Experimental Research of Fibroblasts Rebuilding Decellularized
advertisement
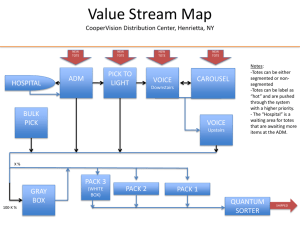
Experimental Research of Fibroblasts Rebuilding Decellularized Dermal Matrix Daofeng LIU 1,a , Xin Sheng HUANG1,band Jinhua ZUO2,c 1 Shengli oilfield central hospital, 2 Dept. of oral and maxillofacial surgery, affiliated hospital of Binzhou medical college No. 31, Jinan Road #1, Dongying City, Shandong Prov. 257034, China Keywords: fibroblast; acellular dermal matrix; hydroxyproline; matrix metalloproteinase-1. Abstract: purpose: Discuss the function of the fibroblasts in the process of decellularized dermal matrix rebuilding. Method: The research team established the animal model of ADM allograft, and cut the specimens to do HE dyeing, picric acid-sirius red dyeing and matrix metalloproteinases 1 immunohistochemical dyeing to test the hydroxyproline at the scheduled time. Results: Count the fibroblasts: the number of the fibroblasts increased sharply within 2 weeks, and the number reached the peak at 2 weeks , and it gradually decreased to the level of genuine leather. Ⅰ/Ⅲ collagen ratio: The ratio declined from 1 to 4 weeks, and the ratio rised to the level of genuine leather. Hydroxyproline: The Hydroxyproline increased within 4 weeks, and the number increased to level of genuine leather. MMP-1 activity: The value of the AOD decreased within 3 weeks, and the value decreased sharply from 2 to 3 weeks, and the value of the AOD increased gradually to level of genuine leather. Conclusions: The fibroblasts has the main function in the process of decellularized dermal matrix rebuilding. 1 Instruction Acellular dermal matrix was made of natural skin except epidermis and dermal cells. And the ADM only retain the collagen and the extracellular matrix, and it is widely used in the clinic [1-2]. The fibroblast is the most important cell in the connective tissue cells. This study explained the function in the process of decellularized dermal matrix rebuilding through observing the dynamic change of ADM allografts. 2 material and method There were 70 male rats that were 2 months of age(license: SCXR(Lu)20060004), and the weight was 250±25g. And the researchers collected 14 male rats to prepare ADM. And the others was divided into 7 groups to allograft ADM. And in 1, 2, 3, 4, 8, 16, 24 weeks, the researchers drew materials. The disposal of the animals accorded with 《Ethical issues in animal experimentation》. 2.1 reagent and instrument DispaseⅡ(Invitrogen Co. USA), Triton X-100(Amresco Co. USA), Mobay Chemical Co. USA, ECLIPSE E600 POL ( Nikon ) , ultraviolet visible spectrophotometer, hydroxyproline checkerboard, rabbit anti rat MMP-1 PcAb. 2.2 preparation of ADM We used the method of Dispase-Triton to prepare ADM. 2.3 animal model of ADM allograft The rats was injected in the peritoneal with 3.6% chloral hydrate(1ml/100g), and they were fixed in the anatomy after the success of the anesthesia. And the hair of the back should be removed and sterilized. The researchers made a full-thickness incision which is 2 cm long on the left of the centre line of the back to separate the lacuna. And then ADM was inserted into the lacuna, and was fixed with line 1 after flatting four corners. After the incision and bandage, the rats was fed in the single cage. 2.4 animal model of ADM allograft The rats was injected in the peritoneal with 3.6% chloral hydrate(1ml/100g), and they were fixed in the anatomy after the success of the anesthesia. And the hair of the back should be removed and sterilized. The researchers made a full-thickness incision which is 2 cm long on the left of the centre line of the back to separate the lacuna. And then ADM was inserted into the lacuna, and was fixed with line 1 after flatting four corners. After the incision and bandage, the rats was fed in the single cage. 2.5 results At a predetermined time, the researchers executed the animals to get the specimens. 2.5.1 observation index The size of ADM, color, texture and the relationship with the surrounding tissue, etc. 2.5.2 HE dyeing We used the conventional method, and observed with the ordinary microscope. And the researchers chose 10 slices at every time point, and randomly selected five high vision(*400) from each slice. 