Abstract Voorjaarscongres 2013 Nederlandse Vereniging
advertisement

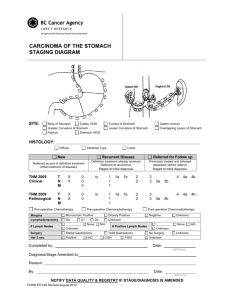
Abstract Voorjaarscongres 2013 Nederlandse Vereniging voor Gastro-Enterologie Who determines the N-stage in colon carcinoma: Pathologist or Surgeon? da Costa D.W.1, van Wagensveld B.A. 1, Wassenaar K. 2, van Tets W.F. 1, Keizer K. 2, Witte B3, van Dekken H2, Vrouenraets B.C.1 1 Department of Surgery, Sint Lucas Andreas Hospital, Amsterdam, Deptartment of Pathology, Sint Lucas Andreas Hospital, Amsterdam 3 Department of Epidemiology and Biostatistics, VU Medical Center, Amsterdam 2 There is evidence suggesting that the more lymph nodes are examined in patients treated for colon cancer, the better the disease can be staged and therefore a more accurate prognosis can be given. According to the Dutch guidelines for colorectal cancer, a minimum of 10 nodes should be analyzed in order to produce a reliable N-stage. Dutch qualifications for providing first-rate health care include finding at least 10 lymph nodes in 80% of all patients with colorectal cancer. We analyzed the number of lymph nodes in patients surgically treated in our hospital over a period of three years (2008-2010). Patients who had received neo-adjuvant treatment were excluded. Our patient group consisted of 156 patients with a median age of 77 (range 29-91 years) and mean of 13 nodes per patient. In 106 patients (67.9%) 10 or more nodes were found. In addition to baseline characteristics and tumour specific data we examined the role of two individual GI-surgeons (A and B), non-GI specialized surgeons (group C) and seven individual pathologists in finding 10 or more lymph nodes. Our univariate model showed that the presence of ≥10 nodes was influenced significantly by tumour size (P=0.050), tumour location (P=0.015) and associated type of resection (P=0.034), individual surgeon (A vs. B; P=0.023) and individual pathologist (A-G; P=0.005). No significant differences were found between GI-surgeons and non-GI specialized surgeons. Individual surgeons (P=0.8) or pathologists (P=0.4) did not influence finding an N+ status. Multivariate factors significantly contributing to finding ≥10 nodes were patient age (P=0.044), type of resection (p=0.007), M-stage (p=0.010) and again individual surgeon (A vs. B; P=0.012) and pathologist (A-G; p=0.004). Odds ratios for finding ≥10 nodes were 4.2 [95% CI: 1.4-12.5] for surgeon B vs. surgeon A and 3.9 [95% CI: 1.1-13.1] for surgeons C vs. surgeon A. Odds ratios between the seven individual pathologists varied from 0,2 [95% CI: 0.03-1.7] to 22,5 [95% CI: 3.8-134.6]. Conclusion: in addition to baseline characteristics and tumour aspects, individual surgeons and pathologists have influence on finding 10 or more lymph nodes in colorectal cancer patients.