Moore-Pediatric-Surgery-Center-Procedures-and
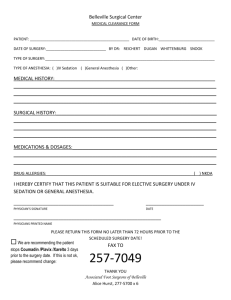
advertisement

[Type text] Moore Pediatric Surgery Center Procedures and Protocols Staffing: Medical Director-Luis Perez Mancilla, MD Chief Pediatrician-Eugenia Vasquez, MD Business AdministratorChief Nurse- Miriam Garcia Director of Operations and Maintenance Book keeper-Mara Morales Social Worker Pharmacy tech/Pharmacist Purpose The purpose of these procedures is to establish standards for the operation of the Moore Pediatric Surgery Center as an out-patient surgical unit in Guatemala City, Guatemala and providing surgical services to pediatric patients. Definitions 1. “Anesthesia service” includes services for all patients who receive general, spinal, regional anesthesia, or monitored anesthesia care. All such patients shall receive a preanesthetic examination, evaluating, planning, and administering anesthesia service required and providing indicated postoperative anesthesia services. 2. “Qualified Anesthetist” means an anesthesiologist or certified registered nurse anesthetist who is licensed to provide anesthesia services either in Guatemala or the United States, approved by the Colegio Medico or similar body in Guatemala, Safely render the patient insensible to pain during the performance of the surgery Monitor and sustain life support functions during the administration of anesthesia Provide pre-anesthesia and post-anesthesia management of the patient Licensure The facility will be licensed according to the laws, rules, and regulations of Guatemala. To this end, the Center has carried out 3 processes: 1) Environmental Impact Study submitted to the Ministry of Environment, 2) Hospital Solid Waste Management Study submitted to the Ministry of Health and 3) License of the facility submitted to the Ministry of Health. Administration The facility shall be operated under a Guatemalan license. There will be an organized functioning governance of the facility to assure accountability. [Type text] The governing body of the facility will hold quarterly meetings and keep a record of the proceedings. Appoint, in writing, a qualified administrator who may be either a separate administrator or the medical director may be the same person. Appoint, in writing, a qualified medical director. Appoint members of the medical staff such as members of the visiting surgical team and Guatemalan practitioners who will be caring for the patients post-operatively. Delineate their privileges based on their qualifications. Administrator An administrator shall be appointed in writing who shall be on site a sufficient number of hours in the business day to manage the facility and to respond to appropriate request by the department. In their absence, they shall designate, in writing, a person to act as administrator in their absence. The administrator will have sufficient power, authority, and freedom to act in the best interests of patient safety and well-being and shall be available at the facility. Qualifications of the administrator will be experience in the administration and supervision of personnel and be knowledgeable about the practice of medicine There will be a general job description of their duties which shall include Compliance with all local laws Develop, evaluate, implement, and update facility policies and procedures annually. Maintain an adequate number of qualified and competent staff to meet the needs of the patients. Follow reporting practices required by the Guatemalan government. Review all incident and accident reports and take appropriate action. Secure through contracts the necessary services not provided directly by the facility. Follow all rules and procedures to maintain a current license in Guatemala. Medical Director. The facility will retain by formal agreement a qualified physician to serve as medical director. The medical director shall be accountable to the governing authority for the quality of services rendered. Qualifications of the medical director: Licensed to practice medicine in Guatemala. [Type text] Have training and expertise in those branches of surgery and anesthesia services offered to provide supervision at the facility. Responsibilities of the Medical Director: Shall have overall responsibility for surgery and anesthesia services provided at the facility. Assist with the creation and updating of facility protocols. Confirm the qualifications of the visiting teams. Coordinate, direct, and evaluate all clinical operations of the facility. Evaluate and recommend the type and amount of equipment needed in the facility. Assure that a qualified physician is available when patients are in the facility. Ensure that physician documentation is recorded immediately and reflects an accurate description of care given. Assure that planned procedures are within the scope of privileges granted to the physicians. Assure that planned procedures are within the scope of the facility. Moore Center Pediatrician The facility will retain by formal agreement a qualified physician to serve as Pediatrician. Qualifications of the Pediatrician: Licensed to practice Medicine in Guatemala Have training and expertise in those branches of Pediatric services offered to all patients of the Moore Pediatric Surgery Center. Responsibilities of the Pediatrician: Shall have overall responsibility for pre and post operative care of the patients operated at the facility. Coordinate all the nurse staff of the facility. Coordinate the work of the Medical Residents of the facility. Ensure proper care of all patients at the ward of the facility Monitor Head Nurse and auxiliary nurse duties Assist with the creation and updating of facility protocols Director of Nursing Services The Moore Center will employ and designate in writing a registered nurse who will be responsible for the supervision and direction of the nursing staff and the operating room suite. Qualifications [Type text] Shall be a registered nurse with a current license and who is qualified by training or education to supervise nursing services. Responsibilities The director of nursing in consultation with the medical director and the pediatrician shall plan and direct the delivery of nursing care. Maintain qualified personnel and supervise them. Assure that a licensed nurse is on duty when patients are in the facility. Maintain the operating room register by her or designate. Write, review, and update nursing policies and procedures. Ensure that nursing documentation is recorded accurately and in a timely fashion. Maintain policies and procedures for pre-operative and post-operative care. Ensure that post-operative instructions are given to the patient or responsible party. Supervise all non-physician direct patient care services. Review identified problems with the medical director. Review policies annually. Visiting Surgical Teams Visiting Surgical Teams will submit to the Moore Pediatric Surgery Center credentials attesting to the medical and para- medical personnel, 2 months prior the Trip’s date. These credentials must be approved by Colegio Medico de Guatemala. Visitors will know policies and procedures of the facility prior every trip and will cooperate with local staff, to give the best medical and surgical care for the patients. Staff and Personnel The facility shall prohibit employees with a communicable disease, open skin lesions, weeping dermatitis or other such conditions from direct contact with patients and patient care items. Comply with Guatemalan health law as it relates to working in such a facility. Participate in training and orientation sessions as organized by the administrator and the medical director and the Chief Pediatrician. Shall be knowledgeable of the policies and procedures of the facility. Quality Assurance The facility administrator, Medical Director, Head Nurse, and Chief Pediatrician shall review the quality of care delivered on a regular basis through a quality assurance program addressing policies, protocols, procedures, incidents reports, medication errors, infection control, patient care and safety. [Type text] Emergency and Disaster The administrator, Medical Director, Chief Pediatrician, and Head Nurse shall develop a plan to address emergency situations and disasters. The plan shall include evacuation plans to a safe place, deliverance of emergency services, specific plans for staff; maintain current emergency contact information for all staff, and policies. A policy specifically addressing fires shall be created. Patient Care Services Each patient shall be under the care of a member of the medical staff or visiting surgical team medical staff. Medical staff shall be credentialed by the policies of the Colegio Medico. All facility staff members shall comply with current laws, facility protocols, and standards as interpreted by the Medical Director. ELECTIVE SURGICAL PROCEDURES PROGRAM 1. - The doctors that will program an elective procedure have to write all patient data in the book designated for that purpose, legibly. The book will be located at the nurse station all time. 2. - The data shall be entered into the computerized system according to the program established for that purpose. Data should include date, time of procedure, patient name, register, age, sex, where it entered service, diagnosis, planned operation, surgeon and assistant. 3. - The operation must be programmed with specific schedule, starting the first operation of each operating room at 7:30 pm. Compute the operating time and the time between surgery and again. Surgeons cannot program any procedure without a specific schedule. 4. - The time stipulated for procedure programming ends at 16:00 5. - Preferably should be scheduled in order of age for surgical patients, and avoid unnecessary fasting for younger patients. GENERAL AND SPECIFIC 1. - In order to schedule elective procedures the physician must verify in advance that the patient has updated its laboratories (less than 6 months validity). 2. - It must verify that the paperwork contains income deposit slip, orders, permission note signed by the patient and responsible family on the anesthesia sheet. 3. - Ensure that the admission sheet is completed correctly by the Admissions Service Personnel. 4. - In the case of operations considered major surgery, patients must have blood compatibility and support. [Type text] 5.-OR personnel will wait a reasonable time the surgeon scheduled 15 minutes. If there is any delay, the surgeon should be notified verbally or by telephone to take action. Not done that way, the Chief Operating Room Head Nurse or may give to cancel the procedure and call the patient that follows, continuing with the established program. 6. - In the case of having emergencies during scheduled elective surgery, must be submitted the case to Chief Operating Room to be him who decides how to schedule surgery and may give such proceedings. All this according to nursing and anesthesia doctors. Is at the discretion of the Head Nurse and Anesthesia doctors to program emergencies. 7. - It is forbidden to schedule patients with false or altered names or data, thus avoiding problems of administrative or legal nature. Neither patients may be substituted or "programmed" by hospitalized patients displayed, if your data does not match the program. 8. - Doctors must respect the program schedule for each specialty according to the respective calendar. 9 .- Be left to the Chief Operating Room any change in the program schedule or order of surgical procedures, and inform the specialists, anesthesiologists and nursing staff of these changes. 10. - It is necessary for each Head of Service to ensure that their patients (elective inpatient and day hospital (are pre-medicated by the anesthesiologist 24 hours before surgery. To this end there is a resident of that pre med anesthesia to patients after 12 hours, every day, in the Department of Pediatric Surgery. 11. - It is prohibited to unauthorized personnel step in the operating rooms. 12. - All staff entering the operating room of Pediatrics should be used "boots" from the red line input. Subsequently, all personnel should wear operating room uniforms (gray, green or blue) and its surgical mask and cap. 13. - It should not to be used in the operating room, jewelry, watch, etc. 14. - It is compulsory to use protective eyewear to operate, the surgeon, the assistant surgeon and scrub nurse. PRE OPERATIVE PROTOCOL: Patients to be considered for out-patient surgery programs must meet the following requirements: 1. - Have a clinical diagnosis of relatively low-risk surgery to resolve. The diagnosis must be verified by the Surgery Center physicians. 2. - Minimum laboratory tests such as hematology, urine, feces. Clotting times will be made to patients with a history of blood illness, or at the discretion of the treating physician. Blood compatibility will be requested in case of anticipated hemorrhage [Type text] 3. - Preoperative pediatric and anesthesiologist evaluation will detect problems like: fevers, coughs, colds, diarrhea, dehydration, anemia, or others. If so, the procedure will be cancelled. 4. - If heart problems are detected, the procedure will be cancelled, and the patient will be referred to local Cardiologist. 5.-Every children who will be discharge the same day of the procedure, must remain locked in a place located not more than an hour away from the hospital. In case of complications, return to the hospital will be easier. Will we not have overnight stays in the facility? 6. - Have completed the paperwork, identification and consent form of surgical procedure signed by the parent or guardian. It added the number of ID or DPI. Parents who cannot read or write can put their fingerprint in the presence of a witness. 7. - Having the corresponding fasting, according to the rules of the American Society of Anesthesiologists. 8. - Take vital signs. The drugs and IV fluids given to patients must be based on body weight. (Kg) 9. - Assess the hygienic condition of the patient to determine the need for a shower before the operation. INTRAORERATIVE PROTOCOL: 1. - Scheduled procedure should last no longer than 90 minutes. Recovery time will be no less than 45 minutes. 2. - Younger patients ideally will be scheduled at the beginning of the surgical day to avoid unnecessary fast. 3. - Intravenous solutions will be placed in the operating room with the patient under sedation. Exceptions to this are a prolonged fasting time. 4. - Photographs can be taken and attached to the clinical record at the surgeon’s desk. 5 .- At the end of the procedure, the patient is transferred to the recovery room, where nurse staff will monitor the patient for a minimum of 45 minutes, and may extend it if the case merits it. 6. - The surgeon and assistants have to fill the operative note and record operating in clear and legible hand writing. Anesthesia sheet should be attached to the paperwork. 7. - As the patient awake, can go to his room where he will be watched closely by the nursing staff of the service. At this time the child may be accompanied by their parents. 8. - Intravenous fluids can be removed until hemodynamic status is stable, and oral intake started. POST OPERATIVE PROTOCOL: [Type text] 1. - After an hour of the patient's recovery, will be provided liquid diet appropriate to their age. Be monitored not have vomiting, or bleeding, fever, pain or any other complication. 2. - Make a final assessment before discharge, which will be supported by the resident doctor on duty, who will sign and stamp the corresponding stationery. 3 .- Recipes will be given to parents or guardians of the patients (and drugs), specifying the name of the patient, drug name, dosage to take, the schedule for giving medication and the name of the treating physician. 4. - Medical staff will give instructions for the healing of wounds and will date and time for postoperative appointment for removal of suture material, if the case warrants it. Educational plan will be given to parents or guardians, related to diet, activity, or other drugs like analgesics and antibiotics. 5 .- If the patient lives far from the Surgery Center or is inside the country, may be given exit and Hospital Staff will get accommodation for 24 hours at the place designated by the authorities of the Centre for that purpose. 6. - Place of final destination after leaving the Center should be considered to provide guidance related to transport. Extended Recovery Services Extended recovery services may be extended to patients that require closer observation. Extended recovery care services shall have policies and procedures that describe the nature and extent of the extended recovery services provided and that are consistent with ambulatory services and anesthesia services. A minimum of two health care workers one of which shall be a registered nurse with ACLS certification shall be on duty. A resident physician may be on site. Nursing Service The facility shall provide nursing services commensurate with the needs of the patients served. All non-medical patient services shall be under the general direction of the director of nursing except as exempted by facility policy. Responsibilities: Nursing service personnel shall be responsible to plan and deliver nursing care, and assist with treatments and procedures. [Type text] All nursing personnel shall have a current license in Guatemala or team nurses should have a current license in the United States. Equipment The facility shall provide equipment in good working order to meet the needs of patients. The type and amount of equipment shall be indicated in facility policy and approved by the medical director. The following equipment shall be available to the operating suite: Emergency call system Cardiac monitor Ventilation support system Defibrillator Suction equipment Equipment for cardiopulmonary resuscitation and airway management Portable oxygen Emergency cart Pharmacy Service The facility will maintain a pharmacy supply under the direction of a pharmacist or pharmacy assistant. The facility will have written policies and procedures to govern the acquisition, storage, and disposal of medications. The quality and appropriateness of medication usage shall be monitored by the medical director. A pharmacy reference manual shall be available to all staff. All medication, solutions, and prescription items shall be kept secure. Drugs shall be accessible only to licensed nursing, pharmacy, and medical personnel. Scheduled drugs will be kept under double lock and key. Records shall be kept as to patient name, drug name, strength, administration documentation, and name and title and time of person administering the drug. Drug disposal will be done according to Guatemalan laws, given through the Ministry of Health. It will be done under supervision of the chief of Pharmacy. Anesthesiology Services [Type text] The facility shall have equipment for the administration of anesthesia service commensurate with the clinical and surgical procedures planned for the facility. Only qualified personnel may administer anesthesia. Qualified anesthesia personnel shall Monitor by continuous presence in the operating room a patient who is undergoing a surgical procedure and who is receiving general, regional or monitored anesthesia care. Continually evaluate a patient’s oxygenation, ventilation, circulation, and temperature. Written anesthesia policies: Preanesthesia evaluation, intraoperative care and record keeping, and postanesthesia care. Needs expansion by anesthesia to suit their needs. Laboratory and Radiology Services The facility shall make provisions for laboratory, radiology, and associated services according to facility policy. The services shall be provided with an order from a physician or a person licensed to prescribe such services. The lab will be a licensed lab as determined by Guatemalan standards. Medical Records A permanent individual medical record shall be maintained for each patient. Records shall conform to good medical and professional practice based on the service provided to the patient. Medical records should contain the following: Admission record (face sheet) that includes the patients name and contact information. A current history and physical exam. Operative reports will contain findings and techniques of the operation. Signed and dated physician orders. Signed and dated nurses notes about the patients care. Laboratory and radiology reports. Pre-anesthesia evaluation. Housekeeping services There shall be housekeeping services to maintain a clean, sanitary, and healthy environment. [Type text] Written housekeeping policies and procedures shall be developed and implemented by the facility and reviewed annually. Laundry Services There shall be laundry services as an outsourcing company. The company offering these services must have experience dealing with hospital services. Dietary The facility will contract a professional company responsible for feeding the patients or at their discretion create a program in house. The company will make available different diets according to patient needs. A nutritionist will be used to deal with adequacy of diets for different patients, ages and needs. Maintenance, Physical Environment, and Safety The facility shall provide a safe and sanitary environment. The administrator shall employ a person qualified to be in charge of facility maintenance or contract for this service. The facility shall develop a written maintenance program to ensure functionality and sanitary practices. When maintenance is performed by an equipment service company, they shall certify that their work is in accordance with acceptable standards. A pest control program shall be developed. Instructional information, cautions, specifications, and operational data on all facility equipment shall be available at all times. Systems-disconnects location information shall be readily available. HVAC systems shall be inspected annually and filters changed regularly. Electrical circuits shall be tested annually. Grounding systems in operating rooms shall be tested monthly and documented. Medical gas systems shall be inspected quarterly. Sterilization units will be tested regularly to assure proper operation Emergency Electric Service The facility purchased an emergency electric plant. It is programmed to start 3 – 5 seconds after any electrical failure. The diesel engine can work more than 14 continuous hours. [Type text] The emergency generator shall be maintained in excellent shape by the facility. The emergency power generator shall be tested weekly and run under load for a period of 30 minutes monthly. Transfer switches and battery operated equipment shall be tested every 14 days. A written record of inspection, performance, test period and repair of the emergency generator shall be maintained at the facility. Storage and Disposal of Garbage, Refuse, and Waste Common garbage will be collected by a local company depending on the facility needs. Medical Solid Waste will be collected by a specialized company. Facility staff dealing with these waste, were properly trained by local authorities. Provisions for Gas Usage Medical gas, air, oxygen and nitrous oxide are available at the facility. Several tanks of these are ready to use at the facility. Several safety valves are located at different points of the pipes. An alarm system is also available at the nurse station. A local company will provide all med gases needed for the trips. Water Supply The facility has two different specialized water filters for drinking water. Water will be available at any time. The facility has two big tanks of water located at the basement, to meet all needs of the facility, including OR’s. [Type text] Operating Room Policies ELECTIVE SURGICAL PROCEDURES PROGRAM THE MOORE PEDIATRIC SURGERY CENTER 1. Cases scheduled shall follow the policies and procedures outlined in the manual describing preoperative evaluation-Sunday. 2. Generally, the center will open for surgery at 7:30 am and close at 4:00 pm. GENERAL AND SPECIFIC 1. - In order to schedule elective procedures the physician must verify in advance that the patient has updated its laboratories (less than 6 months validity). 2. - It must verify that the paperwork contains income deposit slip, orders, permission note signed by the patient and responsible family on the anesthesia sheet. 3. - Ensure that the admission sheet is completed correctly by the Admissions Service Personnel. 4. - In the case of operations considered major surgery, patients must have blood compatibility and support. 5. - Surgeons should arrive on time and the Medical Director or Chief Pediatrician may cancel the case in situations where the surgeon is over 15 (fifteen) minutes late. 6. - The Moore Pediatric Surgery Center performs elective outpatient surgical procedures but in special circumstances with permission from the Medical Director or Head Pediatrician emergency cases may be scheduled. 7. - It is forbidden to schedule patients with false or altered names or data, thus avoiding problems of administrative or legal nature. Neither patients may be substituted or "programmed" by hospitalized patients displayed, if your data does not match the program. 8 .- Any change in the surgical schedule or order of surgical procedures, should be approved by Anesthesia Service, the Chief of the Surgical Team, in consultation with the Medical Director or the Chief Pediatrician. 9. - Only Authorized personnel are allowed in the surgical suites. 