 5070% of all surgical patients experience perioperative hypothermia. In addition, maintenance of normothermia can result in a reduction of patient costs by an estimated $2500-7000 per patient (AANA, 2013). Thermoregulation is minimally impaired against heat under anesthesia, that being said, hyperthermia, which includes passive, febrile, and malignant, deserve its own presentation, therefore I will not be discussing about it. 1. What is hypothermia? Condition marked by an abnormally low internal body temperature (below 36°C) that occurs when systemic heat loss exceeds heat production. The degree of heat loss is determined by the patient’s interaction with the environment (Nagelhout, p 1235). a. How do patients lose heat in the OR? i. Radiation-transfer of heat from our warm bodies into cooler environment (walls, ceiling, equipment). This is the most significant mechanism of heat loss by the body, estimated to account for 40-60% of heat loss. ii. Evaporation: moisture is lost via the skin as perspiration, exposed viscera or as exhaled water vapor during to ventilation. A tiny amount of heat is lost via ventilation. This accounts for up to 25% of heat loss in the OR. iii. Conduction: transfer of heat via contact with cooler object, occurs from high concentration to low concentration (entropy). For example, loss to OR tables, sheets, drapes, skin prep fluids, and IV fluids and irrigants. For adults, a small amount of heat loss occurs, but in pediatrics, the loss is significant. iv. Convection: transfer of kinetic energy to air molecules on the surface of the skin, which move to create air currents that are replaced by cooler air molecules. v. Redistribution- The major initial cause of core hypothermia in the first hour. After induction of anesthesia, due to vasodilation there is a large flow of heat from the core to periphery and as a consequence a rapid 1-1.5°C reduction in core temperature. b. How does anesthesia contribute to hypothermia? It induces thermoregulatory impairment. To understand, you have to understand normal thermoregulation which is a three-phase process of afferent thermal sensing (core and peripheral sensors send info up the anterior tract, sensitive to 3 thousandths of a °C), central regulation by the hypothalamus (which receives 80% of input from core body temperature- trunk and deep tissues that make up half of our mass and is nearly homogenous in temp) and efferent behavior and autonomic responses in order to tightly regulate temperature near 37°C. Typically, patients will vasoconstrict to maintain core temperature, then begin to shiver as hypothermia worsens in order to conserve heat. i. But with Anesthesia, several things happen: First, patients enter the OR and lose heat to the environment via radiation and the body is able to vasoconstrict to conserve core heat at this time. Second, you then induce with general anesthetic, which lowers the vasoconstriction threshold to well below body temperature and the thermoregulatory controlled arterial-venous shunts open causing vasodilation. This large flow of heat from the core to the periphery causes a rapid reduction in core temperature of up to 1.5°C. The amount of heat that redistributes is a function o f the core-to-peripheral tissue-temperature gradient, so a larger temperature gradient promotes more loss. So, it’s this redistribution hypothermia that is responsible for hypothermia during the initial hour after induction of anesthesia. Thirdly, as anesthesia continues, changes in core temperature become dependent on peripheral ii. iii. iv. v. heat balance due to loss of autonomic thermoregulation. Humans become what is called poikilothermic. For example, between 34.6-36.9°C there is no vasoconstriction or shivering occurring. Just remember, under anesthesia, patients continue to rely on autonomic efferent responses like shivering, vasoconstriction, and sweating to regulate body temperature, however these responses kick in at different thresholds now. A patient must become sufficiently hypothermic before thermoregulatory vasoconstriction kicks in again, typically re-emerging at 34.5°C. General Anesthetia-reduces vasoconstriction threshold, peripheral vasodilation Opioids-depress voluntary shivering as a mechanism for generation of heat Regional Anesthesia-peripheral vasodilation via sympathectomy Fluid and Blood Administration-Fluid lowers body temp 0.25 °C for every liter administered and refrigerated blood lowers body temp 0.25 °C for every unit. 2. Why do we Care? **PATIENT OUTCOMES. There is significant morbidity associated with hypothermia. The Physiologic Consequences of Hypothermia include: a. Metabolism-postop shivering increasing total body O2 consumption by 400-500%, depletes glycogen and phosphate stores. b. Respiratory-blunted ventilator response to CO2; decreased tissue O2 requirements; left shift in hemoglobin-02 dissociation curve (increases O2 affinity to Hgb thereby decreasing release to the tissues). c. Cardiovascular: Systemic and pulmonary vasoconstriction; increased arterial BP; increased risk for myocardial events (ventricular dysrhythmia, MI, and cardiac morbidity in postop patients) likely due to SNS stimulation and a 100-500% increase in circulating catecholamines. Data shows a decrease in CV events by a factor of three when patients are normothermic. d. Coagulopathy- impaired platelet function (unable to release thromboxane-Step 2/Activation of Platelets) and the coagulation cascade; enhanced fibrinolysis; increased blood loss and transfusion requirements. Temp of 35.6°C: lose 16% more blood and 22% more likely to receive transfusion. e. Immune- increased risk for bacterial wound infections likely due to vasoconstriction which reduces delivery of oxygen and immune cells to the incision site, by impairing functioning of neutrophils and macrophages, and delaying scar formation and wound