2.5.3 Picric acid-sirius red dying Paraffin slice was dewaxed to water. And the picric acid-sirius red was inserted into the paraffin slice for 1 hour. And then, we used distilled water to wash 5 min. We used the hematoxylin to strain. And the researchers chose 10 slices at every time point, and randomly selected five high vision (*400) from each slice to observe the collagen distribution of Ⅰ(red) and Ⅲ(green). And we use IPP 6.0 software to analyze the collagen distribution of Ⅰ(red) and Ⅲ(green). 2.5.4 hydroxyproline We tested the absorbance through the specification. We make the following rules. H is the content of the hydroxyproline. D is the determination absorbance. B is blank pipe absorbance. S is standard pipe absorbance. Sc is content of the standard pipe. Hv is the volume of the hydrolysate. W is the wet weight of the organization. D B Hv H Sc S B W 2.5.5 matrix metalloproteinase-1(MMP-1) immumohistochemical dyeing The researchers chose 10 slices at every time point, and randomly selected five high vision(*400) from each slice with IPP 6.0 software to test average optical density. 2.6 Statistics The data was shown as mean±standard deviation, and we use SPSS 13.0 to analyze. The statistics had meaning if the p<0.05. 3 Results 3.1 physical characteristics ADM was smooth within 1 week. The color didn’t change within 2 weeks. The more area increased more and more within 3 weeks. ADM was covered by the film which was covered with blood-vessel network, and the color of the ADM was milk white, and the area equal to the beginning of the transplant. ADM fused with the skin within 8 weeks. And the thickness of the ADM pinched after 16 weeks. 3.2 HE dyeing FB around the ADM increased, and the shape was ball within 1 week, and we could see the capillaries. There were more FB in the center of the ADM, and the shape change into a long spindle within 2 weeks, and the collagen accumulated around the ADM, and the blood vessels was rich. 3.3 picric acid-sirius red dyeing ADM has strong sense of layer with polarization microscope, and red bulk fasciculate I type collagen composes rack, and green thin Ⅲ type collagen distribute in it. 3.4 change of hydroxyproline content OHP content increased within 4 weeks, and after 4 weeks, OHP content decreased continually to normal level. 3.5 matrix metalloproteinase-1(MMP-1) immunohistochemical dyeing MMP-1 positive locates in FB cell. And AOD has the negative correlation with MMP-1 activity. Table 1 dynamic change of ADM Time Normal 1W 2W 3W 4W 8W 16W 24W 26 ±6 242 ±22* 397 ±28* 261 ±23* 133 ±21* 54 ±9* 25 ±5 18 ±3 Ⅰ/Ⅲpercent age 3.02 ±0.35 2.81 ±0.27 2.22 ±0.28* 1.96 ±0.17* 1.85 ±0.23* 2.02 ±0.22* 2.43 ±0.27 2.73 ±0.25 OHPcontent 15.87 ±1.02 16.90 ±1.29 19.32 ±1.37* 21.17 ±1.42* 22.33 ±0.72* 17.11 ±1.19 16.59 ±1.03 15.73 ±1.66 AOD 0.490 ±0.011 0.405* ±0.015 0.380* ±0.019 0.264* ±0.016 0.309* ±0.012 0.465 ±0.013 0.475 ±0.010 0.486 ±0.006 FB 4 Discussions The reconstruction after ADM allografts is mainly collagen metabolism. Fibroblast is the main cell which can synthetize and degrade collagen. The functions of FB are chemotactic migration, proliferation and conversion, etc. ADM contains a lot of arginine- glycine- aspartic acid. And FB can use the integrin receptor lig combine with RGD, and migrate into ADM. This study observed the FB was lack of the ability of migration when ADM was inserted into the skin because the number of the cytoskeleton inhibition of movement and migration are less than the receptors required. And the infiltration of FB couldn’t be seen in the microscope in ADM. So FB change into the type of migration through the temptation of the collagen along the direction of the collagen fiber bundle. The platelet derivation growth factor (PDGF) combines with FB membrane when ADM was implanted 1 week, and mitosis signal which was produced by activation of receptor tyrosine kinase lead to DNA synthesis and FB proliferation. And part of the FB transformed into myofibroblast. And this is because of the collagen contraction, and it will disappear through the cell apoptosis. The amount of FB rose around the ADM, and the gap along the small resistance penetrate to the center, and there were a little of MFB, and there were a lot of new collagen fibers