10. - All staff entering the operating room should wear appropriate surgical attire. [Type text] 11. Protective eyewear is required of all people in the operative suite This policy is effective from January, 1st, 2011 Dr. Luis Eduardo Pérez Mansilla Medical Director The Moore Pediatric Surgery Center [Type text] MOORE SURGERY PEDIATRIC CENTER PROCEDURES MANUAL Assistant Nurse's Manual of Pediatric Surgery 1. Moore Surgery Pediatric Center will recruit temporary auxiliary nurses to work for 8 days a month or the duration of the scheduled surgery trip. 2. Auxiliary nurses to be hired must submit their curriculum vitae, photocopy of diploma that validates the status, legal and police records, health cards and 2 letters of recommendation. Must undergo a job interview. 3. Nursing assistants (NA) will work in shifts of morning, afternoon or evening. The head nurse will write a roll shift, for the Moore Surgery Pediatric Center. The head nurse will consider the shifts of our personnel working at other institutions to adapt it to our Center. 4. The auxiliary nurse of the Pediatric Surgery ward shall furnish the patient's room and check their function (lights, TV, bathroom, etc). 5. The nursing assistant shall: a) receive the patient in his room, b) to accommodate him and his parents, and direct them to service routines. The child programmed for surgery must be washed with clean pajamas or dressing gown, disposable boots on his feet and if the patient is female, cap on head to cover long hair. 6. The Auxiliary nurse will review that the patient’s file is complete according to the following order: • Admission Sheet of the patient (Overview, diagnosis, suggested procedure, ID number). • Anesthesia Sheet • Recovery Sheet • Vital Sign Sheet • Intake and Output sheet • Medical notes sheet • Medical orders sheet • Medicines Control Sheet • Nursing Note • Authorization procedure (or consent) sheet, signed by the parent or guardian of the patient. [Type text] • Laboratory tests and radiographs. • Reference Notes (who sent the patient to the Center.) 7. Check vital signs. 8. Fulfill Preoperative orders (check fasting, premedication), put pajamas or gown, verify k the name of the patient, and type of surgery, placing the patient on the stretcher and / or wheelchair, provide emotional support to patients and their families, transporting them to operating rooms, deliver the patient to operating room personnel. 9. Receive the patient and follow Surgeons and Anesthesiologists instructions when patient returns from surgery. The patient will be delivered by the nurse in charge of recovery room. The patient will be brought to his (her) room where will be accompanied by their parents or guardians. Orders will be followed during the post operative time, including the processing of his discharge, the return of drugs, if is a day hospital patient. 10. Obey orders given to the patient when admitted. Children should bathe the morning after his surgery (except if it was contraindicated by the type of operation) teaching the mother or caretaker how to manage patient hygiene so that parents can undertake at home (sponge bath, hair only , etc.). * There will be a specific guide to detail the procedure of patient bathing * 11. Process the patient's discharge order, directing parents toward the same, delivering and reviewing drug prescriptions given to them by the surgeon or pediatrician. Request a wheelchair if necessary. MANUAL OF OPERATING ROOMS NURSE ASSISTANT 1. During the surgical workshops or trips, in the area of operating rooms will have 2 nursing assistants assigned by the head nurse as circulating and scrub nurse. Both must have the knowledge to implement and attend in 3 operating rooms. * Scrub Nurse: Assisting the surgeon during a surgical procedure, knowledge of aseptic techniques, name and location of the surgical instruments. * Circulating Nurse: Attend an operative room, stocking supplies, equipment and instruments that are requested by the surgeons. Book of Acts will be written each day which will report specific data: name, age, condition, diagnosis pre-and post-operative, the name of the surgeon and his or assistants, anesthesiologist, scrub nurse. Time of Start and end of surgery. Check in and exit to and recovery of the patient, and all relevant data obtained. [Type text] 2. Operating room nurses will begin their work on Sunday morning helping surgeons and Foreign Staff to fill different operating rooms with surgical materials for the week. Also will wash and sterilize materials for use on Monday. Their work will end on Friday, when last surgeries of the trip are performed. 3. Operating room nurses will have their own stock of: disposable material, gloves, hats, boots etc., Sterile and no sterile equipment: sheets, fields, gauze, bandages, water, etc., Cleaners: clohrexidina, chlorine, surgical soap, etc. 4. Operating room nurses must know: the physical area of the operating rooms and sterilization rooms and preparation of equipment, the handling of the autoclave. Report to Head Nurse when surgery is "septic" and the operating room can no longer be used. She will oversee the cleaning of the operating room until use. A specific protocol addressing cleaning of operating rooms is available at the facility. Trained cleaning personal will clean septic and non septic OR’s. 5. Auxiliary nurses will help to pack the equipment that foreign doctors have used. Sometimes, doctors donate a large number of equipment. Nurses will do an inventory of all donated items. The inventory will be submitted to Head nurse. 6. The work of operating room nurses ends on Friday afternoon. Should be presented again on Sunday, during the following trip, and should ask Head Nurse when will be next trip. Dr. Eugenia Vasquez Coma Chief of Pediatrics Moore Surgery Pediatric Center END [Type text] MOORE PEDIATRIC SURGERY CENTER POLICIES AND PROCEDURES Pre-operative Evaluation-Sunday I. INTRODUCTION The Policy and Procedure Manual will guide the staff and visiting surgical teams through the necessary documentation on the Sunday prior to team’s operative week to insure that the highest level of medical and surgical care is provided to the patients of the Moore Pediatric Surgery Center. II. EFFECTIVE The provisions of this manual shall remain in force until the promotion and publication of a new document replacing the present format and should be reviewed on at least an annual basis or as needs arise to alter them.. This policy is effective from January 1st, 2011. ADMISSION OF PATIENTS Duties of Receptionist: 1 .- The receptionist at The Moore Pediatric Surgery Center will be responsible for receiving the patient's ID card, which identifies him (her) as a patient of the center. 2 .- The receptionist will tell the patient and family to wait in the waiting room until they are called for evaluation. 3 .- The receptionist will be in charge of seeking patient’s file located at the archive of the hospital. 4. The receptionist will collect from each patient the sum of Q 20.00 as a donation. Duties of Intake Nurse 1.- The patient’s file will be received by the collaborator or nurse, making sure to match the ID card. 2 .- The Collaborator or nurse will call the patient by name and surname and a family member to accompany them and lead to a room designated to to be enabled to measure the patient weight and check vital signs such as temperature , pulse, breathing rate and blood pressure. 3.- The data obtained should be written in the clinical record sheet designated for this purpose. 4.- Any abnormality of vital signs will be reported immediately to the Medical Center staff. 5.- An aide or nurse will be responsible for take the patient with his clinical record to the Surgeon Medical Clinic. Designated clinics for surgeons will be located in the main hallway on the first floor. WEIGHT, SIZE AND VITAL SIGNS. PRE OPERATIVE LABORATORY EVALUATION 1 .- In order to schedule elective procedures the physician must verify in advance that the patient has updated its laboratories (less than 3 months validity). 2 .- It must verify that the paperwork contains income deposit slip, orders, permission note signed by the patient and responsible family on the anesthesia sheet.3 .- Ensure that the admission sheet is completed correctly by the Admissions Service Personnel Surgical Evaluation 1 .- The Centre will have three (3) outpatient clinics for evaluation of patients about to undergo surgery. The clinics will be properly identified as # 1, 2 and 3. Each clinic will be equipped [Type text] with non-sterile gloves, flashlights, tongue depressors, ENT Laryngoscope, stethoscope and sphygmomanometer. Each room will be equipped with pens, medical record sheets, stapler, paper clips and other supplies needed to document the patients care. Any other equipment must be requested to the registered nurse or assistant. 2 .- Each clinic will have a translator as an aide to help foreign doctors to communicate with patients and their parents. 3 .- The surgeon will evaluate each patient confirming the correct diagnosis and if the patient is a suitable candidate for surgery and the procedure with its associated risks, benefits and complications will be explained to the parent or guardian. In order to schedule elective procedures the physician must verify in advance that the patient has updated the routine laboratory exams, no older than 3 months. In the case of operations considered major surgery, patients must have blood compatibility and support. 4.- The surgeon should verify that the paperwork contains the informed consent paper signed by parents or tutors. 5 .- A patient selected for surgery will receive a red card complete with the following data: full name, registration, sex, age, weight, diagnosis and planned operation and surgeon's name. The red card will be attached to the medial record. .In addition, the most relevant data of the case will be written in the medical file. 6.- Upon completion of the surgeons evaluation, an aide will take the patient and clinical records for evaluation by the anesthesiologist. 7.- If the patient will not undergo surgery for various reasons such as current illness or other contraindications, the physician will complete the , yellow card indicating the reasons for rejection, and fixed to the outside of the clinical record. On the record, the surgeon will describe the comments relevant to the case. An employee will transfer the patient and family as well as clinical records, to admission desk. The receptionist will assign an outpatient clinic appointment for a later date. 8.- In cases where the surgeon believes that the case is very complicated or too difficult to perform in Guatemala, and may consider transferring the patient to the U.S., for its management, the surgeon will explain to the patient or family that situation. All information has to be written in the clinical record and will be placed a GREEN card on the outside of the clinical record. Other members of the surgical team may evaluate the patient concerning the possibility of transfer. Families will be informed of the teams process for these types of cases and not give false hopes or guarantees of transfer. All such cases will be coordinated by the team thru the staff of the Moore Pediatric Surgery Center. Anesthesia Pre-operative evaluation 1 .- The anesthesiologist will receive the patient with his family, as well as the clinical record. and the RED card. These must include the information collected: full name, registration, sex, weight, and patient age, diagnosis, planned operation, and complete laboratories. 2 .- The anesthesiologist will interview the patient or family members with questions regarding a history of previous illnesses, previous operations, medication use, and allergies. . The record should reflect that there is no fever, respiratory symptoms, or diarrhea and other negatives as determined by anesthesia. Clinical evaluation will include heart and lung function and areas deemed important by anesthesia staff. Anesthetic complications should be discussed and special emphasis place on preoperative fasting and shall be documented. The red card will be retained by anesthesia to collaborate with the surgeon the scheduling of the cases. [Type text] 3 .- In the event that the operation is canceled, the anesthesiologist shall write the respective entry in the patient's clinical record explaining the reasons for the cancellation. In the event of cancellation, the receptionist will assign an appointment for future re-evaluation. 4 .-Upon completion of the anesthesia evaluation, the Center’s Social Worker will interview the patient and family. SOCIAL WORKER INTERVIEW 1 .- The clinical record will reflect the findings of the socio-economic assessment of the patient and family from the initial Center evaluation. 2 .- The Social Worker will know what kind of operation the patient will have and have access to the medical record to be informed of the diagnosis and proposed surgical procedure. 3..- The Social Worker will determine on a sliding scale basis a donation amount to help offset Center expenses and shall not exceed Q. 500.00 and shall be paid prior to discharge of the patient from the Center. 4 .- The Social Worker will help the patient and family on issues related to accommodation and transport for the day of surgery. If necessary, the patient and family will be located in a temporary shelter, previously chosen and designed for that purpose. 5 .- The clinical record shall be returned to Admission to be used later during the days of the trip. SCHEDULE OF OPERATIONS FOR THE WEEK 1 .- Surgeries should follow the policies and procedures outlined in this manual and take into consideration the following information: A) There are three (3) operating rooms B) The first day's proceedings will start at 7:30 AM and the last ones not later than 4:00 PM C) The younger patients should be scheduled at the beginning of the daily schedule to avoid unnecessary fast under consultation with Anesthesia. D) The most complex or time consuming procedures will be scheduled, preferably at the start of the week, to provide adequate follow up, monitoring the patient for several days. 2 .- The surgeons and anesthesiologists will decide the date and time of the surgical procedure, using the red cards. The date and time of the procedure will be listed on this card and then compiled in the Operating Room Programming Book. Entries will be entered in English and translated into Spanish by the Center Interpreter. 3 .- Nursing staff will inform the family and patients of the date and time of the surgery and appropriate fasting verbally and in writing. 4 .- It is forbidden to schedule patients with false or altered names or data, thus avoiding problems of administrative or legal nature. Neither patients may be substituted or "programmed" by hospitalized patients displayed, if your data does not match the program. [Type text] 5.- Any change in schedule or order of surgical procedures should be approved by Anesthesia Service, the Chief of the Surgical Team, in consultation with the Medical Director or the Chief Pediatrician. 6.- In the case of an emergency re-intervention, the surgical program can be changed by The Medical Director in consultation with the Chief of the Surgical team and the Anesthesiologist. 7.- Only authorized personnel are allowed in the surgical suites. 8.- All staff entering the operating room or recovery area should wear appropriate surgical attire. 9.-Protective eyewear is required of all people in the operative suite. Dr. Luis Eduardo Pérez Mancilla Medical Director The Moore Pediatric Surgery Center END [Type text] DISCHARGE CRITERIA FOR DAY SURGERY I. POLICY Day Surgery patients must meet approved discharge criteria in order to be discharged. II. PURPOSE To insure that the patient has returned to a stable condition before allowing patient to return home. III. CRITERIA A. Patient must have clear airway that is patent per self. B. Patient awakens easily and oriented to person, place, and time or has returned to their preanesthetic level of consciousness. C. Vital signs have returned to 20 pts. +/- of preanesthetic levels and patient should be afebrile. Systolic blood pressures 90 or below will be reported to the physician before patient is discharged. D. Patient is able to swallow and has demonstrated ability to drink oral intake or has returned to pre-procedure level of function. E. Patients 7 years and older must be able to void adequately. (Not applicable to IV sedation or if otherwise ordered by physician) F. Has demonstrated capability to use any supportive equipment ordered by the surgeon for care at home. G. Patient and/or family states understanding of post-operative home care; same is documented. H. Patient will be held at least thirty minutes after receiving pain and/or nausea medication before being discharged accompanied by responsible adult. I. Patient receiving anesthesia or IV sedation must be accompanied by a responsible adult upon discharge. J. If any of the above criteria are not met, the physician will be notified for further orders before discharge. K. Patients final destination should not be more than 90 minutes from the facility. [Type text] L. A telephone line must be available for any emergency communication. First line on call is the facility Resident, the Head Pediatrician, The surgeon, The Medical Director. M. A Discharge note must be written in the Medical record by the Resident. The Resident must sign and seal the note. END [Type text] SURGERY POLICY DOCUMENTATION: PERIOPERATIVE NURSING RECORD I. POLICY: A. A Perioperative Nursing Record will be completed by the Circulating R.N. on each surgical case. B. The patient’s record should reflect the perioperative patient’s plan of care, including assessment, diagnosis, outcome identification, planning, implementation and continuous evaluation. C. The patient’s record should specify what nursing interventions were performed and when, where and by whom during each phase of perioperative care. D. Perioperative documentation forms include, but are not limited to, the perioperative record, anesthesia records, nurse’s notes, implant records, laser logs and surgical count sheets. II. PURPOSE: A. To provide guidelines to assist perioperative nurses in the proper and consistent documentation of intraoperative nursing care. B. Perioperative documentation is essential for the continuity of goal-directed care and for the comparison of achieved patient outcomes to expected outcomes. III. PROCEDURE: A. Perioperative nursing record is begun when patient is transported to holding area for surgery. B. The record is to be legible, in black ink, and each section addressed. C. Pre-op diagnosis, operative procedure, and post-op diagnosis must be obtained from physician (written or oral). D. Times in/out for each OR team member must be entered. Each team member must be listed as first name, last name, and title. Wound classification must be identified. E. If implant sheet is used, indicate this under “Implant.” F. Name of person providing ancillary services must be on nurse’s note. G. Any specimen sent to laboratory or pathology must be identified on the record, with identical description used on laboratory or pathology sheet. [Type text] H. When documenting counts, use 1st initial, last name, and title of each person who participated in count. I. On completion of record, the first page is to remain as part of patients’ medical record and yellow copy to return to OR unit secretary. END [Type text] Laboratory and Radiology Services The facility shall make provisions for laboratory, radiology, and associated services according to facility policy.The services shall be provided with an order from a physician or a person licensed to prescribe such services.The lab will a licensed lab as determined by Guatemalan standards. LABORATORY 1. Moore Pediatric Surgery Center initially will subcontract the services of one or two private laboratories, national, with recognized quality, who have knowledge of the welfare work of our institution. 2. Moore Pediatric Surgery Center will use the external services of two national laboratories: 1) Laboratory Bioclinic and 2) the Faculty of Pharmacy of the University of San Carlos de Guatemala, who are committed to provide timely and accurate services and reasonable prices for the various tests that are required . 3. Bioclinic laboratories and the Faculty of Pharmacy at the USAC are near the Moore Center to facilitate the referral of patients and the receipt of test results. 4. Routine Laboratory tests that will be requested to all patients prior surgery are: hemoglobin, hematocrit, clotting time, blood, feces and urine complete. 5. The laboratories are responsible for providing application forms for the various tests. Laboratory orders will be written by medical residents or the head pediatrician, to properly position the patient data: name, ID No., bed, doctor in charge of the order. He/She will mark the test requested. 6. The parents of the patients will be in charge of carrying a child for laboratory tests and collecting the results. Occasionally the laboratory will send the results to the Moore Pediatric Surgery Center. Medical staff will be informed of abnormal test results. TRANSFUSIONS [Type text] 7. When a patient needs a transfusion of blood or blood products, the laboratory will send a technician to take the blood sample for compatibility. The technician will return to the laboratory and process the sample. Then, the blood will be sent to the hospital. Medical staff who can indicate to the patient's family if it is necessary for them to be donors. The laboratory will provide emergency services outside normal working hours. RADIOLOGY 8. Moore Pediatric Surgery Center will outsource radiology services and diagnostic imaging to an external organization. 9. The Moore Center will work with the Radiological Center “Bioclinic” and the Center “RADCO”, the latter for diagnostic studies and non-emergencystudies. Both sites comply with national standards and regulations. 10. When medical staff determine that a radiological examination is necessary and will help to confirm a diagnosis, the patient and their parents will be notified. It will be the responsibility of the family to take the patient to the diagnostic facility.Prices will be reasonable. 11. Radiologic services provided outside the normal working hours must be available in case of emergency tests. Bioclinic radiology center work from 7 am to 18 p.m. (technitian). The radiologist works only during mornings, so that studies and x-rays will be interpreted at that time. 12. External radiology centers providing radiology services and diagnostic imaging to the Moore Pediatric Surgery Center will have an experienced, qualified radiologists who will interpret the studies. 13. The reports of radiological examinations will be collected by parents or guardians of patients unless otherwise specified. In special situations, studies will be delivered directly to the Moore Pediatric Surgery Center from the radiology center through a messenger, in a timely manner, according to patient needs. 14. Given that Moore Pediatric Surgery Center will employ external sources to provide laboratory and radiology services, the Center will develop an alternative approach to monitoring the quality of those services. [Type text] Dr. Eugenia Vasquez Coma Moore Pediatric Surgery Center END RULES OF PREPARATION AND / OR PRESERVING OPERATIVE PARTS (Pathology slides) RESPONSIBLE: Nurse assistant assigned to operating rooms. 1. A Center approved pathologist who will analyze the surgical specimen. 2. The bottle shall be clean,of adequate size, and formaldehyde, alcohol will be placed with the specimen as prescribed by the pathologist or surgeon. 3. Label the bottle with the following data: patient's full name, ID number, date, doctor, name of the piece, name of the pathologist. 4.Complete the pathology form and forward with the specimen to the clinical pathologist. 5. Ask the attending physician or resident physician to fill the form with all data requested. 6. Pathology samples will be stored in the laundry area of instruments. 