healing. Data shows a three fold decrease in wound infection risk. f. Prolonged recovery from general anesthesia (JoA), ie. Hypothermia’s effect on the drugs anesthetists administer i. Drug Effects –decreased drug metabolism, increased potency due to decreased temp Prolonged due to increased effect and prolonged duration of neuromuscular blockers. Hypothermic patients exhibit a prolonged duration of action to all muscle relaxants due to decreased metabolism and delayed hepatic and renal clearance. Severe (not mild) hyperthermia makes it more difficult to antagonize a neuromuscular block (Naglehout, p 177). Decreased MAC requirements for inhaled anesthetics (every degree drop in temp (C), the MAC decreases 2-5%). As temp of a liquid decreases, solubility of a gas in that liquid increases and this is why cold patient wakes up slower, the gas is more soluble. Remifentanyl metabolism is decreased by 6% for every drop °C .Fentanyl and Propofol metabolism is also reduced. Clearance of Midazolam is decreased 11% for every °C drop in temp **Quality Improvement Measures in place to prevent Adverse Effects of Hypothermia--SCIP and PQRS measures – include provisions related to perioperative normothermia. Combine process (use of warming techniques deemed effective) and outcome components (core temperature) in surgical patients who receive general or neuraxial anesthesia lasting at least 60 minutes who do not have documented intentional hypothermia. Met by fulfilling any one of the three conditions: 1) active intraop over-body warming; 2) body temp >36 within 30 mins before the end of anesthesia, or 3) body temperature >36 within 15 mins after anesthesia (Sessler). Compliance with SCIP provisions is publically reported and PQRS is linked to an incentivized Medicare payment for those eligible professionals who satisfactorily report data on quality measures (AANA, 2013). 5. Strategies to Maintain Normothermia – Important to understand because how normothermia is maintained is entirely at the provider’s discretion, there is no requirement to use any specific approach for any particular patient in any particular environment. A. Temperature Monitoring: Accuracy and Reliability of Monitoring Sites-SCIP does not indicate which temperature site is the most appropriate to monitor as long as it represents core body temperature. When deciding on which site to use, consider the least invasive modality that will provide reliable and adequate assessment of core body temperature for the duration of the operation. a. Reliable Core Sites- rarely differ from core by more than a few tenths of a degree C. a. Pulmonary Artery via Swan-but not reliable with open chest or rapid changes b. Distal Esophagus- risk of trauma/bleeding, affected by ventilation c. Nasopharynx-risk of trauma/bleeding d. Tympanic Membrane via thermocouple-risk of trauma, decreased by air currents b. Other sites (reasonably estimate core but invasive): Bladder (requires UO) and Rectum c. Skin temperature- well below core (2°C ) and varies among patients, non-invasive B. Approaches to Maintaining Normothermia a. Forced-Air Prewarming- Prevents redistribution by causing preemptive vasodilation of the periphery so that the core-to-periphery gradient is low and heat shifts do not occur upon anesthesia induction. Statistically and clinically significant research showing that prewarming for 30 minutes using a warming unit set at 38°C prevent hypothermia and results in decreased shivering, decreased blood loss, increased thermal comfort, and earlier extubation. b. Forced Air- most common because it’s inexpensive, easy to use, effective, and remarkably safe. Works by decreasing the core-to-periphery temperature gradient so that the rate of heat transfer decreases. Once the peripheral temperature increases above that of the core, then there will be a direct transfer of heat to the core, thus increasing the core. Typically takes 30 minutes or more to show an increase in core temp. Only warming system that has been shown in randomized trials to significantly reduce surgical site infection risk. Recently proposed to disperse bacteria contrary to current research and according to CDC most SSIs are due to endogenous flora of the patient’s skin, mucous membranes, or hollow vicera. c. Airway heating and humidification via HME-ineffective approach to maintaining perioperative normothermia d. Posterior heating with pressure relief materials (perfecTemp, Medline)- Even though a small amount of heat lost via conduction, use of these devices maintain normothermia as well as forced air, even in patients with major open abdominal surgery. e. Passive warming: Cotton blankets, Pre-warm posterior surface of OR table to prevent conduction loses f. Warming fluids-1L at ambient temperature reduces mean-body temp of a 70kg adult by 0.25 degrees C (same as one unit of blood)-unnecessary to warm fluids when small amounts are given (<1l/hr). Shouldn’t be first line because cannot compensate for substantial heal loss from skin surface from within surgical incisions. (sessler) 6. Vulnerable populations a. CAD- Cannot tolerate the physiologic demands and require higher incidence of vasopressors and/or inotropic support, arrhythmias, angina, MIs and mortality due to increased adrenergic response and decreased ability of heart to respond to increased myocardial oxygen demand. b. Geriatrics- Older adults have decreased functioning of the hypothalamus, therefore combined with lower basal metabolic rate, high ratio of surface to body mass, and less effective peripheral vasoconstriction to cold, hypothermia is more pronounced and will last longer because it is harder for the elderly to maintain heat as well as restore it. Hypothermia will further slow anesthetic elimination, recovery from anesthesia, and worsen shivering that leads to hypoxia, acidosis, and cardiac compromise. c. Trauma- Upon