around FB, and the old collagen degrade into small pieces. It will be the peak that FB transforms into MFB after 2 weeks. FB strings the collagen matrix through its pseudopodia and retraction. The cytoplasmic of FB will be stellate because of the diversion of the arrangement of collagen fibers. The structure of collagen fibers will change as the activity between FB and collagen fibers. Its arrangement turned into unidirectional from the diversity. FB cytoplasmic projections gradually showed the dual polarity, and the cell turn the appearance of long spindle. FB regulate the collagen contraction through integrins, and it can promote the cells which be planted migrate into the center of ADM. And the amount of FB increased around ADM in the microscope, and a part of FB turn into MFB, and the new collagen accumulated around ADM, and the old collagen degraded dramatically. A part of FB turned into the mature fiber cells after ADM was implanted 3 weeks, and the MFB enter the cell apoptosis. The amount of FB decreased in the microscope, and the number of the elongated cells increased, especially in the center, and the degradation area of the old collagen reduced. The function of FB was almost end after 4 weeks, and there were not FB in the microscope, and the state of the cells was similar with the fiber cells in the dermis. The state when the time was 8, 16, 24 weeks was similar with 4 weeks. It was complied with the law of wound repair. This study found that the content of OHP and Ⅰ/Ⅲ percentage in ADM was closely related with FB. The number of FB increased within 2 weeks after ADM was implanted. And the amount of FB increased, and the new collagen was synthesized and the old collagen was degraded, and the content of OHP increased, the Ⅰ/Ⅲ percentage reduced. The synthesis of FB declined between 2 and 4 weeks, but the new collagen increased. The activity of degradation was strong, and the content of OHP increased a little, and the Ⅰ/Ⅲ percentage continued to fall. MMP-1 was synthesized with FB, and was the core of Ⅰ and Ⅲ collagen. The activity of MMP-1 had the regularity, and was linked with FB. FB supplied the migration pathways for cells, space for the new collagen more regularity. There were FB, vascular endothelial cells, macrophages, etc. And FB accounted for absolute advantage in them. This study found that the fibroblasts has the main function in the process of decellularized dermal matrix rebuilding through secreting collagen matrix and the synthesis and degradation of ADM collagen controlled by MMP-1. The quantity and the form can guarantee the full reconstruction of ADM and avoid excessive renovation, and maintain the stability of ADM, improve the quality of wound, and make the repaired tissue be close to the original tissue. So we can see that FB has an important function for maximizing the clinical value of ADM. Reference [1] Gaspar K, Erdei I, Peter Z, et al. Role of acellular dermal matrix allograft in minimal invasive coverage of deep burn wound with bone exposed--case report and histological evaluation .International Wound Journal, 2006, 3 (1): 51-8. [2] Sallum EA, Nogueira-Filho GR, Casati MZ, et al. Coronally positioned flap with or without acellular dermal matrix graft in gingival recessions: a histometric study. American Journal of Dentistry, 2006, 19 (2): 128-32. [3] Walter RJ, Matsuda T, Reyse HM, et a1. Characterization of acellular dermal matrices(ADMS) prepared by two different methods[J].Burns.1998,24(2):104~13. [4] Sushunqing, Yuzhi, Zhangyiming. Reaction of Fiber Cell and Extracellular Matrix in Repairing Skin Injury. Chinese Journal of Rrauma, 2000, 16(6):345-6. [5] Prasertsung I, Kanokpanont S, Bunaprasert T, et al. Development of acellular dermis from porcine skin using periodic pressurized technique.J Biomed Mater Res B Appl Biomater. 2008, 85 (1):210-9. [6] Piazuelo E, Lanas A, Jimenez P, et al. In vitro wound repair by human gastric fibroblasts: implications for ulcer healing. Dig Dis Sci, 1998, 43(6):1230-40. 7. Shin D, Minn KW. The effect of myofibroblast on contracture of hypertrophic scar. [J] Plast Reconstr Surg ,2004,113(2):633-64. Figure1 two weeks after ADM was implanted Figure2 eight weeks after ADM was implanted Figure3 sixteen weeks after ADM was implanted