7. The person designated to carry the sample to the pathology laboratory must sign a book designed for that purpose. END [Type text] Infection Control The aim of the program is to prevent and control infections in the Moore Center. It is designed to identify and reduce risks of contracting and transmitting infections between patients, medical staff, healthcare professionals, contract workers, volunteers and visitors. The staff pediatrician will have the responsibility of trainingpersonnel on the policies and procedures, and coordination among the staff of the Center. HAND HYGIENE Hands should be washed with an alcohol based hand cleanser. (The hands often tolerated better than washing with soap and water.) - Wash hands with soap and water only when visibly dirty. (Too frequent hand washing without a reason, may cause contact dermatitis.) - artificial nails should not be used. - Keep fingernails short and without nail polish. - The use of gloves does not replace the need for hand washing. - The hand sanitizer dispensers must be visible and located at accessible areas of patient care. - Avoid the "filling" of the soap dispensers. This causes pollutionHands should be washed as follows: - Before patient contact - Before an aseptic task - After the risk of exposure to body fluids - After contact with patient - After contact with the patient's environment WATER PURIFICATION - The Moore Pediatric Surgery Center will use purified water in all services utilizing a water treatment system located in the facility and installed by the company Clean Water System (U.S.)utilizing a two micron filter and ultraviolet light. The water source shall be municipal water that will be placed in a cistern on site. Maintainance of the water purification systemCLEANING OF THE HOSPITAL ROOMS [Type text] Clean areas: These rooms are considered to be medium risk areas and will be cleaned as follows - Cleaning personnel will wear rubber gloves utilizing Center approved cleaning agents. The order of cleaning will be as follows: from a clean area to a dirty one, from top to bottom and from the inside out. Techniques to be used are as follows: Do not sweep but pick up dirt with a damp mop. Clean surfaces with damp cloths. Cleaning carts should be left outside of the patient room. -areas with immunosuppressed patients; These rooms should be the first cleaned and follow the same recommendations as above. Isolation (rooms with infected patients) These rooms will be the last rooms cleaned each day to prevent cross contamination. In rooms with isolated patients, cleaning will be done using single-use gloves, then, dispose it before leaving the room. The cleaning material used in isolated rooms must be specific, ideally in a single-use fashion , except the floor. :The cleaning material must be specific to each area. Protocol for Cleaning of Sterile Areas: -General comments on room cleaning: Cleaning staff will have both contract cleaning staff or dedicated personnel of the Center who will be responsible for cleaning the facility as deemed necessary by the Center. .When handling cleaning products, the staff will be protected to prevent possible risks (inhalation or spray on skin and mucous membranes) with individual protective equipment. The operating and recovery areas specifically will be cleaned by Center staff. [Type text] The room cleaning of the Moore Pediatric Surgery Center will be done once a day, and whenever necessary. At the end of each shift, the material used for cleaning must be left clean, sanitized, drained and kept in the space provided for it. There will be a checklist of cleaning services located at different areas of the hospital, that will record the frequency with which cleaning is carried out in different areas. In the data collection sheets will be noted how the area is seen at a glance: clean, or dirty. This observation will be done after cleaning. Supervision of cleaning will be the responsibility the Center Head Nurse. The Infectious Disease committee representative will monitor the cleaning of the facility. In addition to visual observation, microbiological culture of the area will be made periodically ( Chief of Pediatrics will be responsible with the help of an external service laboratory). The usefulness of the microbiological tests will assess the infection control protocol also, with the educational purpose to determine the effectiveness of new products. NOTE: Cleaning of high-risk areas outlined in the cleaning standards of the operating rooms. When a dirty or contamination is found at any place at the hospital, it should be addressed and cleaned as quickly as possibility. The Moore Pediatric Surgery Center will have own cleaning services as well as external ones. The own cleaning staff will be trained to clean the surgical areas, and external staff will be trained to know the current cleaning protocol. For this assessment must be present the person in charge of the hospital cleaning, or an outside cleaning company member and the Head Nurse of the pediatric ward and operating rooms. SKIN PREPARATION Patients should shower or bath with plain soap and antiseptics at least the night before surgery. - At the time of surgery,the area around the incision site must be cleaned before preparation with antiseptic. - The antiseptic should be applied in concentric circles from center to periphery. - Hair surgical site should not be removed (shaved). If necessary the hair is cut very short. - The surgical skin preparation is made with a broad spectrum antiseptic and nontoxic solutions. - Burned or traumatized skin should be prepared with normal saline irrigation, not antiseptic. [Type text] - Soaps and antiseptics that will be used in the Moore Pediatric Surgery Center will be chosen based on objective and updated criteria.. RULES FOR VISITORS • The Moore Pediatric Surgery Center visiting hours for hospitalized children are: • From 10:00 a.m. at 12:30 p.m. • It is NOT allowed more than two visitors per patient in each room. • It is NOT allowed visitors under 10 years of age. • At the door of each room and in hallways, dry alcohol dispensers will be available, so visitors are asked to wash their hands before and after each visit. • Visitors are asked not to sit on patients beds. • Smoking is forbidden at all hospital areas Bringing food from outside the hospital for patients is forbidden Visitors will be informed that the hospital has provided special containers for sharps (needles, razors, etc.). • Visitors will not interfere in the work of health staff: nurses, physicians, support staff, etc. PERSONAL HEALTH Personnel working at the Moore Pediatric Surgery Center should be educated about health and disease, compared to needed care of themselves for being in contact with diseases or exposure thereto, shall identify the risk of infections related to the tasks performed and implement appropriate preventive measures and consider the cost of prevention, to avoid absenteeism and disability - The Moore Center will have a Committee of infectious disease control. This will be organized to conduct research, monitoring and surveillance of potential exposure to infections or outbreaks. This Committee will be formed initially by the Medical Director, Chief of Pediatrics and the Head Nurse. - Moore Pediatric Surgery Center staff will ensure confidentiality of personnel medical records. - There will be an initial medical examination and clinical history for workers in the Moore Pediatric Surgery Center, including immunization status, history of previous illness that may predispose staff to acquired or transmitted diseases. - The vaccination program required for the Moor Center staff will include: Hepatitis B vaccine (3 doses 1-2-6 months), Influenza (1 annual dose) and Tetanus (once in a life [Type text] time or every 10 years). - If an employee of The Moore Center has been exposed to a patient with Hepatitis A or Varicella virus, a vaccine will be administered in a period less than or equal to 72 hours (3 days). - If an employee of The Moore Center had a needle stick injury, from a person that is not vaccinated for HBV carrier, post-exposure prophylaxis will be done with hyperimmune globulin and vaccine. - Pertussis is a disease with high rates of transmission in pediatric areas, any situation should be monitored for possible infection. END [Type text] Moore Pediatric Surgery Center PERIOPERATIVE POLICY ASEPTIC TECHNIQUE: DRAPING A STERILE FIELD I. POLICY: A. Sterile drapes should be used to establish a sterile field. B. Surgical draping materials should provide appropriate barriers to microorganisms, particulate matter and fluids, and should ensure an effective means of protection to patients and perioperative personnel. C. Sterile drapes should resist combustion and should maintain their integrity and durability. D. Sterile drapes should be placed on the patient, furniture and equipment to be included in the sterile field II. PURPOSE:Aseptic practices are implemented to minimize wound contamination. Surgical drapes establish an aseptic barrier that minimizes the passage of microorganisms between non-sterile and sterile areas. III. PROCEDURE: A. The amount, type and size of drapes that are selected for each procedure should be carefully planned. Factors to consider include: 1. Type of procedure 2. Position of patient 3. The amount of area around the incision to be included in the sterile field 4. Furniture and equipment to be draped 5. Cost considerations B. Standard drapes include: 1. Flat sheets used to drape instrument tables and area of the patient. [Type text] 2. Mayo stand covers. 3. Towels used to drape the operative site. 4. Fenestrated drapes with openings of various sizes and configurations to drape specific procedures (ie: abdominal laparotomy, chest/breast, extremity). a. Fenestrations are generally reinforced with an impervious barrier. b. The fenestrated drape is usually large enough to cover the entire patient and operating table with sufficient material to extend over head and foot of the table. 5. Aperture drapes – small fenestrated drapes, usually plastic, frequently used in eye and ear procedures. 6. Equipment drapes – clear, plastic drapes that cover x-ray, microscopic and other equipment. 7. Stockinette drapes used to drape feet and hands. 8. Leggings – part of a drape set intended for surgery with the patient in lithotomy position. C. Only drapes that are intact or have been properly patched are suitable for draping. E. Non-sterile equipment such as the Mayo stand should be covered appropriately with sterile barrier materials before being introduced to, or over a sterile field. F. During the draping process, draping material should be compact, held higher than the operating table and draped from the surgical site to the periphery. G. All draping is done from the appropriate side. Personnel should not lean across a nonsterile area to place sterile drapes. H. During draping, sterile gloves should be protected by cuffing the draping material over hands. [Type text] I. Once the sterile drape is positioned, it should not be moved. Drapes that are incorrectly placed should be removed by a non-sterile person. J. A towel clip that has been positioned through a drape has its points contaminated and must not be removed until the completion of the procedure. K. Surgical equipment, cables and tubing should be secured to the sterile field with nonperforating towel clamps or devices. L. Whenever the sterility of a drape is in doubt, it is considered contaminated and should not be used. END [Type text] Aseptic Technique:Gowning and Gloving Moore Pediatric Surgery Center SURGERY POLICY ASEPTIC TECHNIQUE: GOWNING AND GLOVING I. POLICY: A. Sterile gowns and gloves should be used within the sterile field. B. Surgical hand scrubs should be performed before donning sterile gown and gloves. C. The scrubbed person should don a sterile gown and sterile gloves from a sterile field other than the main instrument table. D. Surgical gowns should provide appropriate barriers to microorganisms, particulate matter and fluids, and should ensure an effective means of protection to patients and perioperative personnel. E. Surgical gowns should resist combustion and should maintain their integrity and durability. F. Extra protection gowns that are coated or laminated with an impervious film should be worn whenever splashes or spraying of blood or other infectious fluids is anticipated. G. Sterile gloves should provide a barrier to prevent the passage of microorganisms from the scrubbed person to the patient and from the patient to the scrubbed person. 1. Gloves should be selected according to the desired strength, durability and compatibility. 2. Scrubbed personnel should inspect gloves for integrity after donning. 3. Extra strength specialty gloves should be worn for procedures where the [Type text] risk of percutaneous blood exposure is high. 4. Wearing two pairs of gloves may be indicated. 5. Sterile gloves should be rinsed or wiped with sterile water or saline prior to the surgical incision in order to remove glove powders that can incite an inflammatory response and delay healing if introduced into the patient. H. Sterile gowns should be considered sterile in front, from the chest to the level of the sterile field, and the sleeves should be considered sterile from two (2) inches above the elbow to the cuff.I. Once the original gloves are donned, the gown cuff should be considered contaminated. J. The preferred method of changing contaminated gloves is for one member of the sterile team to glove the other member. If this is not permissible, the contaminated glove should be changed by the open-glove method. II. PURPOSE:Aseptic practices are implemented to minimize wound contamination. Surgical gowns and gloves should establish a barrier that minimizes the passage of microorganisms between nonsterile and sterile areas. III. PROCEDURE: A. A gown package containing a sterile towel and sterile gown is opened on a small table, separate from the instrument or back table, within the operating room. The gown and towel are packaged so that when it is opened, the towel is on top of the gown. The gown is folded inside out and from bottom to top in such a manner that the top inside portion of the gown is directly beneath the towel. B. After scrubbing, the hands and arms must be thoroughly dried before the gown is donned. If the hands and arms are not thoroughly dried, contamination of the gown may occur by strike-through from organisms contained in moisture on the skin. C. The scrub person grasps the sterile towel and lifts it straight up and away from the gown without dripping water on the gown or sterile field. The scrub person steps away from the sterile field and allows the towel to unfold without contacting the scrub attire. If the towel contacts a non-sterile surface, the towel is considered contaminated and a new one is used. [Type text] D. The top half of the towel is held in one hand while the opposite hand and forearm are team member. 5. Gloves are donned. 6. After gloving is completed, the scrubbed person extends a paper tab, attached to one of the gown ties, to another team member (sterile or nonsterile). The scrub person pivots away from the other team member, causing the gown to wrap around the scrub person. The scrub person then grasps the tie and pulls it, releasing it from the paper tab. The scrub person ties the gown securely in front. (If a tab is not included with the gown, the scrub person may attach a sterile instrument to the end of one tie and hand it to another non-sterile team member who utilizes the instrument in the same manner as the paper tab). G. Closed gloving is a method of donning sterile gloves whereby the scrubbed hands remain inside the gown sleeve until the glove cuff is secured over the gown cuff. 1. Closed gloving is begun with the hands inside the sleeves of the sterile gown. Using the right hand that is still inside the right cuff, the scrub person grasps the left glove by the glove’s everted cuff. 2. The left forearm is extended with the palm facing up and the hand still inside the sleeve. 3. The left glove is then placed palm side down on the upturned left sleeve, palm to palm, thumb to thumb, with the fingers of the glove pointing toward the scrubbed person’s body. 4. Using the left thumb and index finger, the glove cuff is grasped through the stockinette cuff and the glove is held in place. The fingers of the left hand must not extend beyond the stockinette cuff to grasp the glove. 5. With the use of the sleeve-covered right hand, the cuff of the left glove is [Type text] then stretched over the open end of the left sleeve. The glove should totally encompass the stockinette portion of the sleeve. 6. The sleeve covered right hand is then used to exert an even pull on the left sleeve of the gown, causing the left hand to slide into the glove. 7. To glove the right hand, the right glove is grasped with the already gloved left hand and placed on the right sleeve, palm to palm, thumb to thumb, with gloved fingers pointing toward the scrub person’s body. 8. With the use of the right thumb and index finger, the right glove cuff is grasped through the stockinette cuff and held in place. The fingers of the right hand must not extend beyond the stockinette cuff to hold the glove in place. 9. With the gloved hand, the right glove is stretched over the open end of the right sleeve. 10. The left hand is then used to pull lightly and evenly on the right sleeve,causing the right hand to slide into the right glove. H. In the open-glove technique, the scrub person extends the hands through the stockinette cuff of the sleeves when donning the gown. During gloving, the surgically clean hand touches only the inside of the sterile glove and never contacts the exterior of the glove. 1. The gloves are opened by a non-scrubbed person on a clean, dry surface. 2. Using the right hand, the scrub person grasps the everted cuff of the left glove and slides the fingers and thumb of the left hand into the glove, leaving the everted cuff of the glove over the hand and below the cuff of the gown sleeve. 3. The scrub person then slips the fingers of the left gloved hand under the everted cuff of the right glove and slides the fingers and hand into the right glove. [Type text] 4. The everted glove cuff is brought up and over the cuff of the gown. Care is taken to prevent the sterile gloved hand from touching the skin of the wrist or hand. 5. In the final step, the everted cuff of the right glove is brought over the stockinette cuff of the right sleeve. I. Although both the closed and the open-glove techniques are acceptable, the closed-glove technique is preferred. (In the open-glove technique, there is a greater chance of the scrub person’s bare hands contacting the outside of the sterile glove, causing it to become contaminated.) J. After the scrub person has donned a gown and gloves, he or she assists other team members to gown and glove. 1. The scrub person extends a towel to a newly scrubbed person, being careful not to touch that person’s hands. The towel should be presented by placing one end over the outstretched hand of the newly scrubbed person. 2. The scrub person then grasps the folded gown at the neck edge, lifts it away from the sterile field and allows it to unfold. 3. Keeping the hands on the outside of the gown and using the neck and shoulder area of the gown to form a protective cuff over the gloves, the scrub person offers the inside of the gown to the newly scrubbed team member. 4. The newly scrubbed person dons the gown by inserting arms into the sleeves and extending the hands through the stockinette cuff of the gown. 5. A non-sterile team member will secure the gown at the neck and waist area. 6. The scrub person will then glove the newly scrubbed team member. 7. The sterile glove is grasped under the everted edge and held so the thumb [Type text] of the glove is in opposition to the thumb of the person being gloved. 8. The cuff is stretched open wide. 9. The newly gowned person then advances a hand into the glove. 10. The cuff of the glove is stretched high enough and wide enough to cover the stockinette gown cuff completely. 11. The procedure is repeated to glove the other hand. K. If a team member’s glove becomes contaminated, that person steps back from the sterile field and extends the contaminated hand to a non-sterile team member who dons protective gloves and removes the sterile team member’s contaminated glove by grasping the outside of the glove approximately two (2) inches below the top of the glove and pulling the glove off inside out. Care must be taken that the gown cuff not be pulled down or slipped over the hand because the gown cuff is considered contaminated once the original gloves are donned. 1. The scrub person may re-glove the team member in the same manner as previously performed, or the open-glove technique may be used to reglove without assistance. 2. The closed-glove technique is not acceptable for changing a contaminated glove. During initial gowning and gloving, the scrubbed, but not sterile, ungloved hand passes through the gown cuff, causing the cuff to be considered contaminated. In the closed-glove technique, the cuff contacts the sterile glove; therefore, the new sterile glove would be contaminated by the contaminated cuff. L. If a team member’s gown becomes contaminated, a non-sterile team member dons protective gloves and unfastens the gown at the neck and waist, grasps it at the shoulders, and pulls it forward and off over the scrubbed person’s hands, which are still [Type text] glove. The gown should come off inside out. The non-sterile team member then removes the sterile team member’s gloves and the scrub re-gowns and re-gloves the team member. The contaminated gown should always be removed before the gloves are removed. This prevents microorganisms and debris that may be found on the gown from being dragged across unprotected, un-gloved hands. M. At the completion of surgery, the gown and gloves are removed. The gown is removed first. It is grasped near the neck and sleeve and brought forward over the gloved hands, inverting the gloves as it is removed. The gown is folded so the contaminated outside surface is on the inside. It is deposited in a designated receptacle. N. Gloves are removed so that bare skin does not contact the contaminated external glove. 1. The gloved fingers of one hand are placed under the everted glove cuff of the opposite hand and pulled off. 2. The fold on the remaining glove is grasped with the bare finger of the opposite hand and the glove is pulled off. This technique must be performed carefully to prevent bare skin from contacting the contaminated glove surface. 3. Gloves are deposited in a designated waste receptacle. O. After gloves are removed, the hands are washed. Hand-washing lessens the chance of contamination of the hands that may have occurred from an invisible hole or tear in the glove. P. Gown and gloves are not worn outside of the operating room. END [Type text] Rights of patients and Their Family Patient Safety-Ambulatory Health Care 1. Patient Identification-Use at least two patient identifiers when administering medications, blood, collecting samples, or when providing treatments or procedures. 2. Medication Safety-label all medications in the peri-operative and procedural settings as to name, strength, and quantity. Verify all medication or solutions labels both verbally and visually 3. Health care associated infections-comply with the World Health Organization hand hygiene guidelines. 4. Prevention of wrong site, wrong procedure, wrong patient surgery: Conduct a time-out immediately before starting the procedure or making the incision The time-out should be standardized,initated by the OR nurse, it involves all parties of the team and requires concensus, if a team change occurs, the time-out will be conducted again, should include correct patient identity, the correct site, and the procedure to be done, and finally documentation of the time-out. ACCESS TO TREATMENT For every individual must be given fair access to treatment or accommodation or if medically indicated, regardless of their race, creed, sex, nationality or source of payment for treatment. RESPECT AND DIGNITY The patient has the right to receive respectful treatment at all times and under all circumstances, in recognition of personal dignity. PRIVACY AND CONFIDENTIALITY The patient is entitled, according to law, to personal privacy and information, as manifested in the following rights - The right to refuse to talk or see anyone not officially related to the hospital, including visitors or persons officially connected with the hospital but not directly involved in his treatment. - The right to use appropriate personal clothing and other symbolic religious objects, provided they do not interfere with diagnostic procedures or treatment. - The right to be examined in facilities designed to ensure reasonable visual and auditory privacy. This includes the right to request that the hospital have a person of the same sex present during certain parts of a medical examination during the treatment or procedure performed by a professional of the opposite sex and the right not to remain naked for a longer time than necessary to perform the medical procedure for which the patient was asked to undress. - The right to expect that any consultation or reference to his case be made discreetly and there are no people present that are not directly involved in your treatment, without the patients consent. - The right to have your medical record reviewed only by those directly involved in the patient care or by [Type text] others only with the patient’s written authorization, or your legally authorized representative. - To expect that all communications and records related to treatment, including the source of payment, be treated confidentially. - The right to be told of the isolation and protection rules deemed necessary for their personal safety. PERSONAL SAFETY The patient has the right to expect reasonable safety insofar as the practices and hospital facilities permit. The patient has the right that hospital personnel look after his belongings, avoiding theft or loss. IDENTITY The patient has the right to know the identity and professional status of individuals who are providing services as well as the right to know which doctor or health care professional is mainly in charge of his treatment. This includes the patient's right to know if any professional relationship between individuals who are treating him, and the relationship with other health or educational institutions involved in his treatment. The participation of a patient in clinical trial programs or to obtain information for research purposes should be voluntary. INFORMATION The patient has the right to obtain from the professional responsible for the coordination of his treatment, complete and accurate information of diagnosis (as far as it is known), treatment and prognosis. This information should be told to the patient so that he can be expected to understand it. When it is deemed medically not advisable to give this information to patients, such information will be made available to the authorized individual. COMMUNICATION The patient has the right to access to people outside the hospital through visits, verbally and written. When the patient cannot talk or understand the predominant language of the community, should have access to an interpreter. This is particularly important when such language barriers pose a continuing problem. CONSENT The patient has the right to participate reasonably informed in decisions about his health treatment. To the extent possible, this should be based in a clear and concise explanation of patient’s condition and all the technical processes involved, including the possibility of any risk of death or serious reactions, or problems related to their recovery and satisfactory way possible. The patient should not be subject to any procedure without his voluntary consent, competent and sane, or his legally authorized representative. When the patient has significant medical options for treatment, medical staff should also inform the patient. (The Informed Consent process will be defined by the Moore Pediatric Surgery Center.) The patient has the right to know who is responsible for authorizing and performing the procedures or treatment. The patient should be kept informed if the hospital proposes to carry out or undertake human experimentation or other research or educational project that affect his health or treatment. Also, the patient has the right to refuse to participate in such activities. CONSULTATIONS [Type text] The patient has the right to consult a specialist. EVALUATION AND MANAGEMENT OF PAIN The patient has the right to assessment and management of pain. REFUSAL OF TREATMENT The patient may refuse treatment as the law permits. When a patient refuses treatment, the risks should be explained and documented and witnessed by Center staff in the medical record. OTHER The Moore Pediatric Surgery Center supports the patient's right to receive respectful and compassionate care at the end of his life. The Moore Pediatric Surgery Center supports the right of patients to receive and take action on complaints, conflicts and differences of opinion about patient care. The Moore Pediatric Surgery Center will make every effort to protect the patient from physical attacks by the visitors, other patients or staff. This protection is especially important for infants and children, the elderly and people with disabilities or unable to protect themselves, or if they cannot do gestures for help. (This protection goes beyond physical aggression, encompassing other areas of security and protection against abuse, neglect intention, denial of services or assistance in case of fire). "All patients should be informed about their rights so they can understand. END [Type text] Medical Records A permanent individual medical record shall be maintained for each patient. Records shall conform to good medical and professional practice based on the service provided to the patient. Medical records should contain the following: Admission record (face sheet) that includes the patients name and contact information. A current history and physical exam. Operative reports will contain findings and techniques of the operation. Signed and dated physician orders. Signed and dated nurses notes about the patients care. Laboratory and radiology reports. Pre-anesthesia evaluation. MANUAL OF MEDICAL RECORDS 1. Patients referred to the Moore Pediatric Surgery Center by Guatemalan physicians are encouraged to bring a "reference letter", addressed to Dr. Luis Perez M. or to Dr. Eugenia Vásquez. The letter should specify the diagnosis and include any laboratory tests or radiographic studies used in confirming the diagnosis. 