admission is associated with a three-fold increase in mortality in adults and double in pediatrics, and severe functional impairment. If aggressively rewarmed, will have lower rate of mortality in first 24 hours. d. Pregnant- Due to shift in O2 delivery curve to the left, decreases blood flow to the uterus and may cause fetal bradycardia. e. Peds- Neonates have a large surface area, poor insulation, and small mass to generate heat. They are unable to shiver therefore sympathetic stimulation of brown fat metabolism occurs to increase heat production. The skin is also thinner, has less subcutaneous fat, and higher rates of evaporative heat loss. To prevent radiant heat, wrap in warm blanket, use radiant heat lamps, cover heat to prevent conductive heat loss (60% from head). Annotated Bibliography Odom-Forren, J. (2013). Post-anesthesia Recovery. In Nagelhout, J.L, & Plaus, K.L (Eds.). Nurse Anesthesia (1224-1243). St. Louis, MO: Elsevier Saunders. The author presents a simple review of heat loss, vulnerable populations at risk for hypothermia development, general anesthetic effects on thermoregulation, adverse effects of hypothermia, and treatment of hypothermia. The benefit of this source is the compilation of general anesthetic effects whereas the other information presented is too brief a review and additional sources are needed to develop a thorough understanding of the hypothermia and thermoregulation. The author does present an thorough algorithm for promotion of normothermia, however, a better approach to prevent post-op hypothermia would be to assess the ways in which to prevent it from occurring in the first place. Roberson, M.C, Dieckmann, L.S., Rodriguez, R.E., & Austin, P.N. (2013). A Review of the Evidence for Active Preoperative Warming of Adults Undergoing General Anesthesia. AANA Journal, 81 (5), 351-356. The authors’ reviewed the evidence examining the efficacy of preoperative warming in patient’s undergoing general anesthesia and found that most of the data is clinically significant and supports implementation of active pre-op warming. The authors discuss the benefits of prewarming including decreased shivering, blood loss, and increased thermal comfort. Conversely, the authors agree that additional research into shorter warming times, lower warming settings, and consistent use of calibrated biometric instruments needs to be performed. The authors’ presentation of pre-warming research is objective and provides strong evidence for it’s use in maintaining perioperative normothermia to prevent adverse thermoregulatory outcomes. Roth, J. V. (2009). Some Unanswered Questions About Temperature Management. Anesthesia & Analgesia, 109(5), 1695-1699. Dr. Roth discusses the relative importance of hypothermia and the use of pre-warming as the only way to mitigate initial redistribution hypothermia. Unfortunately, pre-warming requires resource utilization, is not standard of care, and is not universally used. In addition, the author argues the importance of aggressive warming techniques in short duration cases for quicker PACU recovery, reduction of post-op shivering, and attenuation of adrenergic and metabolic responses to mild hypothermia. The author presents strong knowledgeable arguments that are regarded with interest and can be applied to increase compliance with optimal perioperative temperature management. Sappenfield, J.W., Hong, C.M, & Galvagno, S.M. (2013). Perioperative temperature measurement and management: moving beyond the Surgical Care Improvement Project. Journal of Anesthesiology & Clinical Science, 2, 1-8. The authors provide an in-depth explanation of temperature monitoring intraoperatively, including limitations of common sites for core temperature measurement, disadvantages of different methods for increasing body temperature, the importance of maintaining normothermia due to numerous adverse outcomes, and indications for intraoperative hypothermia in the neuro and cardiovascular populations. In addition they address SCIP measurements and why providers need to look beyond SCIP requirements in order to improve patient outcomes in the perioperative period. This strength in this article lies in is the presentation of limitations in the common sites of temperature monitoring. It is very helpful because providers should choose the most appropriate site for core temperature that is the least invasive but most accurate measurement based on their patient’s presentation and planned operation. Sessler, D.I. (2009). Temperature Regulation and Monitoring. In Miller, R.D., Eriksson, L.I., Fleisher, L.A., Wiener-Kronish, J.P, & Young, W.L. (Eds.). Miller’s Anesthesia (1533-1556). Philadelphia, PA: Churchill Livingstone Elsevier. The hypothalamus receives 80% of input from core body temperature in order to coordinate normal thermoregulatory responses. Patient’s undergoing surgery and general anesthesia experience redistribution hypothermia which drops core temperature up to 1.5 °C and in addition, subsequently have an impaired threshold for response to hypothermia so that when mildly hypothermic they cannot actively respond to thermal perturbations. Although therapeutic hypothermia can provide protection after cardiac arrest, malignant hyperthermia, and neonatal asphyxia, inadvertent hypothermia can produce major adverse effects. Regional anesthesia produces both peripheral and central inhibition of thermoregulatory control and can become as severe as that during general anesthesia. The most reasonable way to prevent thermal disturbances is to monitor core temperature and maintain it above 36°C. Sessler provides a detailed physiologic explanation of normal and impaired thermoregulation that is both relevant and clearly understood by the reader. The author provides strong, objective information that is useful in determining how to prevent the negative effects of hypothermia.