2. The reference letter will be received by the admission personnel for the Moore Pediatric Surgery Center and will be made part of the permanent medical record created with a unique identification number. As with all medial records it should contain current address and phone number. **** 3. The admission personnel will make an appointment for the outpatient clinic on Tuesdays and Thursdays from 8:00 am to 4:00 p.m. to be evaluated by Doctors L. Pérez M. and Dr. Vasquez. During this consultation, the patient will be evaluated and additional laboratory tests requested. Imaging studies necessary to support the preoperative diagnosis and surgical treatment will be ordered as necessary. 4. During the evaluation of the patient in the outpatient clinic, Dr. Perez and Dr. Vasquez will inform the parents of the patient that when examined by the American doctors, a translator will be available. During this assessment, a final decision will be made concerning about their surgical case. 5. There is only one medical record per patient. The clinical record shall contain the following paperwork: •. An Admission sheet form (white) contains general patient data: name, age, gender, address, telephone number, name of parents or guardians with their identification number or DPI. This will be completed by hand, by the person responsible for admission. •. A sheet of evolution (blue) containing: Chief complaint, history of illness, history (medical, surgical, trauma, allergy, perinatal, etc.). This sheet will be completed by hand, by the medical staff of the institution. •. A physician order sheet (green) which record the orders, diet, activity, medications, special instructions, etc. (Filled by the medical staff of the institution) [Type text] •. A drug control sheet (light blue), which entered the medication prescribed by doctors, with the timing of dose, route, display, etcand will be completed by nurse who administering themedications. •. Nursing Notes to be completed by nursing staff (white). This sheet will report every patient during every shift. Each note shall be signed by the person who is responsible for the patient. The nursing staff willdocument vital signs, intake and output, and the diet. The nursing staff will also handle the application and return tickets of medicines and equipment, medicines control tickets and the Kardex (light blue ticket that records the patient's name, bed number, treating physician, diagnosis, treatment , diet and directions) This ticket is used to receive and deliver the patients with each shift between nurse staff. •. Dischare against Medical Advise- This sheet will be completed by the Moore Center's medical staff and signed by the parents or guardians of the patient when they request for any reason dischare from the facility without medical clearance. •. Informed Consent. Documentation of informed conscent will provide information to the parents or guardians of the patient concerning the proposed treatment,the benefits or potential complications and possible alternative treatments, the odds of success, potential problems related to recovery and the results of not receiving any treatment. The patient will be informed of the doctor's name that will have the primary responsibility for patient care or are authorized to carry out procedures or treatments. Parents will be given all necessary information to make informed decisions. This document must be signed by parents or guardiansaand the date and time of signing recorded and witnessed. •. A record(blue) which will be the anesthetic protocol, has to be completed by the anesthesiologist responsible for the surgery. This document shall record pre and post operative instructions and document the "pause" or "time out". •. A recovery room notes completed and signed by the recovery nurse from the surgery team every day. (per patient) •. Results of laboratory tests and studies (X rays, CT scans, etc.).. • A protocol will be developed to identify the patient and medical record number. • The records of patients admitted will be placed in the nursing station. Patient information is confidential, so only Guatemalan and team physicians and nurses will have access to this information. If anyone else needing any information must ask permission from the chief of pediatrics. • Upon discharged, residents or teams physicians awill record the discharge medical plan, in addition to the diagnosis and surgical treatment, and postoperative educational plan. This information will be given and explained to the family, including who and when will do post operative care. • Medical records of patients will be stored in a file archive placed in the Admission area. Medical records are legal documents, so it should be kept in order. END [Type text] PROCEDURES FOR PATIENT TRANSFER • The transfer of a patient from the Moore Pediatric Surgery Center to another medical center (Hospital General San Juan de Dios, because of its proximity and contact with the attending physician, the Head of the Department of Pediatrics) will be based on the patient status and the need of specialized health services that were not be available at ourthe Moore Pediatric Surgery Center. The transfer must be approved by the Moore Center Head Pediatricianwho will contact with emergency unit at San Juan de Dios Hospital. Hospital San Juan de Dios. In the absence of the pediatrician, the Medical director or his appointee may make the transfer. • For the transfer of a patient the Center will use the services of an ambulance company's called Health Care at a cost per trip of Q300.00and the Moore Pediatric Surgery Center assume the cost of this service. The patient will be accompanied by a nurse, and if necessary, by a physician of our hospital. The transfer of a patient should be coordinated and approved by the medical director or chief of pediatrics of the Moore Center or their designee in their absence. • Patient transferred will have documentation of the case summary which will include the diagnosis and the treatment of the the patient and the reason for referral.,A copy of alllaboratory tests and x-ray studies will be included. Generally, the transfer of patients will be made only when there is a need for emergency services or intensive care services or treatment that is not available at the Center. • If at any time is not possible to transfer a patient to another medical institution, medical attention will be provided at the Center using medical personnel outside our hospital who can cooperate with us based upon reasonable care and capability of the Center. • Parents or guardians of patients will receive clear instructions about where and how to make the transfer. The instructions include the name and address of the General Hospital San Juan de Dios. The instructions will be given to the [Type text] family both verbally and written and documented that they received such instruction and the reason for the transfer.. • Patient who is transferred may return to the Moore Center upon resolutionof the condition that required special monitoring of their case. END [Type text] POLICY FOR DONATED DRUGS The Surgical program of the Moore Pediatric Surgery Center receives donations ofpharmaceuticals and other medical supplies from companies, medical suppliers, and social organizations and from surgical teams. Purpose-To ensure that these donations are handled in an ethical and professional manner by the authorities of the Moore Pediatric Surgery Center,the warehouse staff and the pharmacy. It is the intent that these donations will be given to patients without cost. • The Moore Pediatric Surgery Center will receive and maintain an inventory of the donated pharmaceuticals, medical supplies, and other donated material and keep an accurate record of their use. The warehouse and the hospital pharmacy receiving these as part of their inventory will maintain an entry and exit record . • The Moore Pediatric Surgery Center will have, within its facilities, a secure storage area and a pharmacy where all medicines and materials will be kept in a safe manner, under appropriate conditions to maintain stability of the products.Contents will be properly labeled as to the material, itsexpiration date and any WARNINGs appropriate to the material or pharmaceutical. • During or after the surgery day, medical foreign and domestic doctorsmay prescribe donated drugs, located in pharmacy, such as analgesics (acetaminophen) and antibiotics to patients who have undergone surgery and / or consider, the need of a medication given by a prescription signed by the physician. These donated drugs will never be sold or used for any other purpose than the unselfish aid to patients. • If a physician prescribes a medication to a hospitalized patient, it must be ordered in the clinical record by writing the name of the drug, the method of administration, the exact dose and schedule. • The nursing staff will be responsible for receiving the donated drugs from the pharmacy, transcribing the written order, then, prepare and administer medications. • If any domestic or foreign physicians need to prescribe a medication to a patient,they will submit a written request to the pharmacy .The patient will receive a receipt documenting the receipt of the medicine. • Non prescriptions medications may be given to the patient. . All other antibiotics or drugs should be prescribed according to specific disease, monitoring its spectrum and side effects. • Donated drugs, located at the pharmacy will be reviewed monthly, after each surgical Trip to check expiration dates. • If a product has expired, will be discarded according to hospital solid waste management protocol. If the medication is a suspension, syrup or powder preparations for reconsitution, it may be disposed of in the toilet. If the medication is a tablets or capsule, it will be discarded in a [Type text] red bag properly identified and be placed in the trash destined for biological waste material. • Empty glass containers of discarded medications will be placed in a cardboard box sealed and identified, and discarded as common garbage. • Expired Medications will be removed from the inventory of Moore Pediatric Surgery Center pharmacy upon their expiration or when notified by the manufacturer or pharmaceutical company. •Donations of psychotropic drugs are not allowed or accepted from foreign because of Guatemalan regulations. END [Type text] SURGERY POLICY ENVIRONMENTAL CLEANING I. POLICY: A. All surgical patients are considered potentially infected with bloodborne pathogens, therefore, the same environmental cleaning protocols should be implemented for all surgical procedures. B. Terminal cleaning is performed daily and on a scheduled basis by Surgery personnel and Environmental Services personnel II. PURPOSE: A. To provide guidelines for environmental cleaning of the Surgical Department. B. To provide a clean environment within the Surgical Department that minimizes patient and employee exposure to potentially infectious microorganisms. III. PROCEDURE: Environmental cleaning measures are required before, during and after each surgical procedure and at the end of each day. A. All horizontal surfaces within the Operating Room (ie: furniture, light, equipment) should be damp dusted with a facility-approved agent and mechanical friction before and after each surgical procedure and at the end of each day. B. A visual inspection should be made for cleanliness before case carts, supplies and instruments are brought into the Operating Room. C. Equipment from areas outside of the Operating Room should be damp dusted with a facility-approved agent before being brought into the Operating Room. D. During surgical procedures, contamination should be confined and contained within the immediate vicinity of the surgical field as much as possible. E. Accidental spills of contaminated debris (ie: blood, tissue, body fluids) in areas outside of the immediate surgical field should be cleaned promptly as possible using a lint-free cloth saturated with a facility-approved agent. F. Contaminated items should be handled using protective barriers. [Type text] G. Contaminated, disposable items used in patient care should be placed in leak-proof containers or tear-resistant, red, biohazard bags to prevent exposure of personnel to items potentially contaminated with infectious microorganisms and to prevent contamination of the surgical environment. H. Contaminated, reusable items should be placed in leak-proof containers to prevent exposure of personnel to blood, tissue and/or body fluids and to prevent contamination of the surgical environment. I. All disposable sharps (ie: needles, scalpels, ESU tips, safety pins) are considered infectious waste and should be placed in special puncture-resistant containers that are labeled as containing biohazardous material. J. Used surgical instruments, basins, trays and other items should be handled only by workers wearing personal protective equipment until decontaminated. K. Floors should be cleaned using a facility-approved agent and a fresh mop after each surgical procedure and at the end of each day. L. Patient transport vehicles, including straps and attachments, should be cleaned with a facility-approved agent after each use. M. Surgical procedure rooms and scrub and utility areas are terminally cleaned daily by Environmental Services. Terminal cleaning includes but is not limited to: i. Surgical lights and external tracks ii. Fixed and ceiling-mounted equipment iii. All furniture and equipment, including wheels and casters – step stools and light switches iv. Hallways and floors v. Handles of cabinets, doors, telephones and push plates vi. Ventilation faceplates vii. Horizontal surfaces (i.e.: tops of counters, sterilizers, fixed shelving) viii. Substerile areas ix. Scrub sinks x. Scrub/utility areas [Type text] N. All areas and equipment in the Surgical Department should be cleaned according to an established schedule, including, but not limited to: i. Ducts and filters ii. Air conditioning equipment iii. Closets, cabinets and shelves iv. Warming cabinets, refrigerators and ice machines v. Walls and ceilings vi. Storage areas vii. Offices, lounges and locker rooms O. Cleaning equipment should be disassembled, cleaned with a facility-approved agent and dried before storage. END [Type text] Counts SURGERY POLICY COUNTS: INSTRUMENT I. POLICY:Instruments should be counted on all procedures where the incision is large enough to permit an instrument to be accidentally retained and in which accurate counts may be achievable II. PURPOSE: A. To provide guidelines to assist personnel in the performance of instrument counts. B. To account for all surgical instruments and ensure that the patient is not injured as a result of a retained foreign body. C. To aid in inventory control and cost containment. III. PROCEDURE: A. Instruments are surgical tools or devices designed to perform a specific function, such as cutting, dissecting, grasping, holding, retracting or suturing. B. Standardized instrument sets are counted in CSR as they are assembled. Preprinted count sheets identical to the standardized set are included in each tray and should be used for documenting counts. C. Instrument counts should be taken: i. Before the procedure to establish a baseline for subsequent counts. ii. When additional instruments are added to the sterile field. iii. Before closure of a cavity within a cavity if applicable and/or before wound closure begins. iv. Before wound closure is complete. v. At the time of permanent relief of the scrub person and /or circulating nurse. vi. When requested by any member of the perioperative team. [Type text] D. Instruments are counted audibly and viewed concurrently by two individuals, one of whom must be a Registered Nurse/Circulator. E. If a counted instrument is passed off, or inadvertently dropped from the sterile field, the circulating nurse should retrieve it, show it to the scrub person and isolate it from the field to be included in the closing counts. F. Particular attention must be given to instruments with multiple parts. Instruments broken or disassembled during a procedure must be accounted for in their entirety by members of the surgical team. G. When only a few instruments are needed from an additional tray, the instruments needed are removed and counted. The rest of the tray should be removed from the operating room. H. Endoscopic instrumentation (e.g. light cords, lenses, trocars) does not need to be counted on laparoscopic cases. i. Instrumentation that may be used on an open procedure must be counted on laparoscopic cases. ii. If a laparoscopic case converts to an open procedure, the endoscopic instrumentation should be isolated. iii. Any subsequent instruments added to the sterile field are counted and documented appropriately. I. Instrument counts should be performed in the same sequence. The count should begin at the surgical site and the immediate surrounding area and proceed to the Mayo stand and back table, then to the instruments that have been removed from the field. J. The results are reported to the surgical team and are documented. If the count is found to be correct, closure will continue. (In the event of a count discrepancy, see “Counts: Discrepancy i. The final instrument count should not be considered complete until those instruments used in closing the wound are removed from the wound and returned to the scrub person. K. All counted instruments must remain in the operating room during the procedure. Waste containers should not be removed form the operating room until all counts are completed and resolved. L. Instrument counts should be documented on the Perioperative nursing Record. Documentation should include: i. Types and number of counts. [Type text] ii. Names and titles of personnel performing the counts. iii. Results of counts. iv. Notification of surgeon. v. Actions taken if count discrepancies occur. (See “Counts” Discrepancy #SUR1010”). vi. Rationale if counts are omitted or not completed. (See “Counts: Waived or Incomplete vii. Any instruments remaining with the patient. Counts:Sharps SURGERY POLICY I. POLICY: Sharps and miscellaneous items with the potential to be retained in the wound or lost should be counted on all procedures. II. PURPOSE: A. To provide guidelines to assist personnel in the performance of sharps counts. B. To account for all sharps and related miscellaneous items and ensure that the patient is not injured as a result of a retained foreign body. III. PROCEDURE: A. Sharps include, but are not limited to, scalpel blades, suture needles, hypodermic needles, cautery blades and needles and safety pins, etc. B. Miscellaneous items include, but are not limited to, vessel loops, umbilical tapes, cautery scratch pads, catheter plugs, etc .C. Sharps counts should be taken: i. Before the procedure to establish a baseline for subsequent counts. ii. When additional sharps or miscellaneous items are added to the sterile field. iii. Prior to the closure of a cavity within a cavity. iv. Before wound closure begins. v. At skin closure or at the end of the procedure. [Type text] vi. At the time of permanent relief of the scrub person and/or circulating nurse. vii. When requested by any member of the perioperative team. D. Sharps and miscellaneous items are counted audibly and viewed concurrently by two individuals, one of whom must be a Registered Nurse Circulator. E. Suture needles should be counted according to the number marked on the outer package and verified by the scrub person when opened. If a package contains an incorrect number of needles, the entire pack should be isolated from the sterile field. i. Empty suture packages should not be used to rectify a discrepancy in a closing needle count. F. Used needles and sharps on the sterile field should be kept in a disposable, puncture-resistant needle container. G. Sharps or other items broken during a procedure must be accounted for in their entirety by members of the surgical team. Note: On occasion, the risk of injury to a patient may be greater if a needle, or a portion of a needle, is retrieved than if it is left to encapsulate in tissue. decision not to retrieve a needle, or portion of a needle, rests with the surgeon. See “Counts: Discrepancy” H. An accurate account of all sharps on the sterile field should be continually maintained by the scrub person. Sharps should be handed to the surgeon on an exchange basis using a “hands free” technique (e.g., sharps basin). I. If a counted sharp is passed off or inadvertently dropped from the sterile field, the circulating nurse should retrieve it, show it to the scrub person and isolate it from the field to be included in the closing counts. J. Sharps counts should be performed in the same sequence each time. The count should begin at the surgical site and the immediate surrounding are and proceed to the Mayo stand and back table and finally to sharps that have been discarded from the field. K. The surgical team is informed of the results of the count. If the count is found to be correct, closure will continue. In the event of a count discrepancy, see “Counts: Discrepancy” L. As skin closure begins, a final count of sharps is conducted in the same manner. The results are reported to the surgical team and are documented. i. The final sharps count should not be considered complete until those sharps used in closing the wound are removed from the wound and returned to the scrub person. [Type text] ii. When multiple procedures are performed on a single patient, sharps from all procedures should be counted together as a single unit. M. All counted sharps and miscellaneous items must remain within the operating room during the procedure. Waste containers should not be removed from the OR until all counts are completed and resolved. N. Contaminated sharps are handled and disposed of in accordance with Gutatemalan Medical Community Policy and hospital policies and procedures. O. Sharps counts should be documented on the Perioperative Nursing Record. Documentation should include: i. Types and number of counts. ii. Names and titles of personnel performing the counts. iii. Results of counts. iv. Notification of surgeon. v. Actions taken if count discrepancies occur. See “Counts: Discrepancy” vi. Rationale if counts are omitted or not completed. See “Counts: Waived or Incomplete” COUNTS: DISCREPANCY I. POLICY: A. In the event there is a discrepancy in the sharps, sponges, or instruments count, proper measures will be initiated to locate item/items. II. PURPOSE: To ensure that the patient is not injured as a result of a retained foreign body. III. PROCEDURE: A. In the event that a discrepancy in the count is identified, the count is repeated. B. The surgeon and surgical team are notified. C. The procedure is suspended (if patient’s condition permits) and a thorough search beginning with the wound and including the operative field, the room and the trash is conducted. D. The Chief of the Surgery team and head nurse for the team is notified. [Type text] E. A lateral view x-ray and an AP view x-ray and any additional views deemed necessary by physician, will be taken (at no charge to the patient) immediately prior to closure of the fascia and again before wound closure, has been completed. F. Information regarding the count discrepancy will be communicated to the Radiologist. The x-ray will be read by a Radiologist with results communicated to the surgeon. The surgeon will review the x-ray to ensure complete capture of the operative area. G. Unless otherwise dictated by the surgeon, if the x-ray reveals a retained sharp, sponge, instrument, or other item, appropriate measures are taken to retrieve it and complete the surgery. H. The count discrepancy, x-ray results and other pertinent information is documented on the Perioperative Nursing Record. I. An incident report is filed END [Type text] Emergency Resustation PERIOPERATIVE POLICY I. POLICY: The purpose is to establish a system for emergency resuscitation notification II. PURPOSE: III. PROCEDURE: END [Type text] ANESTHESIA POLICY EQUIPMENT CLEANING I. INTRODUCTION: It is important to protect the patient from unnecessary exposure to potentially pathogenic organisms originating with the personnel and/or equipment involved in the administration of anesthesia. It is also important to protect personnel from unnecessary exposure to possible infections originating with the patient. II. INFECTION CONTROL PRACTICES: A. Equipment i. Laryngoscope – All laryngoscope handles will be wiped down with germicidal cloths before and after they are used. After use, the blades will be washed with an approved germicide solution and brush. They are then processed utilizing STERRAD for complete sterilization. ii. Soda Lime – Soda Lime canisters are cleaned with Sanicloth plus germicidal cloths, dried, and the Soda Lime changed per manufacturers’ recommendations. Disposable Soda Lime absorbers are used for patients with tuberculosis or gross respiratory infection. When contamination of the Soda Lime absorber is suspected, the Soda Lime is discarded, and the canisters are disinfected with sanicloth plus germicidal cloths and dried. iii. Ventilators – Anesthesia ventilators are washed at regular intervals with Hibiclens scrub brushes, rinsed with clear water, dried, and reassembled. Disposable bacterial filters will be used on the delivery tube of the ventilator. These filters are part of the anesthesia circuit and are replaced after each case. iv. Anesthesia Machines – The anesthesia machines will be cleansed daily with Sanicloth plus germicidal cloths. Preliminary cleaning with soap and water will be carried out if the machine is grossly contaminated. The machine will also be wiped down between cases at room turnover. [Type text] v. Other Non-Disposable Equipment – All of the equipment used by the Anesthesiology Department in the Operating Room is to be cleaned on a regular, prescribed basis, and in addition, anytime it becomes contaminated. Anesthesia carts are washed with germicidal cloths and restocked, rotating supplies. Blood pressure cuffs are cleaned as appropriate. B. Needles and Syringes – All needles and syringes used in anesthesia are of the disposable variety and are discarded in disposal boxes. C. Intravenous Procedure – IVs are started by Anesthesia personnel according to established protocol. D. Spinal and Epidural Trays – Commercially prepared, disposable spinal and epidural trays may be used when received and stored in an appropriate manner. They will not be used if the outer wrapper is perforated or after the expiration date noted on the package. End [Type text] Local Anesthesia:Managing the Patient SURGERY POLICY LOCAL ANESTHESIA: MANAGINGTHE PATIENT I. POLICY:Patients receiving local anesthesia during a procedure should be assessed preoperatively and continually observed during the procedure by an RN. II. PURPOSE:To provide guidelines for RN’s managing patients receiving local infiltration anesthesia only. III. PROCEDURE: A. Preoperatively, the RN reviews the patient’s medical record and interviews the patient. B. Intraoperatively, physiological and psychosocial assessments are performed. i. Heart rate, respiratory rate, and mental status are evaluated. ii. Other types of monitoring (B/P, 02 sat, temperature) can be included. C. The dose, route, and time of all local medication administered should be recorded. D. Other documentation should include, but not be limited to, patient’s responses, all nursing interventions & activities. END [Type text] Standards of Outcome Moore Pediatric Surgery Center STANDARDS OF OUTCOME I. STATEMENT:Patient outcomes are the observable, measurable, physiologic and psychosocial responses to Peri-operative interventions. Standards of outcome provide a framework for measuring patient responses. The achievement of patient outcomes is of primary concern for the surgical department in assessing, planning, implementing and evaluating patient care. II. STANDARDS: A. The patient is free from signs and symptoms of physical injury. B. The patient is free from signs and symptoms of injury due to extraneous objects. C. The patient is free from signs and symptoms of chemical injury. D. The patient is free from signs and symptoms of electrical injury. E. The patient is free from signs and symptoms of injury related to positioning. F. The patient is free from signs and symptoms of laser injury. G. The patient is free from signs and symptoms of radiation injury. H. The patient is free from signs and symptoms of injury related to transfer/transport. I. The patient receives appropriate prescribed medications, safely administered, during the perioperative period. J. The patient is free from signs and symptoms of infection. K. The patient has wound/tissue perfusion consistent with or improved from baseline levels established preoperatively. L. The patient is at, or returning to, normothermia at the conclusion of the intraoperative period. M. The patient’s fluid, electrolyte and acid base balance is consistent with, or improved from, baseline levels established preoperatively. N. The patient’s pulmonary function is consistent with, or improved from, baseline levels established preoperatively. [Type text] O. The patient’s cardiovascular function is consistent with, or improved from, baseline levels established preoperatively. P. The patient demonstrates and/or reports adequate pain control throughout the perioperative period. Q. The patient demonstrates knowledge of expected responses to the operative or other invasive procedure. R. The patient participates in decisions affecting his or her perioperative plan of care. S. The patient’s care is consistent with the perioperative plan of care. T. The patient’s right to privacy is maintained. U. The patient is the recipient of competent and ethical care within legal standards of practice. V. The patient receives consistent and comparable levels of care from all care givers, regardless of the setting. W. The patient’s value system, lifestyle, ethnicity and culture are considered, respected and incorporated in the perioperative plan of care as appropriate. The plan of care reflects the patient’s level of function and ability during the perioperative period. END [Type text] DAY HOSPITAL PROTOCOL GENERAL: One of the most important aspects provided by new surgical and anesthetic techniques, and provides greater patient comfort and for best results is to attain a faster recovery and allow the patient to return home after a brief hospital stay. This has allowed the concept of Day Hospital, in which the patient is admitted the morning of the surgery which can be discharged and return home the same day, bypassing any night in the hospital. Young patients may be accompanied by their parents or relatives and have fun activities for children, such as TVs, videos, games and more. so that children are having fun until the time of surgery. This form of income known as major ambulatory surgery, is offered to patients who are undergoing surgical treatment of low risk. The physician chooses the candidates for this type of income in the outpatient and in accordance with the parents or guardians, provides instructions for preparing the patient for the procedure meets all appropriate safety measures. These include, physical examination, pre-operative fasting time, hygienic measures, schedule of income, and others. . Examples of surgeries that may be considered low risk are among others: inguinal and umbilical hernioplasty, circumcision, orchidopexy unilateral resection of small cysts in different parts of the body, adenoidectomy, placement of ventilation tubes, tympanoplasty, surgery for wisdom teeth dental extractions, dental restoration, etc. Finally, institutional savings by applying this method is considerable and optimize the management of hospital resources and can thus serve a greater number of child population demanding these services. PRE OPERATIVE PROTOCOL: Patients to be considered for out-patient surgery programs must meet the following requirements: 1 .- Have a clinical diagnosis of relatively low-risk surgery to resolve. The diagnosis must be verified by the Surgery Center physicians. 2 .- Minimum laboratory tests such as hematology, urine, feces. Clotting times will be made to patients with a history of blood illness, or at the discretion of the treating physician. Blood compatibility will be requested in case of anticipated hemorrhage 3 .- Preoperative pediatric and anesthesiologist evaluation will detect problems like: fevers, coughs, colds, diarrhea, dehydration, anemia, or others. If so, the procedure will be cancelled. 4 .- If heart problems are detected, the procedure will be cancelled, and the patient will be referred to local Cardiologist. 5 .- Every children who will be discharge the same day of the procedure, must remain locked in a place located not more than an hour away from the hospital. In case of complications, return to the hospital will be easier. [Type text] 6 .- Have completed the paperwork, identification and consent form of surgical procedure signed by the parent or guardian. It added the number of ID or DPI. Parents who can not read or write can put their fingerprint in the presence of a witness. 7 .- Having the corresponding fasting, according to the rules of the American Society of Anesthesiologists. 8 .- Take vital signs. The drugs and iv fluids given to patients must be based on body weight. (kg) 9 .- Assess the hygienic condition of the patient to determine the need for a shower before the operation. INTRAOPERATIVE PROTOCOL: 1 .- Scheduled procedure should last no longer than 90 minutes. Recovery time will be no less than 45 minutes. 2 .- Younger patients ideally will be scheduled at the beginning of the surgical day to avoid unnecessary fast. 3 .- Intravenous solutions will be placed in the operating room with the patient under sedation. Exceptions to this is a prolonged fasting time. 4 .- Photographs can be taken and attached to the clinical record at the surgeons desk. 5 .- At the end of the procedure, the patient is transferred to the recovery room, where nurse staff will monitor the patient for a minimum of 45 minutes, and may extend it if the case merrits it. 6 .- The surgeon and assistants have to fill the operative note and record operating in a clear and legible hand writing. Anesthesia sheet should be attached to the paperwork. 7 .- As the patient awake, can go to his room where he will be watched closely by the nursing staff of the service. At this time the child may be accompanied by their parents. 8.- Intravenous fluids can be removed until hemodynamic status be stable, and oral intake started. POST OPERATIVE PROTOCOL: 1 .- After an hour of the patient's recovery, will be provided liquid diet appropriate to their age. Be monitored not have vomiting, or bleeding, fever, pain or any other complication. 2 .- Make a final assessment before discharge, which will be supported by the resident doctor on duty, who will sign and stamp the corresponding stationery. 3 .- Recipes will be given to parents or guardians of the patients (and drugs), specifying the name of the patient, drug name, dosage to take, the schedule for giving medication and the name of the treating physician. [Type text] 4 .- Medical staff will give instructions for the healing of wounds and will date and time for post-operative appointment for removal of suture material, if the case warrants it. Educational plan will be given to parents or guardians, related to diet, activity, or other drugs like analgesics and antibiotics. 5 .- If the patient lives far from the Surgery Center or is inside the country, may be given exit and Hospital Staff will get accommodation for 24 hours at the place designated by the authorities of the Centre for that purpose. 6 .- Place of final destination after leaving the Center should be considered to provide guidance related to transport. Dr. Luis Eduardo Pérez Mancilla Medical Director The Moore Pediatric Surgery Center END [Type text] Universal Protocol for Moore Center Pre-operative verification process: Verify the correct procedure, for the correct patient, at the correct site Identify the items that must be available for the procedure Relevant documents-History and physical, signed consent form, pre-anesthesia assessment. All diagnostic and radiologic tests available Required implants, devices, or special equipment present. Mark the procedure site: Mark the surgical site when there is more than one possible location for the procedure. Mark the site before the procedure and involve the patient if possible. Mark the site with a sufficiently permanent marker that will be visible after skin preparation and draping. The person marking the procedure should be the licensed practitioner who is accountable for the procedure. It is not necessary to mark mucosal surfaces or perineum or teeth. Perform a time-out The procedure is not started until all question or concerns are resolved. Conduct a time-out immediately before starting the procedure. A designated member of the team starts the time-out. The time-out is standardized. The time-out involves the immediate members of the procedure team: the surgeon, anesthesiologist or anesthetist, circulating nurse, operating room technician. All members of the team must verbally confirm the correct patient, correct area, and correct procedure. If the surgeon changes during the procedure, the same time-out should be conducted again. End [Type text] TITLE: Surgical and/or Invasive Procedure Time Out PURPOSE:To provide a fail-safe check ensuring that all relevant documents and studies are available prior to the start of the procedure and that they have been reviewed and are consistent with each other and with the patient’s expectations and with the team’s understanding of the intended patient, procedure and site. To identify unambiguously the intended site of incision or insertion. To ensure a final verification of the correct patient identity, accurate consent form, procedure to be performed, correct surgical site and side, correct patient position, availability of required implants or special equipment, proper labeling and appropriate display of relevant images and studies, need to administer antibiotics or fluids for irrigation purposes, administration of appropriate antibiotics, and implementation of any other patient safety or procedure specific requirements based upon patient history or medication use. POLICY:The fail-safe check is referred to as a TIME OUT. The TIME OUT is performed immediately prior to the start of all procedures and documented appropriately. When two or more procedures are performed on the same patient and require separate consents (e.g., Cesarean section and tubal ligation) and/or separate teams, a TIME OUT is performed to confirm each procedure before it is initiated. This is not applicable to those situations where the same team is performing multiple components during a single procedure. The TIME OUT is conducted by a designated member of the team and includes interactive, verbal communication between all team members. All team members are free to express concerns about the procedure verification. The procedure is not started until all questions or concerns are resolved. During the TIME OUT, all other activities are suspended to the extent possible without compromising patient safety, in order that all relevant members of the team are focused on the active confirmation of the correct patient, procedure, site, and other critical elements of the TIME OUT. All relevant documents and studies are made available prior to the start of the procedure and are reviewed to ensure consistency with each other and with the patient’s expectations and with the team’s understanding of the intended patient, procedure and site. Missing information or discrepancies must be addressed prior to starting the procedure. The intended procedure site is identified and marked for all procedures involving incision or percutaneous puncture or insertion. Midline, single-organ and endoscopic procedures without intended laterality are exempt. If possible, the procedure site is initially identified and marked before the patient is moved to the location where the procedure will be performed and takes place with the patient (or patient’s representative) involved, awake and aware. To assure unambiguous identification of the site, the correct site is marked YES. The procedure site is marked by a licensed independent practitioner or other provider who is privileged or permitted by the hospital to perform the intended surgical or invasive procedure. This individual will be involved directly in the procedure and will be present during the time the procedure is performed. A surgical marking pen is used to mark the site with exception made in the case of premature infants (<37 weeks gestation) wherein the use of a marking pen may cause permanent tattooing of the skin. The site is marked in a manner which allows the mark to be visible after the patient has been prepped and draped for the procedure. The marking takes into consideration laterality, surface (flexor, extensor), level (spine), and specific digit or lesion to be treated. When the patient refuses to have the site marked and/or in situations when site marking cannot be accomplished (i.e., when it is technically or anatomically [Type text] impossible or impractical to mark the site [e.g., mucosal surfaces]; when patients are tattooed in the area to be marked for site identification; when the patient is a premature infant <37 weeks gestation; when the procedure is an interventional procedure for which the catheter/instrument insertion site is not predetermined [e.g., cardiac catheterization]), the practitioner or provider performing the procedure will be responsible for assuring the correct site isidentified for the intended procedure and will personally verify the site with the team during the TIMEOUT process. POST OPERATIVE PROTOCOL: 1. - After an hour of the patient's recovery, will be provided liquid diet appropriate to their age. Be monitored not have vomiting, or bleeding, fever, pain or any other complication. 2. - Make a final assessment before discharge, which will be supported by the resident doctor on duty, who will sign and stamp the corresponding stationery. 3 .- Recipes will be given to parents or guardians of the patients (and drugs), specifying the name of the patient, drug name, dosage to take, the schedule for giving medication and the name of the treating physician. 4. - Medical staff will give instructions for the healing of wounds and will date and time for postoperative appointment for removal of suture material, if the case warrants it. Educational plan will be given to parents or guardians, related to diet, activity, or other drugs like analgesics and antibiotics. 5 .- If the patient lives far from the Surgery Center or is inside the country, may be given exit and Hospital Staff will get accommodation for 24 hours at the place designated by the authorities of the Centre for that purpose. 6. - Place of final destination after leaving the Center should be considered to provide guidance related to transport. End [Type text] Surgical Site Identification SURGERY POLICY SURGICAL SITE IDENTIFICATION I. POLICY: A. See Hospital Policy: Clinical Care, Surgical and/or Invasive Procedure/Time Out, ADM 2.8. II. PROCEDURE: A. The perioperative RN in the Holding Area will verify patient identity and confirm consistent and correct notation of the surgical site and side in the following manner: i. The patient (or patient’s representative) must verbally confirm identity and procedure including location of the surgical site/side. ii. The patient’s identity will be established with the patient’s identification band as per Hospital Policy, Clinical Care, Patient Identification, ADM 2.7. iii. The following items are reviewed, verified for proper labeling and accurately matched to the patient: 1. Relevant documentation (e.g., history and physical) 2. Procedural consent form(s) 3. Diagnostic and radiologic test results and/or studies 4. Required blood products 5. Procedure as noted on the OR schedule B. Confirmation of the above information will be documented by the perioperative RN in the Perioperative Nursing Record – Holding Area. i. Discrepancies in any of the areas listed above must be resolved before further action is taken. C. When all points of information are consistent, the word “YES” will be written on the patient, slightly above or below the surgical site, by the perioperative RN. Correct site marking will be verified by the surgeon performing the procedure by adding his/her initials to the surgical site. D. Surgical site marking will be performed in the Holding Area prior to the patient being transferred to the OR suite. [Type text] i. The site must be marked in a manner that allows the mark to be visible after the patient has been prepped and draped. ii. The mark will be made with the input of the patient (or patient’s representative) and will be made with a surgical marking pen. iii. The marking takes into consideration laterality, surface (flexor, extensor), level (spine), and specific digit or lesion to be treated. iv. Minimal access procedures intended to treat a lateralized internal organ, whether percutaneous or through a natural orifice are marked on the operative side, slightly above or below the insertion site. v. Midline, single-organ and endoscopic procedures without intended laterality are exempt. vi. For spinal procedures, in addition to preoperative skin marking of the columnar region and side, intraoperative radiographs will be taken to mark exact vertebral level. E. In situations when site marking cannot be accomplished, the surgeon will assume responsibility for assuring the correct site/side is identified for the intended procedure and will personally verify the surgical site/side with the surgical team during the TIME OUT process. This may be applicable during the following situations: i. When patients refuse to have the surgical site marked ii. When it is technically or anatomically impossible or impractical to mark the site (e.g., mucosal surfaces, perineum) iii. When patients are tattooed in the area to be marked for surgical site identification iv. When the patient is an infant <37 weeks gestation wherein the use of a marking pen may cause permanent tattooing of the skin v. When the procedure is an interventional procedure for which the catheter/instrument insertion site is not predetermined (e.g., pacemaker insertion) F. The RN circulator and anesthesia providers will verify patient identity and procedure and confirm consistent and correct notation of the surgical site and side in the same manner as the perioperative RN in the Holding Area. i. The RN circulator will ensure the availability of any implants, devices and/or special equipment required for the procedure before bringing the patient to the operating room. G. The RN circulator will review and confirm (by signature) the documentation provided by the perioperative RN in the Holding Area in the Perioperative Nursing Record – Holding Area. [Type text] H. After the patient enters the OR suite, the RN circulator will conduct a briefing with members of the surgical team and anesthesia personnel which provides: i. Verification of the patient’s identity as established by the patient’s verbal statement (if possible) and with the patient’s identification band a. Upon confirmation of the patient’s identity, a patient label will be placed on the patient in a location that will be notably visible during the TIME OUT (e.g., forehead) ii. Verification of the procedure to be performed as established by the patient’s verbal statement (if possible) and by verification with the procedural consent form iii. Summary of any special equipment, implants, devices, positioning needs, medications, etc. required for the procedure I. Immediately prior to making the incision, a TIME OUT will be taken. During the TIME OUT, the surgical team, anesthesia personnel, and the surgeon will unanimously agree on the following: i. Correct patient identity (using two unique identifiers) ii. Accurate consent form iii. Procedure to be performed iv. Correct surgical site and side with confirmation of site mark visibility following skin prep and sterile draping v. Correct patient position vii. Availability of required implants or special equipment viii. Relevant images and studies properly labeled and appropriately displayed ix. Need to administer antibiotics or fluids for irrigation purposes x. Appropriate antibiotics administered within 60 minutes of the incision xi. Implementation of any additional safety precautions based upon patient history or medication use J. When two or more procedures are performed on the same patient and require separate consents (e.g., Cesarean section and tubal ligation) and/or separate teams, a TIME OUT is performed to confirm each procedure before it is initiated. i. This is not applicable to those situations where the same team is performing multiple components during a single procedure. [Type text] K. Documentation of the TIME OUT and all information verified during the TIME OUT will be recorded on the Perioperative Nursing Record by the RN circulator. END [Type text] Surgical Attire Policy SURGICAL ATTIRE POLICY I. POLICY: A. The Perioperative departments are divided into three (3) areas: i. Restricted: Areas within the Surgery department where surgical procedures are performed and where sterile supplies are stored. ii. Semi-restricted: Peripheral support areas within the Perioperative departments where traffic is limited to authorized personnel and to patients. iii. Unrestricted: Areas within the Perioperative departments with an intermingling of inside and outside traffic, and where street clothes are permitted. B. All persons who enter the restricted and semi-restricted areas of the Perioperative Departments should wear freshly laundered surgical attire. i. If scrubs are worn into the hospital from the outside, they must be changed before entering the restricted areas of the Surgery department in order to minimize the potential for contamination from other environments. ii. All Surgery department personnel exiting the building for any reason must wear a clean lab coat over scrub attire. C. Personnel must keep hair neat, clean, and pulled back. Mustaches and beards must be kept neatly groomed. i. Ornate, or brightly-colored hair accessories or head bands are not appropriate. ii. Head and facial hair, including sideburns and necklines, must be covered when in the restricted areas of the Surgery department. D. Personnel must keep fingernails short, clean and healthy. i. Nail polish, in non-vibrant hues, less than four days old, that is not chipped or excessively worn is acceptable in the restricted and semi-restricted areas of the Perioperative departments. ii. Artificial or acrylic nails may not be worn. E. Cologne and perfume should be avoided in all areas of the Perioperative departments. [Type text] F. All personnel entering the restricted and semi-restricted areas of the Perioperative departments should confine or remove jewelry and watches. i. Small earrings may be worn up to a maximum of two earrings per ear. ii. Jewelry that interferes with, or becomes hazardous to job responsibilities is not permitted. iii. Jewelry worn at the sterile field during surgical procedures must be confined within the scrub attire. iv. Body piercing, tattoos, or other body art must not be visible. G. Name badges must be worn by all personnel at all times. i. Badges should be worn high and neat so customers can see the person’s name and picture. ii. Badges worn at the sterile field during surgical procedures must be confined within the scrub attire. H. Protective barriers should be worn to reduce the risk of exposure to potentially infectious materials. i. All persons entering the restricted areas of the Surgery department must wear a mask when open sterile items and equipment are present. II. PURPOSE: A. To provide guidelines for attire worn within the restricted and semi-restricted areas of the Perioperative departments. B. To promote a high level of cleanliness and hygiene within the perioperative environment. III. PROCEDURES: A. All personnel should enter the Surgery department through the dressing rooms or unrestricted areas and change into proper surgical attire before entering restricted areas. i. Hospital-issued, clean, freshly laundered, two-piece scrub suits made of low-lint, multi-use fabric are provided for use within the restricted areas of the Surgery Department. ii. The top of the scrub suit must be secured at the waist, tucked into the pants, or fit close to the body. iii. A short-sleeved T-shirt may be worn under the scrubs. a. Long-sleeved shirts and/or other clothing that cannot be covered by the surgical scrubs should not be worn. [Type text] iv. Non-scrubbed personnel may wear long-sleeved scrub jackets that are snapped closed during use. v. Perioperative attire is to be changed daily, and/or whenever it becomes visibly soiled or wet by blood, body fluids, sweat or food. a. Surgical attire should be discarded in a designated container after use. b. Surgical attire should not be hung, or placed in a locker for wearing at another time. c. Surgical attire is to be laundered by the hospital-approved laundry facilities. Home laundering is not recommended. B. The first item of apparel donned before entering the restricted areas of the Surgery department should be a clean, low-lint, surgical hat or hood that completely covers and confines all of the hair. i. Disposable headgear should be discarded in a designated receptacle after use. ii. Homemade cloth caps may be worn, but must be made of a fabric that meets hospital standards. Caps must be laundered daily and protected during transport to and from the hospital. iii. Skull caps that fail to cover the side hair above the ears and at the nape of the neck must not be worn. iv. A bald or shaved head must be covered to prevent shedding of squamous cells. v. Surgical hats or caps must either be covered while outside the building or changed prior to entering the restricted area. C. Gloves should be selected and worn depending upon the task to be performed: i. Sterile gloves must be worn when performing sterile procedures. ii. Non-sterile gloves should be worn for other tasks. iii. Gloves must be changed between patient contacts, after contact with contaminated items, or when the task is completed. iv. Hands should be washed after removing gloves. D. Masks worn in the restricted areas of the Perioperative departments must cover the mouth and nose and be secured in a manner than prevents venting. i. Both upper and lower mask strings must be tied securely. [Type text] ii. Use of a double mask is unacceptable as this creates an impediment to breathing and does not increase filtration. iii. Masks should be removed carefully by handling only the ties, then discarded immediately and not left to dangle at the neck. E. Protective eyewear, masks or face shields should be worn whenever activities place personnel at risk for splashing, spraying or splatter. i. Protective eyewear (e.g., goggles, glasses with solid-side shields, chin-length face shields) should be worn in addition to masks. ii. Protective eyewear or face shields that become contaminated should be discarded or decontaminated as promptly as possible. iii. Eye shields should not be worn outside of the departments. F. Additional protective attire (e.g., liquid resistant aprons, extra protection gowns, heavy duty shoe covers) should be worn when exposure to blood or potentially infectious material is anticipated. i. Hands should be washed after removal of masks, eyewear, shoe covers or other protective equipment. ii. If shoe covers are worn, they should be appropriate to the procedure (e.g., waterproof) and changed whenever they become torn, wet or soiled. iii. Shoe covers worn within the Surgery department should be removed before leaving the department. iv. Dedicated shoes used solely within the Surgery department must have clean shoe covers applied prior to leaving the department. G. Shoes and socks (required in all clinical areas) worn within the Perioperative departments must provide protection and should be clean, with no visible soiling. i. In order to minimize the risk of injury, shoes should be water-repellant, with solid uppers, good tread, and enclosed toes and heels. ii. Shoes must meet hospital standards for safety relative to electro-static discharge. END [Type text] INTRAORERATIVE PROTOCOL: 1. - Scheduled procedure should last no longer than 90 minutes. Recovery time will be no less than 45 minutes. 2. - Younger patients ideally will be scheduled at the beginning of the surgical day to avoid unnecessary fast. 3. - Intravenous solutions will be placed in the operating room with the patient under sedation. Exceptions to this are a prolonged fasting time. 4. - Photographs can be taken and attached to the clinical record at the surgeon’s desk. 5 .- At the end of the procedure, the patient is transferred to the recovery room, where nurse staff will monitor the patient for a minimum of 45 minutes, and may extend it if the case merits it. 6. - The surgeon and assistants have to fill the operative note and record operating in clear and legible hand 7. - As the patient awake, can go to his room where he will be watched closely by the nursing staff of the service. At this time the child may be accompanied by their parents. 8. - Intravenous fluids can be removed until hemodynamic status is stable, and oral intake started. END [Type text] Anesthesiology Services. The facility shall have equipment for the administration of anesthesia service commensuratae with the clinical and surgical procedures planned for the facility. Only qualified personnel may administer anesthesia. Qualified anesthesia personnel shall Monitor by continuous presence in the operating room a patient who is undergoing a surgical procedure and who is receiving general, regional or monitored anesthesia care. Continually evaluate a patient’s oxygenation, ventilation, circulation, and temperature. Written anesthesia policies: Preanesthesia evaluation, intraoperative care and record keeping, and postanesthesia care. Needs expansion by anesthesia to suit their needs. RESPONSIBILITIES –ANESTHESIA STAFF I. POLICY: The Anesthesia Team shall be organized under the direction of a chief or lead anesthesiologist, who has overall administrative responsibility for the services provided. A. The Lead Anesthesiologist shall be responsible for the following: 1. Quality of anesthesia care rendered. 2. Enforcement of regulations concerning anesthesia safety. 3. Directing and supervising the activities of the Anesthesia Team 4. Collaborating patient care and equipment needs with the Director of the Perioperative Department. 5. Acting as a Medical Director of PACU. 6. Heading the Anesthesia team. B. The department shall be staffed with qualified anesthesiologists and nurse anesthetists. The CRNA staff will provide anesthesia under the supervision of the anesthesiologists who have [Type text] privileges as approved by the process used by the licensing board in Guatemala for visiting physicians. The anesthesia personnel shall have the competence to: 1. Induce anesthesia. 2. Maintain anesthesia at required levels. 3. Manage untoward reactions. 4. Provide resuscitation care when needed. 5. Provide regional anesthesia (may be administered by either M.D. or CRNA personnel). 6. Emerge patient from anesthesia. D. The anesthesiologist will make care assignments in a collaborative effort with the OR Coordinator in order to manage the OR schedule with maximum efficiency. ANESTHESIA POLICY STANDARDS OF CARE I. POLICY: A. Pre-Operatively An Anesthesiologist shall be responsible for determining the medical status of the patient, developing a plan of anesthesia care and acquainting the patient or responsible adult with the proposed plan. i. The development of an appropriate plan of anesthesia care is based upon: a. Reviewing the medical record. b. Interviewing and examining the patient to: a. Discuss the medical history, preview anesthetic experiences and drug therapy. b. Assess those aspects of the physical condition that might affect decisions regarding perioperative risk and management. [Type text] c. Obtaining and/or reviewing tests and consultations necessary to the conduct of anesthesia. d. Determining the appropriate prescription of preoperative medications as necessary to the conduct of anesthesia. ii. The responsible anesthesiologist will verify that the above has been properly performed and documented in the patient’s record. iii. The patient shall be re-evaluated immediately before anesthesia induction. B. Intraoperatively i. Qualified anesthesia personnel shall be present in the room throughout the conduct of all general anesthetics, regional anesthetics and monitored anesthesia care. ii. During all anesthetics, the patient’s oxygenation, ventilation, circulation and temperature shall be continually evaluated. C. Post-Anesthesia Care i. All patients who have received general anesthesia, regional anesthesia or monitored anesthesia care shall receive appropriate post anesthesia management. a. A Post-Anesthesia Care Unit (PACU), or an area which provides equivalent postanesthesia care, shall be available to receive patients after anesthesia care. All patients who receive anesthesia care shall be admitted to the PACU, or it’s equivalent, except by specific order of the anesthesiologist responsible for the patient’s care. ii. A patient transported to the PACU shall be accompanied by a member of the anesthesia care team who is knowledgeable about the patient’s condition. The patient shall be continually evaluated and treated during the transport with monitoring and the support appropriate to the patient’s condition. [Type text] iii. Upon arrival in the PACU, the patient shall be re-evaluated and a verbal report provided to the responsible PACU nurse by the member of the anesthesia care team who accompanies the patient. a. The patient’s status on arrival in the PACU is documented. b. Information concerning the preoperative condition and the surgical/anesthetic course is transmitted to the PACU nurse. c. The member of the Anesthesia Care Team will remain in the PACU until the PACU nurse accepts responsibility for the nursing care of the patient. iv. The patient’s condition shall be evaluated continually in the PACU. a. The patient is observed and monitored by methods appropriate to the patient’s medical condition. Particular attention should be given to monitoring oxygenation, ventilation, circulation and temperature. During recovery from all anesthetics, a quantitative method of assessing oxygenation, such as pulse oximetry, is employed in the initial phase of recovery. b. An accurate written report of the PACU period shall be maintained. An appropriate PACU scoring system is used on admission, at appropriate intervals prior to discharge and at the time of discharge. c. General medical supervision and coordination of patient care in the PACU is the responsibility of an anesthesiologist. d. There shall be a policy to assure the availability of a physician in the facility that is capable of managing complications and providing cardiopulmonary resuscitation for patients in the PACU. v. A Physician is responsible for the discharge of the patient from the PACU. [Type text] a. When discharge criteria are used, they must be approved by the Department of anesthesia staff. They may vary depending upon whether the patient is discharged to a hospital room or to a short stay unit, or home. b. In the absence of the physician responsible for the discharge, the PACU nurse shall determine that the patient meets the discharge criteria. The name of the physician accepting responsibility for discharge shall be noted on the record. vi. Upon the discretion of the anesthesiologist/anesthetist and the surgeon, a surgical patient may return directly to the floor. The circulating nurse will call a report to the floor beforesending the patient. The OR record will reflect that the patient was transported to PatientRoom. Anesthesia will make a note that they are discharging the patient to their room. vii. Documentation: The following information shall be documented by the anesthesia personnel on all anesthetized patients: a. Pre-operative visits. b. A set of VS immediately before induction. c. All events taking place during the induction of, maintenance of, and emergence from anesthesia, including dosage and duration of all anesthetic agents, other drugs, intravenous fluids, blood and blood fractions. d. Condition of the patient at the end of the surgery. END [Type text] POLICY FOR RESIDENTS THE MOORE PEDIATRIC SURGERY CENTER Year 2.011 GENERAL RULES OPENING TIME: The entire group of surgical residents rotating through the pediatric surgery service should initiate activities at 7:00 am Mondays to Fridays and at 8:00 a.m. Saturdays, Sundays and holidays. SHIFTS: The shifts are delivered at 7:00 a.m. Monday to Friday, Saturday, Sunday and holidays are delivered at 8:00 am and receive the shift at 15:00 hrs. Monday to Friday, Saturday, Sunday and holidays will be received at 8:00 am The Surgical Day weeks, residents should continue its work until the end of Day. PERSONAL APPEARANCE: All residents should care about its image, must be presented clean shaven with clean uniform, clean shoes with his white coat and having ID card. PATIENT CARE: Patients should be assessed daily, observing the clinical course, complications, new data and taking appropriate action for each particular case and notify physician and Head Pediatrician. VISITING ROOMS AND PATIENTS: The group of residents should check the day's surgical program, assess that patients have attended the Centre and are in good condition for surgery. Then go check out for the patient and write a comment or orders on the patient charts. One resident must be submitted to the operating room to assist as necessary. Participate in the proceedings, make operative records and post operative check orders. General visits (residents and department heads) are held on Mondays, Wednesdays and Fridays at 9:00 am During which the resident must submit the cases for surgery and consultations have been carried out by Specialist physicians should be well informed of the case patients, the clinical and relevant laboratory tests. NOTES AND COMMENTS: [Type text] At the start of daily activities, residents will evaluate each patient comprehensively observing general, surgical, new laboratory tests, etc. then make your notes and orders which should be clear, detailing new and important aspects of each case and its evolution, in the end you must enter a comment clear and concise statement of the case, if you have any questions you can expect to have a round with head nurse and pediatrician to make the relevant comments. Any medical note has to be signed and sealed by the resident who has done the same, just as at the end of the general inspection or the report of a case or department heads, should be noted in the comment indicated by the behavior or department heads. OUT PATIENT CLINIC The outpatient pediatric surgery have special programming. The resident should assist the patients' physical examination, laboratory review, diagnosis and possible programming for the Day. We have split the general surgery outpatient clinic in day hospital, clinic of otolaryngology, urology clinic, clinical neurosurgery, plastic surgery, orthopedic clinic, and dental clinic. The entries in the record must be clear and indicate diagnosis, treatment and conduct to follow, likewise, should be recorded in the header, the doctors name who evaluated the patient, date, time, and the seal of the resident or doctor at the end of the note. OPERATING ROOM: The Moore Center have 3 operating rooms (A, B and C) which are allocated to different operations depending on the specialty that comes in the Trip. All procedures must be scheduled in the book room on the computer operations and service (Excel) before 13:00 hrs. filling the requested data. Pediatric surgery programs begin at 7:30 am In case of emergency surgeries, has to be recorded in the book located at the operating room and be informed about the surgery to the Surgeon head of operations room, the Head nurse manager operating room and anesthesiologist in charge at that time The day of surgery, residents allocated to each operating room shall be within the operating room at 7:15 am sharp, and then, ask the recovery room nurse to call the first patient scheduled to begin at 7:30 am OPERATIVE RECORD: All residents must perform the operative record of the surgery that were present. This record should be written in a clear and legible hand writing , and completed immediately after surgery. In special cases of neonatal surgery and general surgery, the operative [Type text] record should be made on the computer and print it , adding a sketch or drawing of the surgery performed and 2 photographs of the surgical procedure by placing on record and leaving recorded in the computer room operations. SPECIFIC RULES RESIDENTS From the Group of residents working in the MOORE PEDIATRIC SURGERY CENTER, one of them will have the highest rank and is responsible for everything that happens in the workplace. Chosen by the Director and Chief of Pediatrics, must report any situation of importance in the Service and Operating Room. 1. Ensure the timeliness of their group in charge. 2. Will be responsible for leading the round with the group of residents, prior to the filing of cases in the general inspection, and to take appropriate curse of action over time as the need arises. 3. Must meet each of the patients who are in the service and patients post surgery requiring attention from pediatric surgery in different areas of specific care center, as well as patients operated on for different post. . 4. You will be responsible for the evaluation of patients post surgery or cures warrant, remove points, etc. Will consult relevant specialists to take a good post-operative. 5. Will ensure that the operating room schedule this done before 13:00 hrs. recorded in the book of operating room designated for this purpose and in the operating room computer (Excel). 6. 7. Will be responsible for presenting to the head of the cases that warrant further attention (surgery) for general tours or during shifts. 8. You will be responsible for the preparation and presentation of interesting case when required. 9. Must submit monthly statistics to end the time of its rotation in the Moore Pediatric Surgery Center, including a copy to the head of service and management, as well as a CD containing photographs of major surgeries during the month. 10. Abide by the orders given by their department heads. 11. The resident on duty must go and visit every day a round between 19:00 and 20:00 hrs. the post surgery patients .. Present telephone call to the chief and department head cases assessed during the visit and the changes on patients. 12. Must submit the After-hours surgical cases to the head Pediatrician for deciding course of action. 13. Attending graduate school at 15:00 hrs. [Type text] Dr. Luis Eduardo Pérez Mancilla Medical Director THE MOORE PEDIATRIC SURGERY CENTER END [Type text] ANESTHESIOLOGISTS MANUAL 1. On Sunday during the pre operative evaluations, the anesthesiologist will evaluate the potential surgical patient to investigate his background and current health status. If everything is normal, the patient may be scheduled FOR SURGERY. 2. The anesthesiologist should foresee, beside the surgeon, the possibility of intraoperative bleeding according to the degree of complexity of the surgical procedure, so the anesthesiologist will be responsible for requesting, before surgery, blood group compatibility and the patient and transfusion (whole blood, packed cells, plasma, etc..) when the surgeon requested. 3. On Monday, prior to start any surgery, the anesthesiologist has to devote some time and space (pre-operative area) identify himself with the patient and his parents. Should explain in a clear way(accompanied by a translator) the anesthesia procedure, the time taken for surgery, prior fasting necessary, reasonable risks of anesthesia and its responsibility in monitoring the recovery of the patient. The anesthesiologist has the option to cancel a procedure if necessary. 4. The anesthesiologist will work in a restricted traffic area (green), so that he can not leave the area without having changed his clothes, except those permitted areas: a) recovery area, b) rest room and c) locker room. To exit the green area all personnel must wear a coat, take off boots and hat, and put a new disposable when to re-enter the sterile area. If any of the staff were walking outside these areas must remove the operating room clothing. 5. The anesthesiologist will receive the surgical patient that comes from the surgical ward from the nurse. When the surgery finishes, the anesthesiologist return the patient to recovery room personnel. Post operative medical orders given by the surgeon or anesthesiologist must precise information about the diet, activity, intravenous fluids, analgesics, antibiotics, etc. Should indicate when the patient is able to be transferred to his room. 6. The anesthesiologist will manage and fill the document called Protocol of Anesthesia, with pre and post operative data, signing of responsibility for what it is detailed. The anesthesiologist must perform a universal protocol for prevention of erroneous interventions and surgical procedures, before any procedure. (3 minutes). The pause must be written on the patient’s record. END [Type text] PROCEDURES MANUAL MANUAL FOR THE RECOVERY AREA (Nurses Recovery) 1. The recovery area, next to the operating room, will be managed by nurses of the surgical team during the trip or journey. 2. The recovery nurses will be in the operating room (green area ), dressed in clothing typical of the surgical area, where they will have room to handle 5 patients simultaneously. May leave the operating room, the recovery area, the break area and the lockers rooms wearing clothing of OR. Upon leaving the restricted areas for lunch, all personnel should wear a gown and remove disposable boots and hat. All staff must wear new boots, mask and gown to re-enter the sterile area. 3. The recovery nurse will receive the post op patient, as well as the anesthesiologist indications .including intravenous fluids, analgesics or other. The recovery area must provide all equipment necessary for full recovery of the patient: a stretcher, monitors, oxygen masks with appropriate reservoir size for the patient age, quilts, IV solutions, analgesics, disposable syringes, splints, cures. IV solutions, analgesics, etc. 4. The recovery nurse will have strict control of liquids intake received by the patient (ORAL or IV) and the excreta (urine, feces, vomit). These data should be recorded and reported in a sheet designed for that purpose. 5. The recovery nurse will monitor the full recovery of postoperative patients and their stability by monitoring and recording of vital signs (blood pressure, pulse, respiration, oxygen saturation), state of consciousness, skin color, etc. She will Indicate when and how the post op patient may leave the recovery area and be transferred to the appropriate area (bed rest, critical area), transporting the patients by arms, stretcher or wheelchair. Patients will be evaluated also by the Moore Center resident physicians to confirm the transfer of patients to their rooms. 6. Once the post op patient is fully recovered, the recovery area nursing staff will call the auxiliary nursing staff of the surgical ward to pick up the patient. 7. If the patient has any complications or medical problems resulting from surgery, should be evaluated by the hospital's chief pediatrician, who will decide the most appropriate actions to take. END [Type text] ANESTHESIA POLICY STANDARDS OF CARE I. POLICY: A. Pre-Operatively An Anesthesiologist shall be responsible for determining the medical status of the patient, developing a plan of anesthesia care and acquainting the patient or responsible adult with the proposed plan. i. The development of an appropriate plan of anesthesia care is based upon: a. Reviewing the medical record. b. Interviewing and examining the patient to: a. Discuss the medical history, preview anesthetic experiences and drug therapy. b. Assess those aspects of the physical condition that might affect decisions regarding perioperative risk and management. c. Obtaining and/or reviewing tests and consultations necessary to the conduct of anesthesia. d. Determining the appropriate prescription of preoperative medications as necessary to the conduct of anesthesia. ii. The responsible anesthesiologist will verify that the above has been properly performed and documented in the patient’s record. iii. The patient shall be re-evaluated immediately before anesthesia induction. B. Intraoperatively i. Qualified anesthesia personnel shall be present in the room throughout the conduct of all general anesthetics, regional anesthetics and monitored anesthesia care. ii. During all anesthetics, the patient’s oxygenation, ventilation, circulation and temperature shall be continually evaluated. C. Post-Anesthesia Care [Type text] i. All patients who have received general anesthesia, regional anesthesia or monitored anesthesia care shall receive appropriate post anesthesia management. a. A Post-Anesthesia Care Unit (PACU), or an area which provides equivalent postanesthesia care, shall be available to receive patients after anesthesia care. All patients who receive anesthesia care shall be admitted to the PACU, or it’s equivalent, except by specific order of the anesthesiologist responsible for the patient’s care. ii. A patient transported to the PACU shall be accompanied by a member of the anesthesia care team who is knowledgeable about the patient’s condition. The patient shall be continually evaluated and treated during the transport with monitoring and the support appropriate to the patient’s condition. iii. Upon arrival in the PACU, the patient shall be re-evaluated and a verbal report provided to the responsible PACU nurse by the member of the anesthesia care team who accompanies the patient. a. The patient’s status on arrival in the PACU is documented. b. Information concerning the preoperative condition and the surgical/anesthetic course is transmitted to the PACU nurse. c. The member of the Anesthesia Care Team will remain in the PACU until the PACU nurse accepts responsibility for the nursing care of the patient. iv. The patient’s condition shall be evaluated continually in the PACU. a. The patient is observed and monitored by methods appropriate to the patient’s medical condition. Particular attention should be given to monitoring oxygenation, ventilation, circulation and temperature. During recovery from all anesthetics, a quantitative method of assessing oxygenation, such as pulse oximetry, is employed in the initial phase of recovery. b. An accurate written report of the PACU period shall be maintained. An appropriate PACU scoring system is used on admission, at appropriate intervals [Type text] prior to discharge and at the time of discharge. c. General medical supervision and coordination of patient care in the PACU is the responsibility of an anesthesiologist. d. There shall be a policy to assure the availability of a physician in the facility that is capable of managing complications and providing cardiopulmonary resuscitation for patients in the PACU. v. A Physician is responsible for the discharge of the patient from the PACU. a. When discharge criteria are used, they must be approved by the Department of anesthesia staff. They may vary depending upon whether the patient is discharged to a hospital room or to a short stay unit, or home. b. In the absence of the physician responsible for the discharge, the PACU nurse shall determine that the patient meets the discharge criteria. The name of the physician accepting responsibility for discharge shall be noted on the record. vi. Upon the discretion of the anesthesiologist/anesthetist and the surgeon, a surgical patient may return directly to the floor. The circulating nurse will call a report to the floor before sending the patient. The OR record will reflect that the patient was transported to Patient Room. Anesthesia will make a note that they are discharging the patient to their room. vii. Documentation: The following information shall be documented by the anesthesia personnel on all anesthetized patients: a. Pre-operative visits. b. A set of VS immediately before induction. c. All events taking place during the induction of, maintenance of, and emergence from anesthesia, including dosage and duration of all anesthetic agents, other drugs, intravenous fluids, blood and blood fractions. d. Condition of the patient at the end of the surgery. [Type text] END [Type text] PACU Policy:Admission of Patient PACU POLICY ADMISSION OF PATIENT I. POLICY: Patients receiving anesthesia are admitted to the PACU immediately after surgery. If indicated, patients receiving local IV sedation may be admitted to the PACU for a period of observation. At the discretion of the Surgeon/Anesthesiologist, any patient whose post-operative condition is critical, who requires assisted ventilation, or who needs specialized intensive care monitoring, may be transferred to the CCU immediate post-op. II. PURPOSE: Post-anesthetic evaluation, observation, and treatment is mandatory in order to assure the patient is recovering from anesthesia and is in stable condition prior to transfer to the nursing unit. With diligent, specialized nursing care, such potentially hazardous complications such as vomiting with aspiration, hemorrhage, shock, airway obstruction, and respiratory or cardiac arrest may often be prevented or at least successfully treated. III. PROCEDURE: Upon admission of the patient to PACU, the following conditions will be assessed and necessary procedures followed: 1. Assess and record patency of airway. a. Establish adequate ventilation as outlined in the Policy and Procedure on Airway Maintenance. b. Count rate of respirations and note depth. c. Observe color of nail beds. 2. Assess and record vital signs as outlined in the Policy and Procedure. (Vital Signs in the PACU). 3. Assess and record level of consciousness. 4. Check armband for proper identification. 5. Assess and record skin temperature and condition. 6. Assess IVs for patency. [Type text] a. Record IV type, remaining fluid count, location of IV site and condition of IV site. 7. Assess and record position of patient. 8. Assess and record condition of dressings. a. Note anatomical location. b. Note amount and character of drainage. 9. Assess patency of drainage tubes. a. Note types of tubes, catheters, or receptacles. b. Note amount and character of drainage. 10. Assess neurovascular status of involved surgical extremities if indicated. a. Note color, temperature, capillary refill, sensation, and movement of extremity. b. Note presence and strength of pulses when applicable. 11. Assess and record presence of pain. END [Type text] PACU:Ketamine PACU POLICY SUBJECT KETAMINE I. POLICY: To keep verbal, tactile and visual stimulation to a minimum during the PACU period. II. PURPOSE: To prevent emergence reaction due to environmental stimulus. III. PROCEDURE: A. Observe rate and quality of respirations. B. Monitor vital signs. Blood pressure and pulse rate are frequently elevated; however, hypotension and bradycardia have been observed. C. Reduce stimulus to patient by decreasing verbal, tactile and visual components of surrounding environment, i.e. dimming lights, decreasing noise level and eliminating excessive movement around patient. D. Observe for side effects, i.e. enhanced skeletal muscle tone manifested by tonic and clonic movements sometimes resembling seizures, nausea, vomiting, diplopia, nystagmus and any arrhythmia. E. Orient patient quietly to surroundings. END [Type text] CONTROLLED DRUGS: DISTRIBUTION AND ACCOUNTABILITY POLICY Controlled drugs shall be distributed, administered, and accounted for in accordance with federal laws, rules, and regulations and the laws rules, and regulations of this state, and other applicable law. Controlled drugs include: - Medications listed in current Federal drug abuse prevention and control acts - Medications designated by regulations of this state RESPONSIBILITY The facility has overall responsibility for controlled drugs. DOCUMENTATION The Director of Pharmacy, acting as the facility's agent, shall ensure that the distribution and administration of controlled drugs are documented adequately by pharmacy, nursing service, and other involved services or personnel in accordance with federal laws and the laws of this state. STORAGE AND SECURITY The Director of Pharmacy, acting as the facility's agent, shall ensure adequate storage and security for controlled drugs in accordance with federal laws and the laws of this state. RECORD FILING Records for controlled drugs shall be filed so they are readily retrievable and receipt and distribution can be established. C-II records shall be separate from records of C-III through C-V drugs and noncontrolled drugs. Controlled substances records shall be maintained in a secure manner. END [Type text] PACU POLICY PACU STANDARDS OF NURSING PRACTICE I. The nurse will collect health status data. The data is obtained by physical exam, review of records, and consultation. A. Surgical procedure performed is documented B. Anesthetic technique and agents are reported C. Intraop complications are reported D. History of patient’s medical condition and medications are reported II. The nurse will make an initial assessment on arrival to PACU using a systematic approach. A. Assess Respiratory Status 1. Assess rate, character and patency of airway a. Type of artificial airway b. Patency of airway 2. Assess for symptoms of difficulty a. Retractions b. Nasal flaring c. Use of accessory neck muscles d. Restlessness e. Confusion or anxiety 3. Note signs of inadequate oxygenation a. Cyanosis blue nail beds b. Mottling of extremities c. Cool extremities 4. Pulse oximetry a. Maintain 02 Sat at 93% or above by use of 02 up to 100% [Type text] b. Notify Anesthesiologist for 02 Sat below 93% 5. Evaluation Endotracheal tube when present a. Assess patency b. Proper placement 1. Breath sounds and equality c. Check that tube is properly secured 1. Taped 2. Tied with umbilical tape d. Location of tube 1. Oral 2. Nasal 6. All general anesthetic patients will receive 40% O2 therapy unless ordered otherwise a. T-tube b. Face shield c. Ventimask 7. Assess tidal volume and NIF a. Parameters are obtained prior to extubation 1. Tidal volume…5-7ml./kg of body weight 2. NIF…-20ml 8. Assess the patient to be extubated a. Return of reflexes 1. Gag, swallow or cough b. Check level of consciousness 1. Comprehends and has ability to follow commands [Type text] c. Return of adequate muscle tone 1. Squeezes hand…good grip 2. Sustains head lift x 5 seconds 3. Able to open eyes 9. Maintains knowledge of extubation a. Suction oropharynx prior to extubation b. Suction ET only if needed, in a sterile manner c. Deflate cuff completely using syringe d. Have the patient take a deep breath, and extubate at the peak of inspiration e. Administer 40% O2 per face shield unless ordered otherwise f. Assess rate and depth of respirations post extubation g. Cough and deep breath every 30 minutes during stay in PACU unless contraindicated h. Elevate HOB unless contraindicated B. Assess Circulation 1. Place on cardiac monitor a. Asses rate b. Assess regularity c. Assess if any cardiac arrhythmias d. Notify Anesthesiologist of any change from pre-op EKG e. Notify Anesthesiologist of heart rate below 50 or greater than 120 and different from pre op 2. Monitor blood pressure a. Notify Anesthesiologist if systolic <90 or >180 C. Assess Temperature [Type text] 1. Oral temps will be taken unless contraindicated of the following patients a. Pediatric patient b. Patient with extensive oral surgery c. Comatose patient d. Patient with an altered level of consciousness who cannot comprehend 2. Note route a. Oral b. Rectal c. Axillary 3. If initial temperature is below 95° F a. Apply warm blankets b. Apply BAIR Hugger c. Recheck patient temperature every 30 minutes III. The nurse will establish a baseline for CVP, arterial liens, pulmonary artery pressure and wedge, as applicable. IV. The nurse will assess the neurological status. A. Assess level of consciousness 1. Stimulate verbally 2. If no response, attempt tactile stimulation 3. Continue to stimulate patient during PACU stay 4. Document patient response to particular stimulus B. Assess papillary response if indicated for that particular surgery [Type text] 1. Note equality and size 2. Notify physician of inequality or significant changes C. Assess the motor-sensory function 1. Be aware of history of orthopedic or neurological limitations (amputee, aphasic) 2. Observe spontaneous movement 3. If indicated, check patient for symmetrical movement and sensation of extremities 4. Consider the effects of anesthetic agents a. Level of spinal anesthetic b. Regional block c. Degree of movement d. Degree of sensation V. The nurse will assess skin and peripheral vascular system. A. Assess general integument 1. Color 2. Temperature 3. Degree of dryness B. Note any pre-existing condition 1. Rash 2. Injury 3. Decubitus 4. Scars 5. Stoma [Type text] C. Document peripheral pulse presence or absence, and character when indicated 1. Absent…0 2. Thready…1+ 3. Diminished…2+ 4. Normal…3+ 5. Bounding>>>4+ 6. Note capillary refill VI. The nurse will evaluate and assess the spinal anesthetic patient until there is a demonstration of decreased of spinal level. A. Maintain proper body alignment B. Evaluate level of anesthetic upon admit and document C. Assess any difficulty in breathing D. Observe for return of sensory-motor function E. Observe for drop of BP as a result of spinal anesthesia-notify Anesthesia VII. The nurse will assess all surgical sites and document condition (includes drains, incision, ostomy, chest tubes). A. Assess drainage from wound or drainage devices 1. Amount of drainage 2. Appearance of wound if applicable 3. Type of drainage devices 4. Patency of drains 5. Report excessive drainage to physician B. Check security of dressing [Type text] C. Attach all drains or tubes to appropriate equipment as ordered; check for 1. Nasogastric a. Check for position and placement b. Irrigate as ordered and record results c. Apply appropriately ordered suction d. Document drainage noted e. Secure tube for patient comfort 2. Chest Tubes a. Check for fluctuation, drainage and bubbling b. Always keep drainage unit below the level of the chest D. Assess urinary output if applicable 1. Maintain output 30ml/hr in catheters 2. Observe a. Clarity of urine b. Color of urine c. Meatal bleeding present d. Patency (clots) 3. Check abdomen for distention 4. Irrigate as ordered and chart results VIII. The nurse will assess fluid and electrolyte status and take supportive measures as ordered. A. Obtain reports of intra-operative I & O when available B. Observe IV sites 1. Patency 2. Redness, edema [Type text] 3. Location 4. Security C. Regulate IV fluids as ordered 1. Document type of fluid 2. Check doctor’s orders for appropriate fluid and rate 3. Label IV bottles if medication added a. Med added b. Dosage c. Date d. Time e. Nurse’s name D. Observe for signs of hemorrhage 1. Increased pulse rate 2. Decreased BP 3. Skin cool, clammy 4. Excessive wound drainage 5. Decreased level of consciousness E. Maintain accurate I & O IX. The nurse will administer drugs and solutions as prescribed. A. Administers medication according to hospital policy 1. Check allergies 2. Route 3. Dosage 4. Patient identified, using patient identifiers (patient name and visit number) [Type text] 5. Staff has knowledge of complications and contraindications of drugs B. Evaluate patient in relation to drugs administered 1. Patient condition and function 2. Amount of drug given and the duration of it’s effect 3. Assess response of any prn meds given C. Titrate drugs always on pump i.e., Lidocaine, Nipride, as outlined in Nursing Policy X. The nurse will use aseptic technique when caring for the patient. A. Universal precautions will be used when: 1. Handling blood 2. Handling body fluids 3. Extubating the patient B. As ordered per physician, nurse will use appropriate isolation technique XI. The nurse will use the Aldrete Score System to numerically evaluate the patient. A. Score and Record 1. Admit 2. Specific intervals 3. Upon discharge B. Numerical scores of 8-10 must be obtained to be discharged, unless obtaining release from Anesthesiologist XII. The nurse will provide safety to the post-op patient. A. Maintain side rails up at all times B. Pediatric patient will not be left unattended [Type text] C. A patient unreacted from general anesthesia will not be left unattended 1. Unable to support own airway 2. Unable to follow commands D. Combative patients will be protected from physical injury 1. Notify Anesthesia for appropriate treatment 2. Use restraints when indicated, as outlined in the WMC Restraint Policy E. All electrical equipment will be used in the proper manner XIII. The nurse will promote comfort and well being of the patients. A. Check for restrictive dressing B. Turn and reposition for comfort as indicated per procedure C. Assess pain intensity per pain scale 0-10 and quality D. Provide relief of nausea and vomiting through medication and other comfort measures E. Provide hygiene as indicated 1. Clean gown 2. Clean face, extremities, etc. F. Explain activities and procedures at patient’s level of understanding G. Control noise level XIV. The nurse will assure the safety of the pediatric patient. A. Patient will never be left unattended B. When necessary, use restraints to prevent dislodgment of IV tubes, etc. as outlined in the Restraint Policy [Type text] XV. Assessment will be age-specific, taking into account the principles of growth and development over a life span. XVI. All nursing care is planned. A. Based on the patient assessment; a plan of care is established B. Expected outcomes are defined C. Interventions are done D. Evaluation and re-evaluation takes place in regards to expected outcomes END [Type text] PACU POLICY ISSUED VITAL SIGNS IN THE PACU I. POLICY: Respiratory and circulatory monitoring will be carried out on all PACU patients. II. PROCEDURE: Blood pressure, pulse and respirations will be taken by the attending PACU RN as often as deemed necessary within the following guidelines: A. Adults – On patients 7 years of age or older, blood pressure, heart rate and respirations (with SaO2) will be checked and recorded at no longer than 10 minute intervals. B. Children – Heart rate and respirations (with SaO2) will be checked and recorded below 7 years of age. Blood pressure will be checked and recorded as warranted. C. Temperatures will be taken on all patients. Temperature must be above 95 degrees core before the patient can be discharged to the room. D. Regional block patient’s vital signs will be taken and recorded as outlined in each block Policy and Procedure. END [Type text] PACU POLICY PACU STANDARDS OF OUTCOME I. The patient will have maintained or achieved adequate physiological function upon discharge from the PACU. A. Respirations full, deep, regular or as pre-op status. B. Able to cough and deep breath freely or as pre-op status C. Systolic blood pressure within 50 points of pre-op range. D. Oriented to person, place and time, with exception of pediatric patient or patient with altered mental status as pre-op. E. Moves all extremities as pre-op with exception of regional block anesthesia. These patients must demonstrate a return of sensory level. F. Drains are patent and without excessive drainage. G. Catheter draining adequate urinary output…30ml/hr. H. IV patent. I. Skin integrity is maintained. J. Peripheral pulses present as applicable to procedure. K. Good capillary refill when applicable. L. Surgical site assessed. 1. Free of excessive drainage. M. Accurate PACU I & O. N. A level of comfort is achieved. II. The patient’s stay in PACU is in a safe environment. A. Patient is free of injury. 1. Protection of prominent body parts. B. PACU is free of preventable hazards. [Type text] C. Nurse will initiate and maintain isolation when indicated. D. Ensure proper disposal of contaminated materials. III. The patient will experience minimal pain and discomfort. A. Pain medication administered as ordered END [Type text] PACU POLICY SUBJECT: PATIENT SAFETY I. POLICY: All PACU room personnel responsible for attending post-anesthesia patients will be acutely aware of safety practices necessary for the prevention of injury, post-op complications arising from unsafe acts and even death as a result of these. Personnel will make every effort to prevent unsafe situations and will take steps to correct them when they occur. II. PURPOSE: The post-anesthesia patient cannot be considered responsible for his own actions. Due to lethargy, disorientation, delayed or diminished reflexes and pain, he may be unable to prevent injury to himself and others and unable to correct situations which are potentially hazardous. Therefore, the responsibility for patient safety in the immediate post-operative period rests entirely with all PACU personnel involved in the care of the patient. III. SAFETY RULES: A. Wall suction must always be in working order and readily accessible to the nurse and patient. This cannot be over-emphasized as vomiting (leading to aspiration) or airway obstruction from excessive oral secretions can arise suddenly and without warning. B. Until fully alert and quiet, all children must be attended by a nurse who does not leave the bedside. Even after awakening, a child must be monitored very closely and personnel must remain at bedside in order to prevent injury from falling or climbing off stretcher, pulling off dressing, removing IV or vomiting. One-to-one ration of PACU staff to child should be continuously provided. C. Siderails on PACU stretchers must always remain up for the duration of the stay. D. If patient is disoriented and combative, restrain manually, sufficient to prevent injury to patient and staff. Call for help if needed. Restraints may be applied as outlined in Restraint Protocol. E. If vomiting occurs or appears imminent, turn patient to side and be ready to suction. F. All electrical equipment must be properly grounded. [Type text] G. O2 outlets, suction, defibrillator and cardiac monitor must be checked at the beginning of each day to assure they are working properly. H. Use of woolen or nylon blankets, gowns and linen is prohibited. I. Under NO CIRCUMSTANCES is a patient to be left unattended in PACU, regardless of degree of alertness and orientation. Complications such as vomiting, cardiac or respiratory arrest of hemorrhage can occur within seconds and a nurse must be in attendance at al times. J. All drugs, IV solutions and sterile supplies necessary for the care of PACU patients must be checked for expiration date prior to usage. If there is ever any doubt as to the sterility or composition of a product, it must be considered unsafe and discarded. K. All personnel must be thoroughly knowledgeable of their responsibilities in case of fire or disaster. Action must be taken quickly and efficiently in order to avoid a catastrophe. L. When transporting patients back to nursing unit, personnel must assure that the patient’s upper and lower extremities are not protruding over or through siderail spaces. Serious injury to fingers, hands, elbows and feet may result if stretcher strikes a door or wall or brushes too closely to these surfaces. M. When turning and positioning, patient’s extremities must be well-supported and in good alignment. Permanent nerve damage, fractures and dislocations may result from patients unconsciously lying on upper extremities for long periods of time. N. When patient is transferring from PACU stretcher to bed, both must be supported (using at least 2 people) and the patient assisted. O. After patient has been transferred to bed, siderails must be put up and bed left in “low” position. The nurse’s call light must be positioned close to patient so that they would be able to use if necessary. END [Type text] PACU POLICY DISCHARGE CRITERIA I. POLICY: The establishment of standardized and measurable criteria for patient readiness of discharge from the PACU is to provide a smooth transition from the PACU to the next step in the patient’s post-operative course. II. PURPOSE: To assure that the post-anesthesia patient’s condition is stable and that he/she is returning to their pre-anesthesia state. III. PROCEDURE: Along with the Aldrete Post-Anesthesia Score, the following criteria are also considered in discharging patients from the PACU: A. Clear Airway – Patient is extubated and airway unobstructed. B. Consciousness – Patient is easily awakened and is oriented to time, place and person. C. Stable Vital Signs – Blood pressure, pulse and respirations coincide with preoperative readings. Blood pressure does not vary more than 50 mmHg from what is considered normal for that patient. Pulse oximeter reading must be at least 93%. Temperature will be taken at discharge and should be at a minimum of 95º core. D. Dressings intact – Nurses Notes will reflect whether the dressing remained dry or required changing in the PACU. E. Patent drains and tubings – Drainage is free and unobstructed. Urine output is at least 30mL/hr. IV lines are functioning. F. Implementation of physician’s orders – A notation will be made on the physician’s order sheet indicating the order was executed, with further explanation recorded in the Nurses Notes. G. If narcotics were administered, the patient must remain in the PACU 30 minutes after the time of initial dose. H. The length of stay depends on the type of surgery and anesthesia and how quickly the individual patient reacts and stabilizes. I. The minimum length of stay for an adult is 30 minutes. Pediatric patients may be discharged sooner. [Type text] J. If the patient has had a regional block, he must exhibit a degree of motor sensory return. K. Aldrete Post Anesthesia Recovery Score (see Aldrete Scoring System Policy) – A total of 8 or more must be achieved before the patient can be discharged to the nursing floor units. Each patient shall be evaluated according to his/her individual baseline values in each of the areas. If a total score of 8 is not achieved, Anesthesia staff will not be given a status report. If Anesthesia releases the patient to the room at this time, this information will be documented in the Nurses Notes. A patient going to the Critical Care Unit or Progressive Care Unite may have a score of less than 8. L. Those patients who are placed in the Critical Care Unit or Progressive Care Unit postoperatively are not required to meet discharge criteria. M. Some patients will not meet discharge criteria. In order to be discharged, a verbal order from the Anesthesia staff or Surgeon must be obtained. IV. PROCEDURE TO DISCHARGE: A. The discharge nurse will evaluate whether discharge criteria have been met. The appropriate box on the PACU Record will be checked. If criteria are not met, an order for discharge is obtained and documented. B. If the discharge criteria are met, the standing order for discharge is checked on the PACU Record and the Anesthesiologist’s name is recorded. C. If the discharge criteria are not met, the verbal order for discharge is checked on the PACU Record and the Anesthesia staff’s or Surgeon’s name is recorded. D. The attending nurse will review the chart to ensure that all pertinent Physician’s orders have been initiated and that supply charges and medication charges are correct. E. The Nursing Unit to which the patient will be returning will be notified of patient’s transport and report will be given. F. Patients will be transported per bed or stretcher to their room. In cases involving small children, they may be carried to the unit. G. When the patient is 13 years or younger, the nurse will stay in attendance with the patient in the room until the family returns or the unit nurse relieves. END [Type text] Surgical Policy: Environmental Cleaning SURGERY POLICY ENVIRONMENTAL CLEANING I. POLICY: A. All surgical patients are considered potentially infected with bloodborne pathogens, therefore, the same environmental cleaning protocols should be implemented for all surgical procedures. B. Terminal cleaning is performed daily and on a scheduled basis by Surgery personnel and Environmental Services personnel II. PURPOSE: A. To provide guidelines for environmental cleaning of the Surgical Department. B. To provide a clean environment within the Surgical Department that minimizes patient and employee exposure to potentially infectious microorganisms. III. PROCEDURE: Environmental cleaning measures are required before, during and after each surgical procedure and at the end of each day. A. All horizontal surfaces within the Operating Room (ie: furniture, light, equipment) should be damp dusted with a facility-approved agent and mechanical friction before and after each surgical procedure and at the end of each day. B. A visual inspection should be made for cleanliness before case carts, supplies and instruments are brought into the Operating Room. C. Equipment from areas outside of the Operating Room should be damp dusted with a facility-approved agent before being brought into the Operating Room. D. During surgical procedures, contamination should be confined and contained within the immediate vicinity of the surgical field as much as possible. E. Accidental spills of contaminated debris (ie: blood, tissue, body fluids) in areas outside of the immediate surgical field should be cleaned promptly as possible using a lint-free cloth saturated with a facility-approved agent. F. Contaminated items should be handled using protective barriers. [Type text] G. Contaminated, disposable items used in patient care should be placed in leak-proof containers or tear-resistant, red, biohazard bags to prevent exposure of personnel to items potentially contaminated with infectious microorganisms and to prevent contamination of the surgical environment. H. Contaminated, reusable items should be placed in leak-proof containers to prevent exposure of personnel to blood, tissue and/or body fluids and to prevent contamination of the surgical environment. I. All disposable sharps (ie: needles, scalpels, ESU tips, safety pins) are considered infectious waste and should be placed in special puncture-resistant containers that are labeled as containing biohazardous material. J. Used surgical instruments, basins, trays and other items should be handled only by workers wearing personal protective equipment until decontaminated. K. Floors should be cleaned using a facility-approved agent and a fresh mop after each surgical procedure and at the end of each day. L. Patient transport vehicles, including straps and attachments, should be cleaned with a facility-approved agent after each use. M. Surgical procedure rooms and scrub and utility areas are terminally cleaned daily by Environmental Services. Terminal cleaning includes but is not limited to: i. Surgical lights and external tracks ii. Fixed and ceiling-mounted equipment iii. All furniture and equipment, including wheels and casters – step stools and light switches iv. Hallways and floors v. Handles of cabinets, doors, telephones and push plates vi. Ventilation faceplates vii. Horizontal surfaces (i.e.: tops of counters, sterilizers, fixed shelving) viii. Substerile areas ix. Scrub sinks x. Scrub/utility areas [Type text] N. All areas and equipment in the Surgical Department should be cleaned according to an established schedule, including, but not limited to: i. Ducts and filters ii. Air conditioning equipment iii. Closets, cabinets and shelves iv. Warming cabinets, refrigerators and ice machines v. Walls and ceilings vi. Storage areas vii. Offices, lounges and locker rooms O. Cleaning equipment should be disassembled, cleaned with a facility-approved agent and dried before storage END [Type text] [Type text] Central Supply Department Steam Sterilization: Instrument Packaging I. POLICY: The preparation of trays and sets will be done as outlined. II. PROCEDURE: A. All instruments, syringes, needles and other items shall be clean prior to being placed in the set. B. Dry instruments prior to packaging. C. Inspect instruments to make sure that they are clean, dry, and functioning properly. (An exception to “dry” is when a small residual of distilled water is required to assist in steam sterilization of items with small lumens such as needles or tubes.) Soiled objects shall be returned for decontamination. Objects that do not function properly shall be removed and replaced with properly functioning items. D. Open, unlock, or disassemble instruments to permit steam to contact all surfaces. E. Instruments shall be placed in or on a perforated tray, basket or in a container system specifically designed for that use. F. Instruments shall be assembled according to Censitrac count sheets to be included with instrument sets or by index cards with tray contents kept in CSR. G. Instrument Trays 1. Use a mesh-bottomed or perforated tray or equivalent. Instrument trays shall be designed for effective sterilization, drying and orderly arrangement of instruments. [Type text] 2. Place a fully opened (single layer) green towel in bottom of tray to assist with drying. Use a towel, which covers the bottom of the tray with minimum excess overhang. 3. Prior to the wrapping of trays or sets, a chemical integrator shall be initialed with the staff member preparing the tray and placed inside. 4. Include count sheet. 5. Non-woven wrappers shall be used to wrap instrument trays. Each tray shall be double wrapped with sheets of wrapping material. The tray will be fastened with sterilization tape containing a chemical indicator and the lot load sticker [Type text] H. Container Systems 1. Instrument sets that are in container systems shall be assembled and sterilized according to manufacturer’s instructions. 2. A chemical integrator shall be initialed with the staff member preparing the tray and placed inside. 3. A filter(s) will be placed in the lid of that container system as required. 4. Container locks will be placed on the clamps of the container. 5. A steam indicator card with the lot load will be placed in the appropriate slot on the side of the container. Employee will initial care. I. Peel Packs 1. Small items and single instruments may be sterilized in paper/plastic peel packs. 2. A chemical integrator shall be in the inside of all peel packs. 3. A second chemical indicator shall be on the outside of the peel pack. 4. The initials of the staff member preparing the pack shall appear visible to the user on instrument label or near label. 5. The lot load sticker will be placed on the outside of the package. J. Instruments shall be distributed evenly to facilitate proper steam and especially to facilitate drying of sets after sterilization. K. The weight of wrapped prepared sets shall not exceed 17 to 25 pounds. L. Each tray or package shall be clearly marked as to its contents. If items are missing or the tray or set is incomplete, notation is made with an orange colored sticker placed on the outside of the wrapper clearly visible to the user. M. For recall purpose, a sterilizer load log for each load will be available in the event of a sterilizer failure. N. Instrument trays that are not used frequently may be wrapped in plastic dust covers immediately after sterilization and drying to protect the integrity of the set. END [Type text] Central Supply Department Central Supply Department Steam Sterilization: Cycles POLICY: Sterilization is the process by which all microorganisms are killed. This is accomplished in a sterilizer that is equipped with automatic time-temperature controls which carry out automatically all the steps in sterilization. PROCEDURE: PREVACUUM CYCLES - WRAPPED, PEEL PACK INSTRUMENT SET WEIGHT TEMPERATURE EXPOSURE TIME DRY TIME Less than 17 pounds 270-274° F 10 minutes 30 minutes 17 – 25 pounds 270-274° F 10 minutes 30 minutes GRAVITY CYCLES - WRAPPED, PEEL PACK INSTRUMENT SET WEIGHT TEMPERATURE EXPOSURE TIME DRY TIME Less than 17 pounds 270-274° F 15 minutes 30 minutes Less than 17 pounds 250-254° F 30 minutes 30 minutes 17 – 25 pounds 270-274° F 15 minutes 45 minutes 17 – 25 pounds 250-254° F 30 minutes 45 minutes FLASH CYCLE – OR, UNWRAPPED INSTRUMENT SET WEIGHT TEMPERATURE EXPOSURE TIME DRY TIME Single Instrument 270° F 4 minutes 1 minute Small – Medium Tray 270° F 10 minutes 1 minute Single Instrument withLumen270° F 10 minutes 1 minute [Type text] Central Supply Department Steam Sterilization: DART Test(Bowie-Dick Test) POLICY: DART (Bowie-Dick) tests are designed to document the removal of residual air from a sample challenge load and will be run before sterilizer use each day. The proper functioning of sterilizer shall be tested in a separate, special cycle by the use of a DART (Bowie and Dick) test, which is designed to test for the removal of air from the chamber during the pre-vacuum stage and which alerts the CSR technician of air pockets (air does not mix with steam) or other malfunctions of sterilizer. Satisfactory test results will show a black uniform coloring. Critical to note are light areas which denote the presence of air pockets within the test pack, and therefore, signal a problem with prevacuum apparatus. Notify unit director immediately if observed or in doubt. PROCEDURE: I. Turn power switch on, chamber must be operating at temperature (270°-274° F) when DART (Bowie-Dick) test is performed. A leak test or a warm up cycle should be completed prior to performing DART (Bowie-Dick) test. II. Bypass the PERFORM LEAK TEST? Prompt when it appears in the display window, unless Leak Test is required at this time. Once the Leak Test has been bypassed or run, the following message appears on the display: � PERFORM DART TEST? (BOWIE-DICK) 1=Y 2=N III. Press the cycle selector touch pad number 1 for YES and the display will show the following: � IS A WARM-UP CYCLE [Type text] REQUIRED? 1=Y 2=N If a warm-up Cycle is required…Press cycle sector touch pad number 1 for YES if the sterilizer is not operating at temperature IV. Press cycle selector touch pad “1” and sterilizer automatically runs a flash type warm-up cycle with three minute sterilize and 1 minute dry times. At the completion of warm-up cycle, display will show the following message: � LOAD DART PACK (Bowie Dick Plus Test Pack) PRESS 1 TO TEST If a warm-up cycle is not required…Press cycle touch selector pad number 2 for NO if sterilizer is at operating temperature (i.e., Leak test has just been performed or the unit has been in operation � Display � LOAD will show the following message: DART PACK (Bowie Dick Plus Test pack) PRESS 1 TO TEST V. Place the Bowie Dick Plus Test Pack on lower shelf of sterilization cart. Position pack where it will be over the drain. Push cart into sterilizer. Run test in empty chamber. VI. Close and lock door. VII. Press cycle selector touch pad “1” to perform the test cycle. The sterilizer will automatically proceed through a prevacuum test cycle with four pressure/vacuum pulses and a three and one half sterilize and one minute dry time. VIII. Unlock and open door at the end of the cycle and remove DART (Bowie Dick Test). Take the Bowie-Dick Test sheet out of the middle of the test pack. IX. Interpret the results as follows: � PASS-Indicated by a uniform black color on the Test Grid [Type text] � FAIL-Indicated by a color response other than black: dark brown, light brown or the original yellow color is unacceptable X. After interpreting the results, enter the date, sterilizer number, operator ID on test sheet. File test sheet in designated file. XI. If the first test fails, the sterilizer can still be qualified by generating two consecutive acceptable results, Test #2 and Test#3. XII. If unacceptable results are indicated for Test #2 OR #3: A. Sterilizer shall be placed out of service. A sign will be placed on the unit to say that it is out of order. B. Report malfunctions and positive DART (Bowie Dick) tests to CSR Coordinator, Perioperative Director and Infection Control Coordinator. C. Biomed shall be notified. D. If able, Biomed will correct problem. E. If unable, Biomed will make any necessary follow-ups to correct the problem. F. Sterilizer will remain out of service until two (2) consecutive acceptable results are obtained. Central Supply Department Decontamination Area POLICY: [Type text] The Central Supply Department will render items free of disease causing bacteria thereby making it safe for handling by hospital personnel and safe for patient contact. PROCEDURE: I. Receiving and handling soiled supplies require special care and these supplies are considered contaminated. II. All Items are received in the decontamination area for cleaning following any procedure. This is to include loaner trays and instruments from other departments of hospital. III. Inspect returned trays and instruments to determine if all parts have been returned. Notify coordinator of any missing parts or instruments. IV. Do not use any items that are not in good condition, are not in working order, or are tagged as needing repair. Place any item that is not in good condition in the repair box. V. Instruments from OR are received in a basin with a biohazard label, and in enzyme detergent. Instruments from other areas in the hospital should be washed in enzyme detergent and placed in bag with biohazard label. Items are brought into decontamination area and CS personnel are notified. VI. When removing instruments from basins and sinks, tongs or forceps will be used to remove instruments to protect employees from sharps injuries. VII. Open all locked instruments and disassemble parts. VIII. Handle delicate, precision items with care to avoid damage and repair. IX. Place instruments in wash pan/mesh basket, place in washer. X In addition to normal dress code requirements, the personnel working in this area shall wear PPE aprons, gloves, and face shields. XI. Traffic control shall be strictly regulated. [Type text] Central Supply Department Subject: Decontamination: Manual Cleaning POLICY: Some instruments and delicate equipment will be manually cleaned. SUPPLIES: Moore Center approved enzyme cleaner solution Brushes Clean cloths Towels (to protect from hard surfaces) Tap water Compressed Air PROCEDURE: I. Instruments are placed in basin of enzyme/water solution. Allow instruments to soak 10 minutes. II. When removing instruments from basins and sinks, tongs or forceps will be used to remove instruments to protect employees from sharps injuries. III. Manually wash instruments in solution removing blood and protein products under water with brush. IV. Give particular attention to serrations, hinges, locks and teeth. V. Avoid using harsh abrasives and cleansing agents, to keep from damaging the steel or plating. VI. Rinse the instruments thoroughly in warm running water. VII. Remove instruments from warm water, place on towel to air dry. VIII. Inspect each instrument while drying it. This will make it unnecessary to pick up, open and close it again later. Manipulate locks and hinges until they work freely, then wipe them as dry as possible with a clean cloth before sterilizing. [Type text] Central Supply Department Steam Sterilization:ATTEST ™ Rapid Readout BiologicalIndicators POLICY: All steam autoclaves will be biologically monitored daily with ATTEST™ Rapid Readout Biological Indicator 1291 for Amsco flash sterilizers and ATTEST™ Rapid Readout Biological Indicator 1292 for CSR steam autoclaves. The best way to ascertain the sterility of an article or to verify the sterilization process is to use a biological monitor. A live spore test utilizing B. stearothermophilus is the most reliable form of biological monitoring. Record the results of all biological monitoring in 3M-log book located in CSR. PROCEDURE: I. All biological monitors are preassembled by the manufacturer 3M. Use ATTEST™ Rapid Readout Biological Indicator 1291 for Amsco flash sterilizers and ATTEST™ Rapid Readout Biological Indicator 1292 Reference #41382 for CSR steam autoclaves. II. Identify the ATTEST Rapid Readout Biological Indicator by writing the sterilizer, load number and processing date on the indicator label. Do not place another label or indicator tape on the ATTEST indicator vial or on the cap. III. Place a Rapid 5 Steam Plus Test Pack Reference #41382 on the front lower rack in a fully loaded sterilizer. This pack is referred to as a PCD – Performance Challenge Device – contains 1 BI and a class 5 integrator. IV. Place Attest Biological in the flash sterilizer in the most challenging area for the steam sterilent, on the bottom shelf, near door and over the drain. [Type text] V. Process the load as usual in CSR autoclaves and flash autoclaves should be run on a four-minute cycle or 10 minute cycle depending on the type of implants or instruments flashed. VI. After completion of the cycle remove ATTEST steam – wait 15 minutes after door opens flash – wait 5 minutes removing the ATTEST biological indicator. (Crushing or excessive handling of the biological indicator before cooling may cause the glass ampule to burst, which may result in personal injury from flying debris. Therefore, the use of protective eyewear and gloves when removing biological indicators from the sterilizer is recommended. Protective eyewear should also be worn when crushing biological indicators.) VII. Remove the ATTEST biological integrator from Attest PCD. VIII. Check the chemical indicator on the label of the biological indicator. A color change from rose to dark brown confirms the biological indicator has been exposed to the steam sterilization process. This color change does not indicate that the process was sufficient to achieve sterility. If the chemical indicator is unchanged, check the sterilization process. IX. Press the cap down. Crush the glass ampule of the biological indicator in the crusher well of the incubator. Hold the biological indicator by the cap and tap on a hard surface until media wets the strip at the bottom of the vial. X. Crush, tap and incubate at least one non-sterilized ATTEST ™ Rapid Readout Biological Indicator (positive control) each day a processed indicator is incubated in the auto-reader. The positive control should be from the same lot number as the processed indicator. It is not necessary to calibrate the auto-reader. XI. Incubate the positive control and the processed indicator at 60 ± 2º C (140 ± 3º F) for one hour for ATTEST™ Rapid Readout Biological Indicator 1291 for Amsco [Type text] flash sterilizers and three hours for ATTEST™ Rapid Readout Biological Indicator 1292 for CSR steam autoclaves and read the results in the ATTEST auto-reader. The final negative biological indicator reading is made at one hour or three hours. Discard the used indicator in a hospital-approved container. XII. Interpretation of results are as follows: � For the sterilized biological indicator, a negative (green light or -) after appropriate incubation period indicates an acceptable sterilization process. A positive (red light or +) indicates that a sterilization process failure has occurred. � The positive biological indicator control must provide a positive result (red light or +). If the positive biological indicator control reads negative (green light or -), check the incubator temperature and the auto-reader with a new positive biological indicator control. The processed indicator results are not valid until the positive biological indicator control reads positive (red light or +). XIII. Immediately act on any positive biological indicator results. ALWAYS retest the sterilizer for processing loads until the biological indicator results are negative. If the sterilized biological indicator indicates a positive load,the autoclave shall be removed from service and repaired. Central Supply Department Subject: Decontamination: Washer/Disinfector POLICY: The Amsco washers shall be used to wash all contaminated instruments or reusable medical devices that do not require hand washing. PURPOSE: [Type text] To establish a means to initially decontaminate reusable medical devices that does not require hand washing. PROCEDURE: I. Amsco washers shall be operated according to manufacturers written instructions. II. In the decontamination area, push the “door open” button on the display panel and open washer door. III. Pull out washer carrier. IV. Load basket on carrier and return carrier to washer. V. Push the “close door” button and wait for door to close, select the appropriate cycle and push “cycle start” button. VI. When the cycle is complete, the alarm will sound VII. In the sterile supply room (prep and pack area), push the “door open” button on the display panel and wait for door to open. VIII. Remove carrier carefully as the instrument temperature may be as high as 180°F, remove baskets and return carrier to the washer. IX. Push the “door close” button on the display panel. X. Check read-out of Amsco washers at the end of each cycle to be sure all perimeters for washing of instrumentation have been met. XI. Report problems to CSR supervisor. END